Abstract
Purpose
The study aimed to identify latent classes of demoralization and examine their associations with depression and quality of life (QOL) among patients with cancer.
Methods
Cross-sectional data from 874 patients with cancer from three tertiary hospitals in Fujian province were collected using a convenience sampling method. Demoralization, depression, and QOL were assessed using the Chinese version of the Demoralization Scale-II, Patient Health Questionnaire-9, and McGill Quality of Life Questionnaire. Latent class analysis was performed on demoralization profiles. Binary logistic regression and multiple stepwise linear regression were used to examine the identified classes’ associations with depression and QOL.
Results
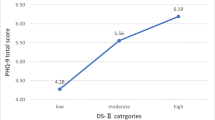
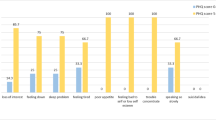
Three latent classes of demoralization were identified: the “low demoralization and emotional disturbance” class (Class 1; 49.6%); “moderate demoralization and meaninglessness” class (Class 2; 29.1%); and “high demoralization and existential despair” class (Class 3; 21.3%). The severity of depression increased and the levels of QOL decreased with the three classes of demoralization. Patients with cancer being depressed in Classes 1 and 2 were 0.128 and 0.018 times that of Class 3, respectively, whereas the magnitudes of decrease in QOL scores for Classes 2 and 3 were 0.378 and 0.629, respectively.
Conclusion
This study revealed three heterogeneous classes of demoralization in Chinese patients with cancer and indicated that increased classes were associated with more severe depression and decreased QOL. Targeted, step-by-step psychological interventions should be developed and implemented according to the characteristics of each class of demoralization to effectively promote psychological well-being among patients with cancer.



Similar content being viewed by others
References
Clarke DM, Kissane DW (2002) Demoralization: its phenomenology and importance. Aust N Z J Psychiatry 36(6):733–742. https://doi.org/10.1046/j.1440-1614.2002.01086.x
Gan LL, Gong S, Kissane DW (2021) Mental state of demoralisation across diverse clinical settings: a systematic review, meta-analysis and proposal for its use as a ‘specifier’in mental illness. Aust N Z J Psychiatry. 00048674211060746. https://doi.org/10.1177/00048674211060746
Hung H, Chen H, Chang Y et al (2010) Evaluation of the reliability and validity of the Mandarin Version of Demoralization Scale for cancer patients. J Intern Med Taiwan 21(6):427–435
Lee C, Fang C, Yang Y et al (2012) Demoralization syndrome among cancer outpatients in Taiwan. Support Care Cancer 20(10):2259–2267. https://doi.org/10.1007/s00520-011-1332-4
Mehnert A, Vehling S, Höcker A, Lehmann C, Koch U (2011) Demoralization and depression in patients with advanced cancer: validation of the German version of the demoralization scale. J Pain Symptom Manage 42(5):768–776. https://doi.org/10.1016/j.jpainsymman.2011.02.013
Wu W, Quan M, Gao L et al (2021) Demoralization and depression in Chinese cancer patients. Support Care Cancer 29(11):6211–6216. https://doi.org/10.1007/s00520-021-06195-9
Mullane M, Dooley B, Tiernan E, Bates U (2009) Validation of the Demoralization Scale in an Irish advanced cancer sample. Palliat Support Care 7(3):323–330. https://doi.org/10.1017/S1478951509990253
Eggen AC, Reyners AK, Shen G et al (2020) Death anxiety in patients with metastatic non-small cell lung cancer with and without brain metastases. J Pain Symptom Manage 60(2):422-429.e421. https://doi.org/10.1016/j.jpainsymman.2020.02.023
Bovero A, Sedghi NA, Opezzo M et al (2018) Dignity-related existential distress in end-of-life cancer patients: prevalence, underlying factors, and associated coping strategies. Psycho-Oncol 27(11):2631–2637. https://doi.org/10.1002/pon.4884
Peng H, Hsueh H, Chang Y, Li R (2021) The mediation and suppression effect of demoralization in breast cancer patients after primary therapy: a structural equation model. J Nurs Res 29(2):e144. https://doi.org/10.1097/JNR.0000000000000421
