Abstract
Purpose
There has been little research on the healthcare cost-related coping mechanisms of families of patients with cancer. Therefore, we assessed the association between a cancer diagnosis and the healthcare cost-related coping mechanisms of participant family members through their decision to forego or delay seeking medical care, one of the manifestations of financial toxicity.
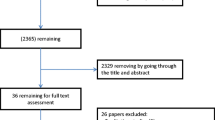
Methods
Using data from the National Health Interview Survey (NHIS) between 2000 and 2018, sample weight-adjusted prevalence was calculated and multivariable logistic regressions defined adjusted odds ratios (aORs) for participant family members who needed but did not get medical care or who delayed seeking medical care due to cost in the past 12 months, adjusting for relevant sociodemographic covariates, including participant history of cancer (yes vs. no) and participant age (18–45 vs. 46–64 years old). The analysis of family members foregoing or delaying medical care was repeated using a cancer diagnosis * age interaction term.
Results
Participants with cancer were more likely than those without a history of cancer to report family members delaying (19.63% vs. 16.31%, P < 0.001) or foregoing (14.53% vs. 12.35%, P = 0.001) medical care. Participants with cancer in the 18 to 45 years old age range were more likely to report family members delaying (pinteraction = 0.028) or foregoing (pinteraction < 0.001) medical care. Other factors associated with cost-related coping mechanisms undertaken by the participants’ family members included female sex, non-married status, poorer health status, lack of health insurance coverage, and lower household income.
Conclusion
A cancer diagnosis may be associated with familial healthcare cost-related coping mechanisms, one of the manifestations of financial toxicity. This is seen through delayed/omitted medical care of family members of people with a history of cancer, an association that may be stronger among young adult cancer survivors. These findings underscore the need to further explore how financial toxicity associated with a cancer diagnosis can affect patients’ family members and to design interventions to mitigate healthcare cost-related coping mechanisms.

Similar content being viewed by others
Data sharing statement
The data is publicly available via IPUMS (https://www.ipums.org/).
Code availability
Not applicable.
References
Mariotto AB, Yabroff KR, Shao Y, Feuer EJ, Brown ML (2011) Projections of the cost of cancer care in the United States: 2010–2020. J Natl Cancer Inst 103(2):117–128
Bernard DS, Farr SL, Fang Z (2011) National estimates of out-of-pocket health care expenditure burdens among nonelderly adults with cancer: 2001 to 2008. J Clin Oncol 29(20):2821–2826
Davidoff AJ, Erten M, Shaffer T et al (2013) Out-of-pocket health care expenditure burden for Medicare beneficiaries with cancer. Cancer 119(6):1257–1265
Yabroff KR, Dowling EC, Guy GP Jr et al (2016) Financial hardship associated with cancer in the United States: findings from a population-based sample of adult cancer survivors. J Clin Oncol 34(3):259–267
Financial Toxicity (Financial Distress) and Cancer Treatment (PDQ®)–patient version (2019) https://www.cancer.gov/about-cancer/managing-care/track-care-costs/financial-toxicity-pdq
Zafar SY, Peppercorn JM, Schrag D et al (2013) The financial toxicity of cancer treatment: a pilot study assessing out-of-pocket expenses and the insured cancer patient’s experience. Oncologist 18(4):381–390
Oshima SM, Tait SD, Rushing C et al (2021) Patient perspectives on the financial costs and burdens of breast cancer surgery. JCO Oncol Pract 17(6):e872–e881
Watabayashi K, Steelquist J, Overstreet KA et al (2020) A pilot study of a comprehensive financial navigation program in patients with cancer and caregivers. J Natl Compr Canc Netw 18(10):1366–1373
Guy GP Jr, Ekwueme DU, Yabroff KR et al (2013) Economic burden of cancer survivorship among adults in the United States. J Clin Oncol 31(30):3749–3757
Ramsey S, Blough D, Kirchhoff A et al (2013) Washington State cancer patients found to be at greater risk for bankruptcy than people without a cancer diagnosis. Health Aff (Millwood) 32(6):1143–1152
Ell K, Xie B, Wells A, Nedjat-Haiem F, Lee PJ, Vourlekis B (2008) Economic stress among low-income women with cancer: effects on quality of life. Cancer 112(3):616–625
Lathan CS, Cronin A, Tucker-Seeley R, Zafar SY, Ayanian JZ, Schrag D (2016) Association of financial strain with symptom burden and quality of life for patients with lung or colorectal cancer. J Clin Oncol 34(15):1732–1740
Knight TG, Deal AM, Dusetzina SB, et al. (2018) Financial toxicity in adults with cancer: adverse outcomes and noncompliance. J Oncol Pract : JOP1800120.
