Abstract
Background
Paclitaxel regimen which is widely used in clinical treatment causes many negative physical and psychological consequences on women with breast cancer (BC). This longitudinal study firstly aimed to investigate symptom status, body perception changes, and the risk of anxiety and depression in BC patients receiving during paclitaxel regimen.
Materials and methods
This descriptive and prospective study was conducted with 84 BC patients receiving paclitaxel regimen. “Chemotherapy Symptom Assessment Scale (C-SAS),” “Body Perception Scale (BPS),” and “Hospital Anxiety and Depression Scale (HADS)” were applied at five time points (T1, before the first Paclitaxel infusion; T2, at the end of first cycle; T3, at the end of fourth cycle; T4, at the end of eighth cycle; T5, at the end of twelfth cycle). Data was analyzed using descriptive statistics, Cochrane Q, and linear mix model regression analysis.
Results
The frequency of needling and numbness in hands and feet, pain, and skin or nail changes significantly increased in the subsequent assessment points (T2, T3, T4, and T5) compared to the initial assessment (T1) (p < 0.05). The mean scores of BPS significantly decreased at T2, T4, and T5 compared to T1 (F = 8.152, p < 0.001). The mean scores of the anxiety subscale of the HADS scale decreased at the T3, T4, and T5 compared to T1 (F = 6.865, p < 0.001), and the mean scores of the depression subscale significantly increased at the T5 compared to T1 (F = 3.708, p = 0.006).
Conclusions
The oncology nurse should comprehensively evaluate the patients who scheduled to receive paclitaxel treatment, and provide counseling to the patients during these specific weeks. Better management of the symptoms that increase with the paclitaxel regimen with repeated interviews under the supervision of the nurse will also prevent the deterioration of body perception. In addition, since the risk of depression increases over time in patients receiving paclitaxel, nurses should periodically screen the risk of depression, and timely consult the patients for the appropriate support.
Similar content being viewed by others
Introduction
Breast cancer (BC) is the most common type of cancer among women worldwide, causing significant rates of mortality and morbidity [1, 2]. In recent years, adjuvant and neoadjuvant systemic therapies have started to take an important place in BC treatment to reduce the associated mortality rate, in addition to the classical treatment methods such as surgery, chemotherapy, and radiotherapy [3].
Paclitaxel is frequently preferred during adjuvant and neoadjuvant therapies [4]. Paclitaxel is a taxane group drug and can be administered weekly (12 weeks) or every 21 days (four cycles) after four cycles of Adriamycin–cyclophosphamide (AC) treatment in patients with early-stage BC [5,6,7]. With the increasing clinical use of paclitaxel in BC, it is reported that therapeutic response, survival, and disease-free survival rates have increased [6].
Paclitaxel, which cannot cross the blood–brain barrier, induces symptoms by causing toxic effects in the periphery. Dynamic instability of microtubules in the cell is necessary for mitosis. Paclitaxel stabilizes the microtubule by binding to the lumens of the cell, stops mitosis, and eventually causes apoptosis. In particular, neurons are frequently affected by paclitaxel even though they are not dividing cells [8]. Paclitaxel often causes significant symptoms such as neutropenia, nausea, vomiting, diarrhea, oral mucositis, amenorrhea, alopecia, arthralgia, myalgia, peripheral neuropathy, skin and nail changes, liver and renal toxicity, and hypersensitivity reactions in BC patients depending on the number of cycles, and the dose administered [5, 6, 9,10,11]. In particular, during the weekly administered paclitaxel regimen, patients are found feeling uncomfortable due to arthralgia and myalgia, taste changes, peripheral neuropathy, fatigue, cognitive problems, and insomnia [12]. In addition, neurotoxicity is reported to be associated with the increasing cumulative dose of the paclitaxel [11]. Patients with BC receiving paclitaxel also experience anxiety, depression, and decrease in body perception due to physiological effects of paclitaxel including alopecia, changes in sexual life, menstrual disorders, weight changes, and changes in nails/skin [13,14,15].
