Abstract
Introduction
This study aimed to investigate long-term neurocognitive, psychological, and return to work (RTW) outcomes in meningioma patients, and to explore whether neurocognitive and psychological factors influence RTW outcomes in this population.
Methods
In this retrospective study, 61 meningioma patients completed in-depth clinical neuropsychological assessments. Of these participants, 42 were of working-age and had RTW information available following neuropsychological assessment. Seventy-one percent and 80% of patients received radiation and surgery, respectively, with 49% receiving both radiation and surgery. Associations between demographic, medical, neurocognitive, psychological, and RTW data were analyzed using multivariable logistic regression analyses.
Results
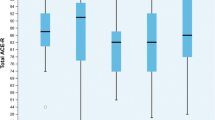
In our sample, 68% of patients exhibited global neurocognitive impairment, with the largest effect sizes found on tests of visual memory (d = 0.73), executive function (d = 0.61), and attention (d = 0.54). Twenty-seven percent exhibited moderate to severe levels of depressive symptoms. In addition, 23% and 30% exhibited clinically significant state and trait anxiety, respectively. Forty-eight percent of patients were unable to RTW. Younger age, faster visuomotor processing speed, and, unexpectedly, higher trait anxiety scores were associated with an increased likelihood of returning to work.
Conclusions
Meningioma patients are at risk of experiencing neurocognitive deficits, psychological symptoms, and difficulties returning to work. Our results suggest that neurocognitive and psychological factors contribute to RTW status in meningioma patients. Prospective research studies are necessary to increase our understanding of the complexity of functional disability in this growing population.
Similar content being viewed by others
Data availability
The datasets generated during and/or analyzed during the current study are available from the corresponding author on reasonable request.
Code availability
Not applicable.
Notes
Two participants were not administered the BDI-II.
Five participants were not administered the STAI.
References
Walker, Zakaria D, Yuan Y, Yasmin F, Shaw A, Davis F (2021) Brain Tumour Registry of Canada (BRTC): incidence (2013–2017) and mortality (2014–2018) report. Brain Tumour Registry of Canada (BTRC) A Surveillance Research Collaborative
Louis DN, Perry A, Reifenberger G, von Deimling A, Figarella-Branger D, Cavenee WK et al (2016) The 2016 World Health Organization classification of tumors of the central nervous system: a summary. Acta Neuropathol 131:803–820. https://doi.org/10.1007/s00401-016-1545-1
Goldbrunner R, Stavrinou P, Jenkinson MD, Sahm F, Mawrin C, Weber DC, et al. (2021) EANO guidelines on the diagnosis and management of meningioma. Neuro Oncol
Corniola MV, Meling TR (2021) Functional outcome and quality of life after meningioma surgery: a systematic review. Acta Neurol Scand 143:467–474. https://doi.org/10.1111/ane.13395
Meskal I, Gehring K, Rutten GJM, Sitskoorn MM (2016) Cognitive functioning in meningioma patients: a systematic review. J Neurooncol 128:195–205. https://doi.org/10.1007/s11060-016-2115-z
Rijnen SJ, Meskal I, Bakker M, De Bain W, Rutten GJM, Gehring K, et al. (2019) Cognitive outcomes in meningioma patients undergoing surgery: individual changes over time and predictors of late cognitive functioning. Neuro Oncol
Williams T, Brechin D, Muncer S, Mukerji N, Evans S, Anderson N (2019) Meningioma and mood: exploring the potential for meningioma to affect psychological distress before and after surgical removal. Br J Neurosurg 1–5. https://doi.org/10.1080/02688697.2019.1571163.
Najafabadi AHZ, van der Meer PB, Boele FW, Taphoorn MJB, Klein M, Peerdeman SM et al (2021) Long-term disease burden and survivorship issues after surgery and radiotherapy of intracranial meningioma patients. Neurosurgery 88:155–164. https://doi.org/10.1093/neuros/nyaa351
Dijkstra M, Van Nieuwenhuizen D, Stalpers LJA, Wumkes M, Waagemans M, Vandertop WP et al (2009) Late neurocognitive sequelae in patients with WHO grade I meningioma. J Neurol Neurosurg Psychiatry 80:910–915. https://doi.org/10.1136/jnnp.2007.138925
Porter KR, McCarthy BJ, Freels S, Kim Y, Davis FG (2010) Prevalence estimates for primary brain tumors in the United States by age, gender, behavior, and histology. Neuro Oncol 6:520–527. https://doi.org/10.1093/neuonc/3.3.152
Kalkanis SN, Quinones-Hinojosa A, Buzney E, Ribaudo HJ, Black P (2000) Quality of life following surgery for intracranial meningiomas at Brigham and Women’s Hospital: a study of 164 patients using a modification of the functional assessment of cancer therapy-brain questionnaire. J Neurooncol 48:233–241. https://doi.org/10.1023/A:1006476604338
Schepers VPM, Van Der Vossen S, Berkelbach Van Der Sprenkel JW, Visser-Meily JMA, Post MWM (2018) Participation restrictions in patients after surgery for cerebral meningioma. J Rehabil Med 50:879–85. https://doi.org/10.2340/16501977-2382.