NikoyKouhpas E, Karimi Z, Rahmani B, Shoaee F (2020) The relationship between existential anxiety and demoralization syndrome in predicting psychological well-being of patient with cancer. Clin Psychol 8(3):175–182. https://doi.org/10.32598/jpcp.8.3.515.1
Ghiggia A, Pierotti V, Tesio V, Bovero A (2021) Personality matters: relationship between personality characteristics, spirituality, demoralization, and perceived quality of life in a sample of end-of-life cancer patients. Support Care Cancer 29(12):7775–7783. https://doi.org/10.1007/s00520-021-06363-x
Kissane DW, Wein S, Love A et al (2004) The Demoralization Scale: a report of its development and preliminary validation. J Palliat Care 20(4):269–276
Fang C, Chang M, Chen P et al (2014) A correlational study of suicidal ideation with psychological distress, depression, and demoralization in patients with cancer. Support Care Cancer 22(12):3165–3174. https://doi.org/10.1007/s00520-014-2290-4
Vehling S, Kissane DW, Lo C et al (2017) The association of demoralization with mental disorders and suicidal ideation in patients with cancer. Cancer 123(17):3394–3401. https://doi.org/10.1002/cncr.30749
Ko KT, Lin CJ, Pi SH, Li YC, Fang CK (2018) Demoralization syndrome among elderly patients with cancer disease. Int J Gerontol 12(1):12–16. https://doi.org/10.1016/j.ijge.2018.01.001
Liu ST, Wu X, Wang N et al (2020) Serial multiple mediation of demoralization and depression in the relationship between hopelessness and suicidal ideation. Psycho-Oncol 29(8):1321–1328. https://doi.org/10.1002/pon.5439
Xu K, Hu DY, Liu YL et al (2019) Relationship of suicidal ideation with demoralization, depression, and anxiety a study of cancer patients in mainland China. J Nerv Ment Dis 207(5):326–332. https://doi.org/10.1097/nmd.0000000000000974
Fava GA, Freyberger HJ, Bech P et al (1995) Diagnostic criteria for use in psychosomatic research. Psychother Psychosom 63(1):1–8. https://doi.org/10.1159/000288931
Robinson S, Kissane DW, Brooker J et al (2016) Refinement and revalidation of the demoralization scale: the DS-II—internal validity. Cancer 122(14):2251–2259. https://doi.org/10.1002/cncr.30015
Hagenaars JA, McCutcheon AL (2002) Applied latent class analysis. Cambridge University Press, Cambridge
Bobevski I, Kissane D, Vehling S et al (2018) Latent class analysis differentiation of adjustment disorder and demoralization, more severe depressive and anxiety disorders, and somatic symptoms in patients with cancer. Psychooncology 27(11):2623–2630. https://doi.org/10.1002/pon.4761
Clarke DM, Kissane DW, Trauer T, Smith GC (2005) Demoralization, anhedonia and grief in patients with severe physical illness. World Psychiatry 4(2):96–105
Von Elm E, Altman DG, Egger M et al (2007) The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement: guidelines for reporting observational studies. Lancet 370(9596):1453–1457. https://doi.org/10.1016/s0140-6736(07)61602-x
Lu J, Li D, Li F et al (2011) Montreal cognitive assessment in detecting cognitive impairment in Chinese elderly individuals: a population-based study. J Geriatr Psychiatry Neurol 24(4):184–190. https://doi.org/10.1177/0891988711422528
Brislin RW (1970) Back-translation for cross-cultural research. J Cross Cult Psychol 1(3):185–216. https://doi.org/10.1177/135910457000100301
Kroenke K, Spitzer RL, Williams JB (2001) The PHQ-9: validity of a brief depression severity measure. J Gen Intern Med 16(9):606–613. https://doi.org/10.1046/j.1525-1497.2001.016009606.x
Wang W, Bian Q, Zhao Y et al (2014) Reliability and validity of the Chinese version of the Patient Health Questionnaire (PHQ-9) in the general population. Gen Hosp Psychiatry 36(5):539–544. https://doi.org/10.1016/j.genhosppsych.2014.05.021
Chilcot J, Rayner L, Lee W et al (2013) The factor structure of the PHQ-9 in palliative care. J Psychosom Res 75(1):60–64. https://doi.org/10.1016/j.jpsychores.2012.12.012
Wang B (2013) A study of the application of PHQ-9 and GAD-7 in malignant tumor population. Dissertation, Central South University.
