Abstract
Purpose
Previous evidence regarding the impact of exercise interventions on chemotherapy-induced peripheral neuropathy often focuses on lower-extremity functions, such as muscle strength and balance ability, while their effects on upper extremities remain unknown. We aimed to evaluate the efficacy of combined hand exercise intervention on upper-extremity function, symptoms, and quality-of-life in patients with chemotherapy-induced peripheral neuropathy (CIPN).
Methods
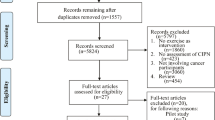
After screening 341 patients, 42 were randomly assigned to either the intervention (n = 21) or control (n = 21) group. Participants were evaluated at baseline (T0) and after one (T1) and two (T2) chemotherapy cycles. The primary outcome was upper-extremity function measured using the Michigan Hand Outcomes Questionnaire (MHQ) at T2. The intention-to-treat and as-treated populations were compared using a mixed-effect model.
Results
In the intention-to-treat analysis, the decline in activities of daily living of MHQ was significantly suppressed in the intervention group compared with that in the control group at T2 (difference: 7.23; 95% confidence interval: 0.35–14.10). Similarly, in the as-treated analysis, the decline in activities of daily living of MHQ was significantly suppressed in the intervention group compared with that in the control group at T2 (difference: 13.09; 95% confidence interval: 5.68–20.49). Pain also significantly improved in the intervention group compared with that in the control group at T2 (difference: 13.21; 95% confidence interval: − 22.91 to − 3.51).
Conclusion
The combined hand exercise intervention may improve upper-extremity function, such as by suppressing decline in ADL, and reduce pain in patients with CIPN.


Similar content being viewed by others
Data availability
Not applicable.
Code availability
Not applicable.
Change history
12 March 2022
A Correction to this paper has been published: https://doi.org/10.1007/s00520-022-06946-2
References
Bakitas MA (2007) Background noise: the experience of chemotherapy-induced peripheral neuropathy. Nurs Res 56:323–331. https://doi.org/10.1097/01.NNR.0000289503.22414.79
Speck RM, DeMichele A, Farrar JT, Hennessy S, Mao JJ, Stineman MG, Barg FK (2012) Scope of symptoms and self-management strategies for chemotherapy-induced peripheral neuropathy in breast cancer patients. Support Care Cancer 20:2433–2439. https://doi.org/10.1007/s00520-011-1365-8
Oh PJ, Lee JR, Kim SK, Kim JH (2020) Changes in chemotherapy-induced peripheral neuropathy, disturbance in activities of daily living, and depression following chemotherapy in patients with colorectal cancer: a prospective study. Eur J Oncol Nurs 44:101676. https://doi.org/10.1016/j.ejon.2019.101676
Mols F, Beijers T, Lemmens V, Hurk CJ, Vreugdenhil G, Franse LVP (2012) Chemotherapy-induced neuropathy and its association with quality of life among 2- to 11-year colorectal cancer survivors: results from the population-based PROFILES registry. J Clin Oncol 31:2699–2707. https://doi.org/10.1200/JCO.2013.49.1514
Eckhoff L, Knoop A, Jensen MB, Ewertz M (2015) Persistence of docetaxel-induced neuropathy and impact on quality of life among breast cancer survivors. Eur J Cancer 51:292–300. https://doi.org/10.1016/j.ejca.2014.11.024
Ezendam NPM, Pijlman B, Bhugwandass C, Pruijt JFM, Mols F, Vos MC, Pijnenborg JM, van de Poll-Franse LV (2014) Chemotherapy-induced peripheral neuropathy and its impact on health-related quality of life among ovarian cancer survivors: results from the population-based PROFILES registry. Gynecol Oncol 135:510–517. https://doi.org/10.1016/j.ygyno.2014.09.016
