Abstract
Purpose
The impact of pain on functional status and mental health among older adults with cancer is a relevant, yet understudied. We sought to identify the prevalence of pain at diagnosis in older adults with gastrointestinal (GI) malignancies and evaluate the association of pain with functional status limitations, cognition, and mental health.
Methods
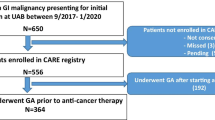
This prospective cross-sectional study included older adults (age ≥ 60) with GI cancers enrolled in the CARE Registry. Pain measured in numeric rating scale from 0 to 10. We utilized the literature based cutoff for moderate-severe as ≥ 4. Logistic regression used to assess differences in functional status, falls, cognitive complaints, and depression/anxiety associated with moderate/severe pain, adjusted for sex, race, education, ethnicity, marital status, cancer type/stage, and treatment phase.
Results
Our cohort included 714 older adults with an average mean age of 70 years and 59% male. Common diagnoses included colorectal (27.9%) and pancreatic (18%). A total of 43.3% reported moderate/severe pain. After multivariate adjusting for covariates, participants with self-reported moderate/severe pain were more likely to report limitations in instrumental activities of daily living (adjusted odds ratio [aOR] 4.3 95% confidence interval [CI] 3.1–6.1, p < .001), limitation in activities of daily living (aOR 3.2 95% CI 2.0–5.1, p < .001), cognitive complaints (aOR 2.9 95% CI 1.4–6.0, p < .004), anxiety (aOR 2.2 95% CI 1.4–3.4, p < 0.01), and depression (aOR 3.7 95% CI 2.2–6.5, p < .001).
Conclusions
Pain is common among older adults with GI cancers and is associated with functional status limitations, cognitive complaints, and depression/anxiety. Strategies to reduce pain and minimize its potential impact on function and mental health warrant future research.

Similar content being viewed by others
Data availability
All data is available per written individual request to University of Alabama at Birmingham (UAB). Code availability: Any software programming code is available per written individual request to UAB.
Code availability
Any software programming code is available per written individual request to University of Alabama at Birmingham (UAB).
References
Smith BD, Smith GL, Hurria A, Hortobagyi GN, Buchholz TA (2009) Future of cancer incidence in the United States: burdens upon an aging, changing nation. J Clin Oncol 27(17):2758–65. https://doi.org/10.1200/JCO.2008.20.8983
Marosi C, Koller M (2016) Challenge of cancer in the elderly. ESMO Open 1(3):e000020. https://doi.org/10.1136/esmoopen-2015-000020
Sawhney R, Sehl M, Naeim A (2005) Physiologic aspects of aging: impact on cancer management and decision making, part I. Cancer J 11(6):449–460
Rocque GB, Williams GR (2019) Bridging the data-free zone: decision making for older adults with cancer journal of clinical oncology: official journal of the American Society of. Clinical Oncology 37(36):3469–71. https://doi.org/10.1200/JCO.19.02588
Williams GR, Mackenzie A, Magnuson A et al (2016) Comorbidity in older adults with cancer. Journal of geriatric oncology 7(4):249–57. https://doi.org/10.1016/j.jgo.2015.12.002
Jacobsen R, Liubarskiene Z, Moldrup C, Christrup L, Sjogren P, Samsanaviciene J (2009) Barriers to cancer pain management: a review of empirical research. Medicina (Kaunas) 45(6):427–433
Rodriguez CS (2001) Pain measurement in the elderly: a review. Pain Manag Nurs. 2(2):38–46. https://doi.org/10.1053/jpmn.2001.23746
Ho K, Spence J, Murphy MF (1996) Review of pain-measurement tools. Ann Emerg Med. 27(4):427–32. https://doi.org/10.1016/s0196-0644(96)70223-8
Glare PA, Davies PS, Finlay E et al (2014) Pain in cancer survivors. J Clin Oncol. 32(16):1739–47. https://doi.org/10.1200/JCO.2013.52.4629
Cella DF, Tulsky DS (1993) Quality of life in cancer: definition, purpose, and method of measurement. Cancer Invest 11(3):327–36. https://doi.org/10.3109/07357909309024860
Thomas E, Peat G, Harris L, Wilkie R, Croft PR (2004) The prevalence of pain and pain interference in a general population of older adults: cross-sectional findings from the North Staffordshire Osteoarthritis Project NorStOP. Pain 110(1–2):361–8. https://doi.org/10.1016/j.pain.2004.04.017