Zhao J, Zheng Z, Han X et al (2019) Cancer history, health insurance coverage, and cost-related medication nonadherence and medication cost-coping strategies in the United States. Value Health 22(7):762–767
Bestvina CM, Zullig LL, Rushing C et al (2014) Patient-oncologist cost communication, financial distress, and medication adherence. J Oncol Pract 10(3):162–167
Dusetzina SB, Winn AN, Abel GA, Huskamp HA, Keating NL (2014) Cost sharing and adherence to tyrosine kinase inhibitors for patients with chronic myeloid leukemia. J Clin Oncol 32(4):306–311
Neugut AI, Subar M, Wilde ET et al (2011) Association between prescription co-payment amount and compliance with adjuvant hormonal therapy in women with early-stage breast cancer. J Clin Oncol 29(18):2534–2542
Richard P, Patel N, Lu YC, Walker R, Younis M. The financial burden of cancer on families in the United States. Int J Environ Res Public Health 2021; 18(7).
Kelada L, Wakefield CE, Vetsch J et al (2020) Financial toxicity of childhood cancer and changes to parents’ employment after treatment completion. Pediatr Blood Cancer 67(7):e28345
Veenstra CM, Wallner LP, Jagsi R et al (2017) Long-term economic and employment outcomes among partners of women with early-stage breast cancer. J Oncol Pract 13(11):e916–e926
Grunfeld E, Coyle D, Whelan T et al (2004) Family caregiver burden: results of a longitudinal study of breast cancer patients and their principal caregivers. CMAJ 170(12):1795–1801
Nipp RD, Shui AM, Perez GK et al (2018) Patterns in health care access and affordability among cancer survivors during implementation of the affordable care act. JAMA Oncol 4(6):791–797
Snyder RA, Chang GJ (2019) Financial toxicity: a growing burden for cancer patients. ACS Bulletin. https://bulletin.facs.org/2019/09/financial-toxicity-a-growing-burden-for-cancer-patients. Accessed 9 Aug 2021
Centers for Disease Control and Prevention. National health interview survey: methods. https://www.cdc.gov/nchs/nhis/index.htm. Accessed 7 Aug 2021
Ruggles S FS, Goeken R, et al. Integrated public use microdata series USA: version 9.0 . University of Minnesota; 2019. Accessed August 31, 2020. Available at: https://doi.org/10.18128/D010.V9.0.
Sanford NN, Lam MB, Butler SS et al (2019) Self-reported reasons and patterns of noninsurance among cancer survivors before and after implementation of the affordable care act, 2000–2017. JAMA Oncol 5(10):e191973
Gonzales F, Zheng Z, Yabroff KR (2018) Trends in financial access to prescription drugs among cancer survivors. J Natl Cancer Inst 110(2):216–219. https://doi.org/10.1093/jnci/djx164
Yabroff KR, Lawrence WF, Clauser S, Davis WW, Brown ML (2004) Burden of illness in cancer survivors: findings from a population-based national sample. J Natl Cancer Inst 96(17):1322–1330
Cohee AA, Adams RN, Johns SA et al (2017) Long-term fear of recurrence in young breast cancer survivors and partners. Psychooncology 26(1):22–28
Ares I, Lebel S, Bielajew C (2014) The impact of motherhood on perceived stress, illness intrusiveness and fear of cancer recurrence in young breast cancer survivors over time. Psychol Health 29(6):651–670