Grisold W, Cavaletti G, Windebank AJ (2012) Peripheral neuropathies from chemotherapeutics and targeted agents: diagnosis, treatment, and prevention. Neuro Oncol 14:iv45–iv54. https://doi.org/10.1093/neuonc/nos203
Seretny M, Currie GL, Sena ES, Ramnarine S, Grant R, MacLeod MR, Colvin LA, Fallon M (2014) Incidence, prevalence, and predictors of chemotherapy-induced peripheral neuropathy: a systematic review and meta-analysis. Pain 155:2461–2470. https://doi.org/10.1016/j.pain.2014.09.020
Loprinzi CL, Lacchetti C, Bleeker J, Cavaletti G, Chauhan C, Hertz DL, Kelley MR, Lavino A, Lustberg MB, Paice JA, Schneider BP, Lavoie Smith EM, Smith ML, Smith TJ, Wagner-Johnston N, Hershman DL (2020) Prevention and management of chemotherapy-induced peripheral neuropathy in survivors of adult cancers: ASCO guideline update. J Clin Oncol 38:3325–3348. https://doi.org/10.1200/JCO.20.01399
Prinsloo S, Novy D, Driver L, Lyle R, Ramondetta L, Eng C, McQuade J, Lopez G, Cohen L (2017) Randomized controlled trial of neurofeedback on chemotherapy-induced peripheral neuropathy: a pilot study. Cancer 123:1989–1997. https://doi.org/10.1002/cncr.30649
Kleckner IR, Kamen C, Gewandter JS, Mohile NA, Heckler CE, Culakova E, Fung C, Janelsins MC, Asare M, Lin PJ, Reddy PS, Giguere J, Berenberg J, Kesler SR, Mustian KM (2018) Effects of exercise during chemotherapy on chemotherapy-induced peripheral neuropathy: a multicenter, randomized controlled trial. Support Care Cancer 26:1019–1028. https://doi.org/10.1007/s00520-017-4013-0
Zimmer P, Trebing S, Timmers-Trebing U, Schenk A, Paust R, Bloch W, Rudolph R, Streckmann F, Baumann FT (2018) Eight-week, multimodal exercise counteracts a progress of chemotherapy-induced peripheral neuropathy and improves balance and strength in metastasized colorectal cancer patients: a randomized controlled trial. Support Care Cancer 26:615–624. https://doi.org/10.1007/s00520-017-3875-5
Streckmann F, Kneis S, Leifert JA, Baumann FT, Kleber M, Ihorst G, Herich L, Grüssinger V, Gollhofer A, Bertz H (2014) Exercise program improves therapy-related side-effects and quality of life in lymphoma patients undergoing therapy. Ann Oncol 25:493–499. https://doi.org/10.1093/annonc/mdt568
Vollmers PL, Mundhenke C, Maass N, Bauerschlag D, Kratzenstein S, Röcken C, Schmidt T (2018) Evaluation of the effects of sensorimotor exercise on physical and psychological parameters in breast cancer patients undergoing neurotoxic chemotherapy. J Cancer Res Clin Oncol 144:1785–1792. https://doi.org/10.1007/s00432-018-2686-5
Chung KC, Pillsbury MS, Walters MR, Hayward RA (1998) Reliability and validity testing of the Michigan Hand Outcomes Questionnaire. J Hand Surg Am 23:575–587. https://doi.org/10.1016/S0363-5023(98)80042-7
Oda T, Abe Y, Katsumi Y, Ohi H, Nakamura T, Inagaki K (2016) Reliability and validity of the Japanese version of the Michigan hand outcomes questionnaire: a comparison with the DASH and SF-36 questionnaires. J Hand Surg Asian Pac 21:72–77. https://doi.org/10.1142/S2424835516500119
Bell-Krotoski J, Tomancik E (1987) The repeatability of testing with Semmes-Weinstein monofilaments. J Hand Surg Am 12:155–161. https://doi.org/10.1016/s0363-5023(87)80189-2
Tiffin J, Asher EJ (1948) The Purdue pegboard; norms and studies of reliability and validity. J Appl Psychol 32:234–247. https://doi.org/10.1037/h0061266
Calhoun EA, Welshman EE, Chang CH, Lurain JR, Fishman DA, Hunt TL, Cella D (2003) Psychometric evaluation of the Functional Assessment of Cancer Therapy/Gynecologic Oncology Group-Neurotoxicity (Fact/GOG-Ntx) questionnaire for patients receiving systemic chemotherapy. Int J Gynecol Cancer 13:741–748. https://doi.org/10.1111/j.1525-1438.2003.13603.x
Sullivan MJL, Bishop SR, Pivik J (1995) The pain catastrophizing scale: development and validation. Psychol Assess 7:524–532. https://doi.org/10.1037/1040-3590.7.4.524