Thurin E, Corell A, Gulati S, Smits A, Henriksson R, Bartek J et al (2020) Return to work following meningioma surgery: a Swedish nationwide registry-based matched cohort study. Neuro-Oncology Pract 7:320–328. https://doi.org/10.1093/nop/npz066
Schiavolin S, Mariniello A, Broggi M, Acerbi F, Schiariti M, Franzini A et al (2021) Characteristics of patients returning to work after brain tumor surgery. Front Hum Neurosci 14:1–8. https://doi.org/10.3389/fnhum.2020.609080
Ownsworth T, Hawkes A, Steginga S, Walker D, Shum D (2009) A biopsychosocial perspective on adjustment and quality of life following brain tumor: a systematic evaluation of the literature. Disabil Rehabil 31:1038–1055. https://doi.org/10.1080/09638280802509538
Mani K, Cater B, Hudlikar A (2017) Cognition and return to work after mild/moderate traumatic brain injury: a systematic review. Work 58:51–62. https://doi.org/10.3233/WOR-172597
Najafabadi AHZ, van der Meer PB, Boele FW, Taphoorn MJB, Klein M, Peerdeman SM et al (2021) Determinants and predictors for the long-term disease burden of intracranial meningioma patients. J Neurooncol 151:201–210. https://doi.org/10.1007/s11060-020-03650-1
Greiffenstein MF, Baker WJ, Gola T (1994) Validation of malingered amnesic measures with a large clinical sample. Psychol Assess 6:218–224
Reitan RM (1958) Validity of the trail making test as an indicator of organic brain damage. Percept Mot Skills 8:271–276
Beck A, Steer R, Brown G (1996) Manual for the Beck Depression Inventory-II. San Antonio, TX: Psychological Corportation
Spielberger CD, Gosuch RL, Lushene PR, Vagg PR, Jacobs AG (1983) Manual for the State-Trait Anxiety Inventory (Form Y). Consulting Psychologists Press, Palo Alto
Wefel JS, Vardy J, Ahles T, Schagen SB (2011) International Cognition and Cancer Task Force recommendations to harmonise studies of cognitive function in patients with cancer. Lancet Oncol 12:703–708. https://doi.org/10.1016/S1470-2045(10)70294-1
Cohen J (1988) Statistical power analysis for the behavioral sciences, 2nd edn. Erlbaum, New York
Zakzanis KK (2001) Statistics to tell the truth, the whole truth, and nothing but the truth. Formulae, illustrative numerical examples, and heuristic interpretation of effect size analyses for neuropsychological researchers. Arch Clin Neuropsychol 16:653–67. https://doi.org/10.1016/S0887-6177(00)00076-7.
Corp IBM (2019) IBM SPSS Statistics Version 26. IBM Corporation, Armonk, NY
R Core Team (2020) R: a language and environment for statistical computing. Vienna: R Foundation for Statistical Computing
McWhirter L, Ritchie CW, Stone J, Carson A (2020) Performance validity test failure in clinical populations- a systematic review. J Neurol Neurosurg Psychiatry 91:945–952. https://doi.org/10.1136/jnnp-2020-323776
Zenisek R, Millis SR, Banks SJ, Miller JB (2016) Prevalence of below-criterion Reliable Digit Span scores in a clinical sample of older adults. Arch Clin Neuropsychol 31:426–433. https://doi.org/10.1093/arclin/acw025
Jeffay E, Binder LM, Zakzanis KK (2021) Marked intraindividual cognitive variability in a sample of healthy graduate students. Psychol Inj Law. https://doi.org/10.1007/s12207-021-09417-x
Schretlen DJ, Testas SM, Winicki JM, Pearlson GD, Gordon B (2008) Frequency and bases of abnormal performance by healthy adults on neuropsychological testing. J Int Neuropsychol Soc 14:436–445. https://doi.org/10.1017/S1355617708080387
Bonelli RM, Cummings JL (2007) Frontal-subcortical circuitry and behavior. Dialogues Clin Neurosci 9:141–151
Meskal I, Gehring K, van der Linden SD, Rutten GJM, Sitskoorn MM (2015) Cognitive improvement in meningioma patients after surgery: clinical relevance of computerized testing. J Neurooncol 121:617–625. https://doi.org/10.1007/s11060-014-1679-8
Weyer-Jamora C, Brie MS, Luks TL, Smith EM, Braunstein SE, Villanueva-Meyer JE et al (2021) Cognitive impact of lower-grade gliomas and strategies for rehabilitation. Neuro-Oncology Pract 8:117–128. https://doi.org/10.1093/nop/npaa072
Richard NM, Bernstein LJ, Mason WP, Laperriere N, Maurice C, Millar BA et al (2019) Cognitive rehabilitation for executive dysfunction in brain tumor patients: a pilot randomized controlled trial. J Neurooncol 142:565–575. https://doi.org/10.1007/s11060-019-03130-1
Goebel S, Von Harscher M, Mehdorn H (2011) Comorbid mental disorders and psychosocial distress in patients with brain tumours and their spouses in the early treatment phase. Support Care Cancer 19:1797–1805. https://doi.org/10.1007/s00520-010-1021-8
Gibson AW, Graber JJ (2021) Distinguishing and treating depression, anxiety, adjustment, and post-traumatic stress disorders in brain tumor patients. Ann Palliat Med 10:875–892. https://doi.org/10.21037/apm-20-509
Kangas M (2015) Psychotherapy interventions for managing anxiety and depressive symptoms in adult brain tumor patients: a scoping review. Front Oncol 5. https://doi.org/10.3389/fonc.2015.00116.
