Abstract
Purpose
This study aims to investigate the effects of electromyography (EMG) biofeedback on scapular positions and muscle activities during scapular-focused exercises in oral cancer patients with accessory nerve dysfunction.
Methods
Twenty-four participants were randomly allocated to the motor-control with biofeedback group (N = 12) or the motor-control group (N = 12) immediately after neck dissection. Each group performed scapular-focused exercises with conscious control of scapular orientation for 3 months. EMG biofeedback of upper trapezius (UT), middle trapezius (MT), and lower trapezius (LT) was provided in the motor-control with biofeedback group. Scapular symmetry measured by modified lateral scapular slide test; shoulder pain; active range of motion (AROM) of shoulder abduction; upper extremity function; maximal isometric muscle strength of UT, MT, and LT; and muscle activities during arm elevation/lowering in the scapular plane were evaluated at baseline and the end of the intervention.
Results
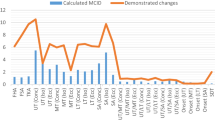
After the 3-month intervention, only the motor-control with biofeedback group showed improving scapular symmetry. Although both groups did not show significant improvement in shoulder pain, increased AROM of shoulder abduction and muscle strength of the UT and MT were observed in both groups. In addition, only the motor-control with biofeedback group had improved LT muscle strength, upper extremity function, and reduced UT and MT muscle activations during arm elevation/lowering.
Conclusions
Early interventions for scapular control training significantly improved shoulder mobility and trapezius muscle strength. Furthermore, by adding EMG biofeedback to motor-control training, oral cancer patients demonstrated greater effectiveness in stabilizing scapular position, muscle efficiency, and upper extremity function than motor-control training alone.
Trial registration
Institutional Review Board: This study was approved by the Chang Gung Medical Foundation Institutional Review Board (Approval No: 201901788A3. Approval Date: 2 January, 2020).
Clinical trial Registration: This trial was registered at ClinicalTrials.gov (ClinicalTrials.gov ID: NCT04476004. Initial released Date: 16 July, 2020).



Similar content being viewed by others
Data availability
Not applicable.
Code availability
Not applicable.
References
Roren A, Fayad F, Poiraudeau S, Fermanian J, Revel M, Dumitrache A et al (2013) Specific scapular kinematic patterns to differentiate two forms of dynamic scapular winging. Clin Biomech (Bristol, Avon) 28(8):941–947. https://doi.org/10.1016/j.clinbiomech.2013.09.003
Camargo PR, Neumann DA (2019) Kinesiologic considerations for targeting activation of scapulothoracic muscles - part 2: trapezius. Braz J Phys Ther 23(6):467–475. https://doi.org/10.1016/j.bjpt.2019.01.011
Tsuji T, Tanuma A, Onitsuka T, Ebihara M, Iida Y, Kimura A et al (2007) Electromyographic findings after different selective neck dissections. Laryngoscope 117(2):319–322. https://doi.org/10.1097/01.mlg.0000249781.20989.5c
Orhan KS, Demirel T, Baslo B, Orhan EK, Yucel EA, Guldiken Y et al (2007) Spinal accessory nerve function after neck dissections. J Laryngol Otol 121(1):44–48. https://doi.org/10.1017/S0022215106002052
Kelley MJ, Kane TE, Leggin BG (2008) Spinal accessory nerve palsy: associated signs and symptoms. J Orthop Sports Phys Ther 38(2):78–86. https://doi.org/10.2519/jospt.2008.2454
Salerno G, Cavaliere M, Foglia A, Pellicoro DP, Mottola G, Nardone M et al (2002) The 11th nerve syndrome in functional neck dissection. Laryngoscope 112(7 Pt 1):1299–1307. https://doi.org/10.1097/00005537-200207000-00029