Gotink RA, Younge JO, Wery MF, Utens EMWJ, Michels M, Rizopoulos D, van Rossum LFC, Roos-Hesselink JW, Hunink MMG (2017) Online mindfulness as a promising method to improve exercise capacity in heart disease: 12-month follow-up of a randomized controlled trial. PLoS ONE 12:e0175923. https://doi.org/10.1371/journal.pone.0175923
Hernán MA, Hernández-Díaz S (2012) Beyond the intention-to-treat in comparative effectiveness research. Clin Trials 9:48–55. https://doi.org/10.1177/1740774511420743
Tripepi G, Chesnaye NC, Dekker FW, Zoccali C, Jager KJ (2020) Intention to treat and per protocol analysis in clinical trials. Nephrology (Carlton) 25:513–517. https://doi.org/10.1111/nep.13709
S Malay SUN Study Group KC Chung 2013 The minimal clinically important difference after simple decompression for ulnar neuropathy at the elbow J Hand Surg Am 38 652 659 https://doi.org/10.1016/j.jhsa.2013.01.022
London DA, Stepan JG, Calfee RP (2014) Determining the Michigan Hand Outcomes Questionnaire minimal clinically important difference by means of three methods. Plast Reconstr Surg 133:616–625. https://doi.org/10.1097/PRS.0000000000000034
Bodur H, Yilmaz O, Keskin D (2006) Hand disability and related variables in patients with rheumatoid arthritis. Rheumatol Int 26:541–544. https://doi.org/10.1007/s00296-005-0023-1
Zimmerman NB, Kaye MB, Wilgis EFS, Zimmerman RM, Dubin NH (2009) Are standardized patient self-reporting instruments applicable to the evaluation of ulnar neuropathy at the elbow? J Shoulder Elbow Surg 18:463–468. https://doi.org/10.1016/j.jse.2009.02.010
Winters-Stone KM, Horak F, Jacobs PG, Trubowitz P, Dieckmann NF, Stoyles S, Faithfull S (2017) Falls, functioning, and disability among women with persistent symptoms of chemotherapy-induced peripheral neuropathy. J Clin Oncol 35:2604–2612. https://doi.org/10.1200/JCO.2016.71.3552
Lee P, Liu CH, Fan CW, Lu CP, Lu WS, Hsieh CL (2013) The test–retest reliability and the minimal detectable change of the Purdue pegboard test in schizophrenia. J Formos Med Assoc 112:332–337. https://doi.org/10.1016/j.jfma.2012.02.023
Streckmann F, Lehmann HC, Balke M, Schenk A, Oberste M, Heller A, Schürhörster A, Elter T, Bloch W, Baumann FT (2019) Sensorimotor training and whole-body vibration training have the potential to reduce motor and sensory symptoms of chemotherapy-induced peripheral neuropathy-a randomized controlled pilot trial. Support Care Cancer 27:2471–2478. https://doi.org/10.1007/s00520-018-4531-4
Umeki N, Murata J, Higashijima M (2019) Effects of training for finger perception on functional recovery of hemiplegic upper limbs in acute stroke patients. Occup Ther Int 2019:6508261. https://doi.org/10.1155/2019/6508261
Duregon F, Vendramin B, Bullo V, Gobbo S, Cugusi L, Blasio AD, Neunhaeuserer D, Zaccaria M, Bergamin M, Ermolao A (2019) Effects of exercise on cancer patients suffering chemotherapy-induced peripheral neuropathy undergoing treatment: a systematic review. Crit Rev Oncol Hematol 121:90–100. https://doi.org/10.1016/j.critrevonc.2017.11.002
Campbell KL, Winters-Stone KM, Wiskemann J, May AM, Schwartz AL, Courneya KS, Zucker DS, Matthews CE, Ligibel JA, Gerber LH, Morris GS, Patel AV, Hue TF, Perna FM, Schmitz KH (2019) Exercise guidelines for cancer survivors: consensus statement from international multidisciplinary roundtable. Med Sci Sports Exerc 51:2375–2390. https://doi.org/10.1249/MSS.0000000000002116
IR Kleckner SB Park F Streckmann J Wiskemann S Hardy N Mohile 2021 Systematic review of exercise for prevention and management of chemotherapy-induced peripheral neuropathy symptoms https://doi.org/10.1007/s11764-021-00997-w