Senft C, Behrens M, Lortz I, Wenger K, Filipski K, Seifert V et al (2020) The ability to return to work: a patient-centered outcome parameter following glioma surgery. J Neurooncol 149:403–411. https://doi.org/10.1007/s11060-020-03609-2
Moritz-Gasser S, Herbet G, Maldonado IL, Duffau H (2012) Lexical access speed is significantly correlated with the return to professional activities after awake surgery for low-grade gliomas. J Neurooncol 107:633–641. https://doi.org/10.1007/s11060-011-0789-9
Clemens L, Langdon D (2018) How does cognition relate to employment in multiple sclerosis? A systematic review. Mult Scler Relat Disord 26:183–191. https://doi.org/10.1016/j.msard.2018.09.018
Saunders SL, Nedelec B (2014) What work means to people with work disability: a scoping review. J Occup Rehabil 24:100–110
Gheaus A, Herzog L (2016) The goods of work (other than money!). J Soc Philos 47:70–89
Liaset IF, Kvam L (2018) Experiences of returning to work after brain tumor treatment. Work 60:603–612. https://doi.org/10.3233/WOR-182768
Mellifont D, Smith-Merry J, Scanlan JN (2016) Pitching a Yerkes-Dodson curve ball?: a study exploring enhanced workplace performance for individuals with anxiety disorders. J Workplace Behav Health 31:71–86. https://doi.org/10.1080/15555240.2015.1119654
Ostrom QT, Gittleman H, Truitt G, Boscia A, Kruchko C, Barnholtz-Sloan JS (2018) CBTRUS statistical report: primary brain and other central nervous system tumors diagnosed in the United States in 2011–2015. Neuro Oncol 20:iv1–86. https://doi.org/10.1093/neuonc/noy131.
Rogers L, Gilbert M, Vogelbaum MA (2010) Intracranial meningiomas of atypical (WHO grade II) histology. J Neurooncol 99:393–405. https://doi.org/10.1007/s11060-010-0343-1
Nassiri F, Liu J, Patil V, Mamatjan Y, Wang JZ, Hugh-White R, et al. (2021) A clinically applicable integrative molecular classification of meningiomas. Nature 597. https://doi.org/10.1038/s41586-021-03850-3.
Hutchinson S, Steginga SK, Dunn J (2006) The tiered model of psychosocial intervention in cancer: a community based approach. Psychooncology 15:541–546
Funding
This work was supported in part by the Princess Margaret Cancer Foundation, and the Ontario Ministry of Health and Long Term Care (OMOHLTC). The views expressed do not necessarily reflect those of the OMOHLTC.
Author information
Authors and Affiliations
Contributions
AS, KE, KKZ, and DM designed the study. AS, KE, and KKZ drafted the manuscript. AS performed the analyses. KKZ, DM, DST, PK, GZ, and KE critically revised the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval
This retrospective chart review study involving human participants was in accordance with the ethical standards of the institutional research committee and with the Declaration of Helsinki. Approval was granted by the Research Ethics Board’s at the University Health Network and the University of Toronto.
Consent to participate
Not applicable.
Consent for publication
Not applicable.
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Sekely, A., Zakzanis, K.K., Mabbott, D. et al. Long-term neurocognitive, psychological, and return to work outcomes in meningioma patients. Support Care Cancer 30, 3893–3902 (2022). https://doi.org/10.1007/s00520-022-06838-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00520-022-06838-5