MacKinney EC, Kuchta KM, Winchester DJ et al (2022) Overall survival is improved with total thyroidectomy and radiation for male patients and patients older than 55 with T2N0M0 stage 1 classic papillary thyroid cancer. Surgery 171(1):197–202
Muzzatti B, Bomben F, Flaiban C, Piccinin M, Annunziata MA (2020) Quality of life and psychological distress during cancer: a prospective observational study involving young breast cancer female patients. BMC Cancer 20(1):758
Ziner KW, Sledge GW, Bell CJ, Johns S, Miller KD, Champion VL (2012) Predicting fear of breast cancer recurrence and self-efficacy in survivors by age at diagnosis. Oncol Nurs Forum 39(3):287–295
Zheng Z, Jemal A, Han X et al (2019) Medical financial hardship among cancer survivors in the United States. Cancer 125(10):1737–1747
Dee EC, Nipp RD, Muralidhar V, Yu Z, Butler SS, Mahal BA, Nguyen PL, Sanford NN (2021) Financial worry and psychological distress among cancer survivors in the United States, 2013-2018. Support Care Cancer 29(9):5523–5535. https://doi.org/10.1007/s00520-021-06084-1
DeSantis CE, Lin CC, Mariotto AB et al (2014) Cancer treatment and survivorship statistics, 2014. CA Cancer J Clin 64(4):252–271
Fenn KM, Evans SB, McCorkle R et al (2014) Impact of financial burden of cancer on survivors’ quality of life. J Oncol Pract 10(5):332–338
Bradley CJ, Given CW, Roberts C (2001) Disparities in cancer diagnosis and survival. Cancer 91(1):178–188
Dee EC, Arega MA, Yang DD et al (2021) Disparities in refusal of locoregional treatment for prostate adenocarcinoma. JCO Oncol Pract 17(10):e1489–e1501
Jain B, Bajaj SS, Paguio JA et al (2022) Socioeconomic disparities in healthcare utilization for atherosclerotic cardiovascular disease. Am Heart J 246:161–165
Zavala VA, Bracci PM, Carethers JM et al (2021) Cancer health disparities in racial/ethnic minorities in the United States. Br J Cancer 124(2):315–332
Politi MC, Yen RW, Elwyn G et al (2021) Women who are young, non-white, and with lower socioeconomic status report higher financial toxicity up to 1 year after breast cancer surgery: a mixed-effects regression analysis. Oncologist 26(1):e142–e152
Altice CK, Banegas MP, Tucker-Seeley RD, Yabroff KR (2017) Financial hardships experienced by cancer survivors: a systematic review. J Natl Cancer Inst 109(2).
Smith GL, Lopez-Olivo MA, Advani PG et al (2019) Financial burdens of cancer treatment: a systematic review of risk factors and outcomes. J Natl Compr Canc Netw 17(10):1184–1192
Bekelman JE, Halpern SD, Blankart CR et al (2016) Comparison of site of death, health care utilization, and hospital expenditures for patients dying with cancer in 7 developed countries. JAMA 315(3):272–283
Sarfati D, Koczwara B, Jackson C (2016) The impact of comorbidity on cancer and its treatment. CA Cancer J Clin 66(4):337–350
Krieger N, Wright E, Chen JT, Waterman PD, Huntley ER, Arcaya M (2020) Cancer stage at diagnosis, historical redlining, and current neighborhood characteristics: breast, cervical, lung, and colorectal cancers, Massachusetts, 2001–2015. Am J Epidemiol 189(10):1065–1075
Mujahid MS, Gao X, Tabb LP, Morris C, Lewis TT. (2021) Historical redlining and cardiovascular health: the multi-ethnic study of atherosclerosis. Proc Natl Acad Sci U S A 118(51).