Cui J, Fang F, Shen F et al (2014) Quality of life in patients with advanced cancer at the end of life as measured by the McGill quality of life questionnaire: a survey in China. J Pain Symptom Manage 48(5):893–902. https://doi.org/10.1016/S0885-3924(02)00593-6
Hu W, Dai Y, Chiu T (2003) Psychometric testing of the translated McGill Quality of Life Questionnaire-Taiwan version in patients with terminal cancer. J Formos Med Assoc 102(2):97–104
Lo RS, Woo J, Zhoc KC et al (2001) Cross-cultural validation of the McGill Quality of Life questionnaire in Hong Kong Chinese. Palliat Med 15(5):387–397. https://doi.org/10.1191/026921601680419438
Celeux G, Soromenho G (1996) An entropy criterion for assessing the number of clusters in a mixture model. J Classif 13(2):195–212. https://doi.org/10.1007/BF01246098
Nylund KL, Asparouhov T, Muthén BO (2007) Deciding on the number of classes in latent class analysis and growth mixture modeling: a Monte Carlo simulation study. Struct Equ Modeling 14(4):535–569. https://doi.org/10.1080/10705510701575396
Cheng J, Chen J, Zhang Y, Kissane D, Yan J (2019) Translation and psychometric properties for the Demoralization Scale in Chinese breast cancer patients. Eur J Oncol Nurs 42:134–140. https://doi.org/10.1016/j.ejon.2019.09.001
Robinson S, Kissane DW, Brooker J et al (2016) Refinement and revalidation of the demoralization scale: the DS-II—external validity. Cancer 122(14):2260–2267. https://doi.org/10.1002/cncr.30012
Mehnert A, Hartung TJ, Friedrich M et al (2018) One in two cancer patients is significantly distressed: prevalence and indicators of distress. Psychooncology 27(1):75–82. https://doi.org/10.1002/pon.4464
Fraguell-Hernando C, Limonero JT, Gil F (2020) Psychological intervention in patients with advanced cancer at home through individual meaning-centered psychotherapy-palliative care: a pilot study. Support Care Cancer 28(10):4803–4811. https://doi.org/10.1007/s00520-020-05322-2
Bovero A, Botto R, Adriano B et al (2019) Exploring demoralization in end-of-life cancer patients: prevalence, latent dimensions, and associations with other psychosocial variables. Palliat Support Care 17(5):596–603. https://doi.org/10.1017/S1478951519000191
Griffith JL, Dsouza A (2012) Demoralization and hope in clinical psychiatry and psychotherapy. The psychotherapy of hope: the legacy of persuasion and healing. The Johns Hopkins University Press, Baltimore, pp 158–177
Nanni MG, Caruso R, Travado L et al (2018) Relationship of demoralization with anxiety, depression, and quality of life: a Southern European study of Italian and Portuguese cancer patients. Psychooncology 27(11):2616–2622. https://doi.org/10.1002/pon.4824
Acknowledgements
We are grateful to the patients who participated in the study.
Funding
This research was supported by the General Project of Fujian Provincial Nature Science Foundation, with grant number [2021J01133126].
Author information
Authors and Affiliations
Contributions
Fefei Huang and Fumei Lin contributed to the study conception and design. Material preparation, data collection and analysis were performed by Fumei Lin, Xiujing Lin, Qingqin Chen, Yu-an Lin and Qiuhong Chen. The first draft of the manuscript was written by Yuting Hong and all authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval
This study was performed in line with the principles of the Declaration of Helsinki. Approval was granted by the Ethics Committee of Fujian Medical University (No: FMU2019012).
Consent to participate
Informed consent was obtained from all individual participants included in the study.
Consent to publish
Not applicable.
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Appendix
Appendix
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Lin, F., Hong, Y., Lin, X. et al. Demoralization profiles and their association with depression and quality of life in Chinese patients with cancer: a latent class analysis. Support Care Cancer 30, 10019–10030 (2022). https://doi.org/10.1007/s00520-022-07412-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00520-022-07412-9