Chen YH, Lin CR, Liang WA, Huang CY (2020) Motor control integrated into muscle strengthening exercises has more effects on scapular muscle activities and joint range of motion before initiation of radiotherapy in oral cancer survivors with neck dissection: a randomized controlled trial. PLoS One 15(8):e0237133. https://doi.org/10.1371/journal.pone.0237133
Chen YH, Huang CY, Liang WA, Lin CR, Chao YH (2021) Effects of conscious control of scapular orientation in oral cancer survivors with scapular dyskinesis: a randomized controlled trial. Integr Cancer Ther 20:15347354211040828. https://doi.org/10.1177/15347354211040827
Myers JB, Wassinger CA, Lephart SM (2006) Sensorimotor contribution to shoulder stability: effect of injury and rehabilitation. Man Ther 11(3):197–201. https://doi.org/10.1016/j.math.2006.04.002
Lustenhouwer R, Cameron IGM, van Alfen N, Oorsprong TD, Toni I, van Engelen BGM et al (2020) Altered sensorimotor representations after recovery from peripheral nerve damage in neuralgic amyotrophy. Cortex 127:180–190. https://doi.org/10.1016/j.cortex.2020.02.011
Worsley P, Warner M, Mottram S, Gadola S, Veeger HE, Hermens H et al (2013) Motor control retraining exercises for shoulder impingement: effects on function, muscle activation, and biomechanics in young adults. J Shoulder Elbow Surg 22(4):e11–e19. https://doi.org/10.1016/j.jse.2012.06.010
Hotta GH, Santos AL, McQuade KJ, de Oliveira AS (2018) Scapular-focused exercise treatment protocol for shoulder impingement symptoms: three-dimensional scapular kinematics analysis. Clin Biomech (Bristol, Avon) 51:76–81. https://doi.org/10.1016/j.clinbiomech.2017.12.005
Boehm KE, Kondrashov P (2016) Distribution of neuron cell bodies in the intraspinal portion of the spinal accessory nerve in humans. Anat Rec (Hoboken) 299(1):98–102. https://doi.org/10.1002/ar.23279
San Juan JG, Gunderson SR, Kane-Ronning K, Suprak DN (2016) Scapular kinematic is altered after electromyography biofeedback training. J Biomech 49(9):1881–1886. https://doi.org/10.1016/j.jbiomech.2016.04.036
Huang HY, Lin JJ, Guo YL, Wang WT, Chen YJ (2013) EMG biofeedback effectiveness to alter muscle activity pattern and scapular kinematics in subjects with and without shoulder impingement. J Electromyogr Kinesiol 23(1):267–274. https://doi.org/10.1016/j.jelekin.2012.09.007
Dalla Toffola E, Bossi D, Buonocore M, Montomoli C, Petrucci L, Alfonsi E (2005) Usefulness of BFB/EMG in facial palsy rehabilitation. Disabil Rehabil 27(14):809–815. https://doi.org/10.1080/09638280400018650
Sturma A, Hruby LA, Prahm C, Mayer JA, Aszmann OC (2018) Rehabilitation of upper extremity nerve injuries using surface EMG biofeedback: protocols for clinical application. Front Neurosci 12:906. https://doi.org/10.3389/fnins.2018.00906
Uhl TL, Kibler WB, Gecewich B, Tripp BL (2009) Evaluation of clinical assessment methods for scapular dyskinesis. Arthroscopy 25(11):1240–1248. https://doi.org/10.1016/j.arthro.2009.06.007
Kibler WB (1998) The role of the scapula in athletic shoulder function. Am J Sports Med 26(2):325–337. https://doi.org/10.1177/03635465980260022801
Shadmehr A, Sarafraz H, Heidari Blooki M, Jalaie SH, Morais N (2016) Reliability, agreement, and diagnostic accuracy of the Modified Lateral Scapular Slide test. Man Ther 24:18–24. https://doi.org/10.1016/j.math.2016.04.004
McGarvey AC, Osmotherly PG, Hoffman GR, Chiarelli PE (2013) Scapular muscle exercises following neck dissection surgery for head and neck cancer: a comparative electromyographic study. Phys Ther 93(6):786–797. https://doi.org/10.2522/ptj.20120385