Omran M, Belcher EK, Mohile NA, Kesler SR, Janelsins MC, Hohmann AG, Kleckner IR (2021) Review of the role of the brain in chemotherapy-induced peripheral neuropathy. Front Mol Biosci 8:693133. https://doi.org/10.3389/fmolb.2021.693133
Wang XM, Lehky TJ, Brell JM, Dorsey SG (2012) Discovering cytokines as targets for chemotherapy-induced painful peripheral neuropathy. Cytokine 59:3–9. https://doi.org/10.1016/j.cyto.2012.03.027
Lees JG, Makker PGS, Tonkin RS, Abdulla M, Park SB, Goldstein D, Moalem-Taylor G (2017) Immune-mediated processes implicated in chemotherapy-induced peripheral neuropathy. Eur J Cancer 73:22–29. https://doi.org/10.1016/j.ejca.2016.12.006
Gleeson M, Bishop NC, Stensel DJ, Lindley MR, Mastana SS, Nimmo MA (2011) The anti-inflammatory effects of exercise: mechanisms and implications for the prevention and treatment of disease. Nat Rev Immunol 11:607–615. https://doi.org/10.1038/nri3041
Kleckner IR, Kamen C, Cole C, Fung C, Heckler CE, Guido JJ, Culakova E, Onitilo AA, Conlin A, Kuebler JP, Mohile S, Janelsins M, Mustian KM (2019) Effects of exercise on inflammation in patients receiving chemotherapy: a nationwide NCORP randomized clinical trial. Support Care Cancer 27:4615–4625. https://doi.org/10.1007/s00520-019-04772-7
Khosravi N, Stoner L, Farajivafa V, Hanson ED (2019) Exercise training, circulating cytokine levels and immune function in cancer survivors: a meta-analysis. Brain Behav Immun 81:92–104. https://doi.org/10.1016/j.bbi.2019.08.187
Park JS, Kim S, Hoke A (2015) An exercise regimen prevents development paclitaxel induced peripheral neuropathy in a mouse model. J Peripher Nerv Syst 20:7–14. https://doi.org/10.1111/jns.12109
Slivicki RA, Mali SS, Hohmann AG (2019) Voluntary exercise reduces both chemotherapy-induced neuropathic nociception and deficits in hippocampal cellular proliferation in a mouse model of paclitaxel-induced peripheral neuropathy. Neurobiol Pain 6:100035. https://doi.org/10.1016/j.ynpai.2019.100035
Park JS, Höke A (2014) Treadmill exercise induced functional recovery after peripheral nerve repair is associated with increased levels of neurotrophic factors. PLoS ONE 9:e90245. https://doi.org/10.1371/journal.pone.0090245
Chu SH, Lee YJ, Lee ES, Geng Y, Wang XS, Cleeland CS (2015) Current use of drugs affecting the central nervous system for chemotherapy-induced peripheral neuropathy in cancer patients: a systematic review. Support Care Cancer 23:513–524. https://doi.org/10.1007/s00520-014-2408-8
Ishikawa K, Kajiwara Y, Sakamoto J, Sasaki R, Goto K, Honda Y, Kataoka H, Okita M (2019) Low-intensity muscle contraction exercise following the onset of arthritis improves hyperalgesia via reduction of joint inflammation and central sensitization in the spinal cord in a rat model. Neurosci Lett 706:18–23. https://doi.org/10.1016/j.neulet.2019.04.031
Funding
This study was partially funded by the grant of the Japanese Association of Occupational Therapists.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The study was approved by the hospital ethics committee before the start of the study (approval number 463). Informed consent was obtained from all individual participants included in the study.
Consent for publication
Not applicable.
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
The original version of this article was revised. Tables 1, 2, 3 are now corrected.
Rights and permissions
About this article
Cite this article
Ikio, Y., Sagari, A., Nakashima, A. et al. Efficacy of combined hand exercise intervention in patients with chemotherapy-induced peripheral neuropathy: a pilot randomized controlled trial. Support Care Cancer 30, 4981–4992 (2022). https://doi.org/10.1007/s00520-022-06846-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00520-022-06846-5