Shega JW, Dale W, Andrew M, Paice J, Rockwood K, Weiner DK (2012) Persistent pain and frailty: a case for homeostenosis. J Am Geriatr Soc 60(1):113–7. https://doi.org/10.1111/j.1532-5415.2011.03769.x
Farrukh N, Hageman L, Chen Y et al (2020) Pain in older survivors of hematologic malignancies after blood or marrow transplantation: a BMTSS report. Cancer 126(9):2003–12. https://doi.org/10.1002/cncr.32736
Kenzik K, Pisu M, Johns SA et al (2015) Unresolved pain interference among colorectal cancer survivors: implications for patient care and outcomes. Pain Med 16(7):1410–25. https://doi.org/10.1111/pme.12727
Persons AGSPoPPiO (2002) The management of persistent pain in older persons. J Am Geriatr Soc. 50(6):205–24. https://doi.org/10.1046/j.1532-5415.50.6s.1.x
Williams GR, Kenzik KM, Parman M et al (2022) Integrating geriatric assessment into routine gastrointestinal (GI) consultation: the cancer and aging resilience evaluation (CARE). J Geriatr Oncol 11(2):270–73. https://doi.org/10.1016/j.jgo.2019.04.008
Hays RD, Bjorner JB, Revicki DA, Spritzer KL, Cella D (2009) Development of physical and mental health summary scores from the patient-reported outcomes measurement information system (PROMIS) global items. Qual Life Res 18(7):873–80. https://doi.org/10.1007/s11136-009-9496-9
Tesler MD, Savedra MC, Holzemer WL, Wilkie DJ, Ward JA, Paul SM (1991) The word-graphic rating scale as a measure of children’s and adolescents’ pain intensity. Res Nurs Health 14(5):361–71. https://doi.org/10.1002/nur.4770140507
Williams GR, Al-Obaidi M, Dai C et al (2021) Fatigue is independently associated with functional status limitations in older adults with gastrointestinal malignancies-results from the CARE registry. Support Care Cancer 29(11):6793–800. https://doi.org/10.1007/s00520-021-06273-y
Williams GR, Al-Obaidi M, Dai C et al (2020) Association of malnutrition with geriatric assessment impairments and health-related quality of life among older adults with gastrointestinal malignancies. Cancer 126(23):5147–55. https://doi.org/10.1002/cncr.33122
Williamson A, Hoggart B (2005) Pain: a review of three commonly used pain rating scales. J Clin Nurs 14(7):798–804. https://doi.org/10.1111/j.1365-2702.2005.01121.x
DuMontier C, Sedrak MS, Soo WK et al (2020) Arti Hurria and the progress in integrating the geriatric assessment into oncology: Young International Society of Geriatric Oncology review paper. J Geriatr Oncol. 11(2):203–11. https://doi.org/10.1016/j.jgo.2019.08.005
Williams GR, Deal AM, Jolly TA et al (2014) Feasibility of geriatric assessment in community oncology clinics. J Geriatr Oncol 5(3):245–51. https://doi.org/10.1016/j.jgo.2014.03.001
Giri S, Al-Obaidi M, Weaver A et al (2021) Association BETWEEN CHRONOLOGIC AGE AND GERIATRIC ASSESSMENT-IDENTIFIED IMPAIRMENTS: FINDINGS FROM The CARE Registry. J Natl Compr Canc Netw. 1-6. https://doi.org/10.6004/jnccn.2020.7679
Fillenbaum GG, Smyer MA (1981) The development, validity, and reliability of the oars multidimensional functional assessment questionnaire1. J Gerontol 36(4):428–34. https://doi.org/10.1093/geronj/36.4.428
Godby RC, Dai C, Al-Obaidi M et al (2021) Depression among older adults with gastrointestinal malignancies. J Geriatr Oncol. 12(4):599–604. https://doi.org/10.1016/j.jgo.2020.10.020
Mir N, MacLennan P, Al-Obaidi M et al (2020) (2020) Patient-reported cognitive complaints in older adults with gastrointestinal malignancies at diagnosis- results from the cancer & aging resilience evaluation (CARE) study. J Geriatr Oncol 11(6):982–88. https://doi.org/10.1016/j.jgo.2020.02.008
Wilford J, Osann K, Hsieh S, Monk B, Nelson E, Wenzel L (2018) Validation of PROMIS emotional distress short form scales for cervical cancer. Gynecologic oncology 151(1):111–16. https://doi.org/10.1016/j.ygyno.2018.07.022
Yost KJ, Eton DT, Garcia SF, Cella D (2011) Minimally important differences were estimated for six patient-reported outcomes measurement information system-cancer scales in advanced-stage cancer patients. J Clin Epidemiol. 64(5):507–16. https://doi.org/10.1016/j.jclinepi.2010.11.018
Cella D, Choi SW, Condon DM et al (2019) PROMIS((R)) Adult health profiles: efficient short-form measures of seven health domains. Value Health. 22(5):537–44. https://doi.org/10.1016/j.jval.2019.02.004