De Mey K, Danneels LA, Cagnie B, Huyghe L, Seyns E, Cools AM (2013) Conscious correction of scapular orientation in overhead athletes performing selected shoulder rehabilitation exercises: the effect on trapezius muscle activation measured by surface electromyography. J Orthop Sports Phys Ther 43(1):3–10. https://doi.org/10.2519/jospt.2013.4283
Mottram SL, Woledge RC, Morrissey D (2009) Motion analysis study of a scapular orientation exercise and subjects’ ability to learn the exercise. Man Ther 14(1):13–18. https://doi.org/10.1016/j.math.2007.07.008
Norkin CC, White DJ (2016) Measurement of joint motion: a guide to goniometry. F.A. Davis, Philadelphia
Muir SW, Corea CL, Beaupre L (2010) Evaluating change in clinical status: reliability and measures of agreement for the assessment of glenohumeral range of motion. N Am J Sports Phys Ther 5(3):98–110
Hawker GA, Mian S, Kendzerska T, French M (2011) Measures of adult pain: Visual Analog Scale for Pain (VAS Pain), Numeric Rating Scale for Pain (NRS Pain), McGill Pain Questionnaire (MPQ), Short-Form McGill Pain Questionnaire (SF-MPQ), Chronic Pain Grade Scale (CPGS), Short Form-36 Bodily Pain Scale (SF-36 BPS), and Measure of Intermittent and Constant Osteoarthritis Pain (ICOAP). Arthritis Care Res (Hoboken) 63(Suppl 11):S240–S252. https://doi.org/10.1002/acr.20543
Hao Q, Devji T, Zeraatkar D, Wang Y, Qasim A, Siemieniuk RAC et al (2019) Minimal important differences for improvement in shoulder condition patient-reported outcomes: a systematic review to inform a BMJ Rapid Recommendation. BMJ Open 9(2):e028777. https://doi.org/10.1136/bmjopen-2018-028777
Liang HW, Wang HK, Yao G, Horng YS, Hou SM (2004) Psychometric evaluation of the Taiwan version of the Disability of the Arm, Shoulder, and Hand (DASH) questionnaire. J Formos Med Assoc 103(10):773–779
Goldstein DP, Ringash J, Irish JC, Gilbert R, Gullane P, Brown D et al (2015) Assessment of the Disabilities of the Arm, Shoulder, and Hand (DASH) questionnaire for use in patients after neck dissection for head and neck cancer. Head Neck 37(2):234–242. https://doi.org/10.1002/hed.23593
Franchignoni F, Vercelli S, Giordano A, Sartorio F, Bravini E, Ferriero G (2014) Minimal clinically important difference of the disabilities of the arm, shoulder and hand outcome measure (DASH) and its shortened version (QuickDASH). J Orthop Sports Phys Ther 44(1):30–39. https://doi.org/10.2519/jospt.2014.4893
Ekstrom RA, Soderberg GL, Donatelli RA (2005) Normalization procedures using maximum voluntary isometric contractions for the serratus anterior and trapezius muscles during surface EMG analysis. J Electromyogr Kinesiol 15(4):418–428. https://doi.org/10.1016/j.jelekin.2004.09.006
Hayes K, Walton JR, Szomor ZL, Murrell GA (2002) Reliability of 3 methods for assessing shoulder strength. J Shoulder Elbow Surg 11(1):33–39. https://doi.org/10.1067/mse.2002.119852
Michener LA, Boardman ND, Pidcoe PE, Frith AM (2005) Scapular muscle tests in subjects with shoulder pain and functional loss: reliability and construct validity. Phys Ther 85(11):1128–1138
Birhanu T, Molenberghs G, Sotto C, Kenward MG (2011) Doubly robust and multiple-imputation-based generalized estimating equations. J Biopharm Stat 21(2):202–225. https://doi.org/10.1080/10543406.2011.550096
Ma Y, Mazumdar M, Memtsoudis SG (2012) Beyond repeated-measures analysis of variance: advanced statistical methods for the analysis of longitudinal data in anesthesia research. Reg Anesth Pain Med 37(1):99–105. https://doi.org/10.1097/AAP.0b013e31823ebc74
Sigrist R, Rauter G, Riener R, Wolf P (2013) Augmented visual, auditory, haptic, and multimodal feedback in motor learning: a review. Psychon Bull Rev 20(1):21–53. https://doi.org/10.3758/s13423-012-0333-8