Barnes JM, Johnson KJ, Boakye EA, Schapira L, Akinyemiju T, Park EM, Graboyes EM, Osazuwa-Peters N (2021) Early medicaid expansion and cancer mortality. J Natl Cancer Inst 113(12):1714–1722. https://doi.org/10.1093/jnci/djab135
Lee G, Dee EC, Orav EJ et al (2021) Association of Medicaid expansion and insurance status, cancer stage, treatment and mortality among patients with cervical cancer. Cancer Rep (Hoboken) 4(6):e1407
Takvorian SU, Oganisian A, Mamtani R et al (2020) Association of Medicaid expansion under the affordable care act with insurance status, cancer stage, and timely treatment among patients with breast, colon, and lung cancer. JAMA Netw Open 3(2):e1921653
Banegas MP, Yabroff KR, O’Keeffe-Rosetti MC et al (2018) Medical care costs associated with cancer in integrated delivery systems. J Natl Compr Canc Netw 16(4):402–410
Sadigh G, Switchenko J, Weaver KE, Elchoufi D, Meisel J, Bilen MA, Lawson D, Cella D, El-Rayes B, Carlos R (2022) Correlates of financial toxicity in adult cancer patients and their informal caregivers. Support Care Cancer 30(1):217–225. https://doi.org/10.1007/s00520-021-06424-1
Khera N, Sugalski J, Krause D et al (2020) Current practices for screening and management of financial distress at NCCN member institutions. J Natl Compr Canc Netw 18(7):825–831
de Souza JA, Yap BJ, Wroblewski K et al (2017) Measuring financial toxicity as a clinically relevant patient-reported outcome: the validation of the COmprehensive Score for financial Toxicity (COST). Cancer 123(3):476–484
Dar MA, Chauhan R, Murti K, Trivedi V, Dhingra S (2021) Development and validation of subjective financial distress questionnaire (SFDQ): a patient reported outcome measure for assessment of financial toxicity among radiation oncology patients. Front Oncol 11:819313
Wheeler SB, Rodriguez-O'Donnell J, Rogers C, Fulcher J, Deal A, Manning ML, Gellin M, Padilla N, Rosenstein DL (2020) Reducing cancer-related financial toxicity through financial navigation: Results from a pilot intervention. Cancer Epidemiol Biomarkers Prev 29(3):694. https://doi.org/10.1158/1055-9965.EPI-20-0067
Cubanski J, Neuman T, Freed M (2021) What’s the Latest on Medicare Drug Price Negotiations? KFF. https://www.kff.org/medicare/issue-brief/whats-the-latest-on-medicare-drug-price-negotiations/. Accessed 9 Aug 2021
Stabile M, Thomson S, Allin S et al (2013) Health care cost containment strategies used in four other high-income countries hold lessons for the United States. Health Aff (Millwood) 32(4):643–652
Lentz R, Benson AB 3rd, Kircher S (2019) Financial toxicity in cancer care: prevalence, causes, consequences, and reduction strategies. J Surg Oncol 120(1):85–92
Bach PB, Saltz LB, Witttes RE (2012) In Cancer care, cost matters. The New York Times. https://www.nytimes.com/2012/10/15/opinion/a-hospital-says-no-to-an-11000-a-month-cancer-drug.html. Accessed 3 Aug 2021
Pollack A (2012) Sanofi halves price of cancer drug Zaltrap after Sloan-Kettering rejection. The New York Times. https://www.nytimes.com/2012/11/09/business/sanofi-halves-price-of-drug-after-sloan-kettering-balks-at-paying-it.html. Accessed 25 Jul 2021
Funding
Funding grant number R01-CA240582 (PLN), NIH/NCI Cancer Center Support Grant P30 CA008748 (FC and ECD).
Author information
Authors and Affiliations
Contributions
Study concept and design: ECD, BK. Data analysis and interpretation: ECD, FC, BK, NNS. Manuscript preparation: ECD, NNS, BK, FC. Critical revision: All authors.
Corresponding authors
Ethics declarations
Ethics approval
IRB review exempt due to publicly available data.
Consent to participate
Only publicly available, de-identified data were used.
Consent for publication
Only publicly available, de-identified data were used.
Conflict of interest
Author BAM received funding from the Prostate Cancer Foundation and (PCF), the American Society for Radiation Oncology (ASTRO), the Department of Defense, and the Sylvester Comprehensive Cancer Center outside the submitted work. Author PLN received grants and personal fees from Bayer, Janssen, and Astellas and personal fees from Boston Scientific, Dendreon, Ferring, COTA, Blue Earth Diagnostics, Myovant Sciences, and Augmenix outside the submitted work. Author VM received a grant from the Conquer Cancer Foundation outside the submitted work. The remaining authors declare they have no financial interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Nina N. Sanford and Edward Christopher Dee contributed as co-senior authors.
Rights and permissions
About this article
Cite this article
Kazzi, B., Chino, F., Kazzi, B. et al. Shared burden: the association between cancer diagnosis, financial toxicity, and healthcare cost-related coping mechanisms by family members of non-elderly patients in the USA. Support Care Cancer 30, 8905–8917 (2022). https://doi.org/10.1007/s00520-022-07234-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00520-022-07234-9