van den Beuken-van Everdingen MH, de Rijke JM, Kessels AG, Schouten HC, van Kleef M, Patijn J (2007) Prevalence of pain in patients with cancer: a systematic review of the past 40 years. Ann Oncol. 18(9):1437–49. https://doi.org/10.1093/annonc/mdm056
Brunello A, Ahcene-Djaballah S, Lettiero A et al (2019) Prevalence of pain in patients with cancer aged 70years or older: a prospective observational study. J Geriatr Oncol. 10(4):637–42. https://doi.org/10.1016/j.jgo.2019.01.005
van den Beuken-van Everdingen MH, Hochstenbach LM, Joosten EA, Tjan-Heijnen VC, Janssen DJ (2016) Update on prevalence of pain in patients with cancer systematic review and meta-analysis. J Pain Symptom Manage. 51(6):1070–90 e9. https://doi.org/10.1016/j.jpainsymman.2015.12.340
Enting RH, Oldenmenger WH, Van Gool AR, van der Rijt CC, SillevisSmitt PA (2007) The effects of analgesic prescription and patient adherence on pain in a dutch outpatient cancer population. J Pain Symptom Manage 34(5):523–31. https://doi.org/10.1016/j.jpainsymman.2007.01.007
Rustoen T, Fossa SD, Skarstein J, Moum T (2003) The impact of demographic and disease-specific variables on pain in cancer patients. J Pain Symptom Manage. 26(2):696–704. https://doi.org/10.1016/s0885-3924(03)00239-2
Lamba N, Mehanna E, Kearney RB et al (2002) Racial disparities in supportive medication use among older patients with brain metastases: a population-based analysis. Neuro Oncol. 22(9):1339–47. https://doi.org/10.1093/neuonc/noaa054
Yeager KA, Williams B, Bai J et al (2019) Factors related to adherence to opioids in black patients with cancer pain. J Pain Symptom Manage. 57(1):28–36. https://doi.org/10.1016/j.jpainsymman.2018.10.491
Jefferson K, Quest T, Yeager KA (2019) Factors associated with black cancer patients’ ability to obtain their opioid prescriptions at the pharmacy. J Palliat Med. 22(9):1143–48. https://doi.org/10.1089/jpm.2018.0536
Giri S, Clark D, Al-Obaidi M et al (2021) Financial distress among older adults with cancer. JCO Oncol Pract. 17(6):e764–e73. https://doi.org/10.1200/OP.20.00601
Connolly D, Garvey J, McKee G (2017) Factors associated with ADL/IADL disability in community dwelling older adults in the Irish longitudinal study on ageing (TILDA). Disabil Rehabil. 39(8):809–16. https://doi.org/10.3109/09638288.2016.1161848
Cwirlej-Sozanska A, Wisniowska-Szurlej A, Wilmowska-Pietruszynska A, Sozanski B (2019) Determinants of ADL and IADL disability in older adults in southeastern Poland. BMC Geriatr. 19(1):297. https://doi.org/10.1186/s12877-019-1319-4
Park J (2019) A study on the sleep quality, pain, and instrumental activities of daily living of outpatients with chronic stroke. J Phys Ther Sci. 31(2):149–52. https://doi.org/10.1589/jpts.31.149
Fried TR, Bradley EH, Towle VR, Allore H (2022) Understanding the treatment preferences of seriously ill patients. The New England J Med 346(14):1061–6. https://doi.org/10.1056/NEJMsa012528
Funding
Supported in part by the National Institutes of Health (K08CA234225 – GW). The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
Author information
Authors and Affiliations
Contributions
All authors contributed to the study conception and design. Material preparation, data collection, and analysis were performed by Grant R. Williams, Mustafa AL-Obaidi, and Sarah Kosmicki, and all authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval
Ethical considerations were presented to and approved by the UAB IRB per review. Study subjects were determined to be exposed to minimal risk.
Consent to participate
All enrolled participants have been consented by IRB-approved study personnel, according to UAB IRB rules and regulations.
Consent for publication.
All authors reviewed and agreed to submission with an intent for publication.
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
AL-Obaidi, M., Kosmicki, S., Harmon, C. et al. Pain among older adults with gastrointestinal malignancies- results from the cancer and aging resilience evaluation (CARE) Registry. Support Care Cancer 30, 9793–9801 (2022). https://doi.org/10.1007/s00520-022-07398-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00520-022-07398-4