Duarte-Moreira RJ, Castro KV, Luz-Santos C, Martins JVP, Sa KN, Baptista AF (2018) Electromyographic biofeedback in motor function recovery after peripheral nerve injury: an integrative review of the literature. Appl Psychophysiol Biofeedback 43(4):247–257. https://doi.org/10.1007/s10484-018-9403-7
Moezy A, Sepehrifar S, Solaymani DM (2014) The effects of scapular stabilization based exercise therapy on pain, posture, flexibility and shoulder mobility in patients with shoulder impingement syndrome: a controlled randomized clinical trial. Med J Islam Repub Iran 28:87
Gane EM, McPhail SM, Hatton AL, Panizza BJ, O’Leary SP (2018) The relationship between physical impairments, quality of life and disability of the neck and upper limb in patients following neck dissection. J Cancer Surviv 12(5):619–631. https://doi.org/10.1007/s11764-018-0697-5
Herman DC, Onate JA, Weinhold PS, Guskiewicz KM, Garrett WE, Yu B et al (2009) The effects of feedback with and without strength training on lower extremity biomechanics. Am J Sports Med 37(7):1301–1308. https://doi.org/10.1177/0363546509332253
Holtermann A, Roeleveld K, Mork PJ, Gronlund C, Karlsson JS, Andersen LL et al (2009) Selective activation of neuromuscular compartments within the human trapezius muscle. J Electromyogr Kinesiol 19(5):896–902. https://doi.org/10.1016/j.jelekin.2008.04.016
Sale DG (1988) Neural adaptation to resistance training. Med Sci Sports Exerc 20(5 Suppl):S135–S145. https://doi.org/10.1249/00005768-198810001-00009
Hickey D, Solvig V, Cavalheri V, Harrold M, McKenna L (2018) Scapular dyskinesis increases the risk of future shoulder pain by 43% in asymptomatic athletes: a systematic review and meta-analysis. Br J Sports Med 52(2):102–110. https://doi.org/10.1136/bjsports-2017-097559
Gane EM, Michaleff ZA, Cottrell MA, McPhail SM, Hatton AL, Panizza BJ et al (2017) Prevalence, incidence, and risk factors for shoulder and neck dysfunction after neck dissection: a systematic review. Eur J Surg Oncol 43(7):1199–1218. https://doi.org/10.1016/j.ejso.2016.10.026
Cardoso LR, Rizzo CC, de Oliveira CZ, dos Santos CR, Carvalho AL (2015) Myofascial pain syndrome after head and neck cancer treatment: Prevalence, risk factors, and influence on quality of life. Head Neck 37(12):1733–1737. https://doi.org/10.1002/hed.23825
Acknowledgements
The authors thank for the statistical assistance and acknowledge the support of the Maintenance Project of the Center for Big Data Analytics and Statistics (Grant CLRPG3D0048) at Chang Gung Memorial Hospital for statistical consultation and data analysis.
Author information
Authors and Affiliations
Contributions
Yueh-Hsia Chen and Cheng-Ya Huang contributed to the study conception and design. Data collection and analysis were performed by Yueh-Hsia Chen. Wei-An Liang and Chi-Rung Lin assisted in intervention protocols. The first draft of the manuscript was written by Yueh-Hsia Chen, and Cheng-Ya Huang commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
This study was performed in line with the principles of the Declaration of Helsinki. Approval was granted by the Chang Gung Medical Foundation Institutional Review Board (Date: 2 January, 2020/No: 201901788A3) and Clinical Trials (Date: 16 July, 2020/No: NCT04476004). Informed consent was obtained from all individual participants included in the study.
Consent for publication
Not applicable.
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Chen, YH., Liang, WA., Lin, CR. et al. A randomized controlled trial of scapular exercises with electromyography biofeedback in oral cancer patients with accessory nerve dysfunction. Support Care Cancer 30, 8241–8250 (2022). https://doi.org/10.1007/s00520-022-07263-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00520-022-07263-4