Parallel to the increasing symptom status during the BC treatment, patients find it increasingly difficult to adapt to the treatment. Changes in physical, cognitive, and emotional statuses may also cause a decline in body perception [16]. Body perception in BC patients is negatively affected during the paclitaxel regimen as a result of edema, weight changes, alopecia, differentiation in skin color and nails, oral mucositis, menstrual cycle disorders, and sexual life problems [17, 18]. At the same time, as in many cultures, imputed meanings related to aesthetic appearance, femininity, attractiveness, sexuality, and motherhood in Turkish culture make the treatment process even more difficult for patients with BC [19, 20]. Several studies have also highlighted that chemotherapy and mastectomy, which have an important place in the BC treatment, negatively affect the body perception in BC patients [13, 14, 21].
Another clinical situation that needs to be considered is that emotional changes, including distress, anxiety, and depression in BC patients. Experienced symptoms, decreased body perception, and increased anxiety during BC treatment cause more difficulty in coping with the treatment process in BC patients, and lead to the formation of a risk group for depression [17]. Previous studies conducted with BC patients reported that alopecia, weight changes, fatigue, and difficulties in sexual life are directly related to higher anxiety, and depression levels in those undergoing surgery and chemotherapy [15, 22, 23]. Besides, numerous studies have emphasized that the anxiety levels are higher in the first year after a BC diagnosis [24], which gradually decrease during the treatment [25].
In the literature, no studies have been found that investigated changes in symptom status, body perception, and the risk of anxiety, and depression prospectively in patients with BC scheduled to receive paclitaxel regimen. This study is the first attempt to fill this research gap by investigating changes in body perception, symptom status, and the risk of anxiety and depression concurrently, and determining the time intervals of deterioration in these three variables in BC patients who scheduled to receive paclitaxel regimen. Therefore, this study aimed to determine the symptom status, body perception changes, and the risk of anxiety and depression in patients with BC for a total of 12 weeks. It is assumed that determining the time intervals during the paclitaxel treatment when the risk of anxiety and depression occurs can enable the planning of comprehensive education programs and counseling sessions for BC patients and reduce the symptom burden and the deterioration in body perception with structured nursing interventions.
Research questions
-
How do the symptom status change in BC patients during the paclitaxel regimen?
-
How do body perception levels change in BC patients during the paclitaxel regimen?
-
How do the symptoms of anxiety and depression change in BC patients during the paclitaxel regimen?
Methods
Study design and setting
This descriptive and prospective study was conducted between July 29, 2019, and June 15, 2020, at three centers including the Hacettepe University Oncology Hospital, Health Sciences University Dr Abdurrahman Yurtaslan Ankara Oncology Training and Research Hospital, and Ankara City Hospital located in Ankara, Turkey. Participants were recruited from the outpatient clinics of the Departments of Clinical Oncology of the three local public hospitals. All patients selected for this study received a total of 12 paclitaxel infusions in the oncology outpatient clinic once a week, for a total of 12 weeks.
Participants
The population of the study consisted of patients with BC who received the first cure of the paclitaxel regimen in the daytime treatment units. The patients who met the inclusion criteria were included in the study without using any sampling method. Considering the correlation coefficient as 0.30 between the BPS and the HADS total scores, the sample size was calculated at least 84 patients with a power of 80% through the G Power 3.1.10 program. Patients aged between 18 and 65 years, who were diagnosed of BC and had completed four cycles of AC regimen prior to the paclitaxel regimen and all the 12 cycles of the paclitaxel, were included in the study. Those who had communication problems, had a psychiatric diagnosis (major depression, etc.), had a different cancer diagnosis, had previous history of radiotherapy, using relaxation techniques or antidepressants during the study, could not complete 12 cycles of the paclitaxel regimen, and were not willing to participate were excluded from the study. In this context, a total of 88 patients were assessed; four patients were excluded due to following reasons: did not want to continue the study (n = 2), could not be reached after the fourth cycle (n = 1), and did not want to receive her treatment due to fear of coronavirus-19 disease (COVID-19) (n = 1). Finally, this study was completed with 84 patients.
Data collection tools
Demographic and clinical information form
This form developed based on the literature [4,5,6, 26], and consisted of age, height, weight, body mass index, educational level, marital status, income level, employment status, whether having children or not, accompanying comorbidities, duration of BC diagnosis, BC stage, previous treatments, mastectomy status, people living together with, and residency in Ankara, Turkey.
Chemotherapy Symptom Assessment Scale (C-SAS)
This scale was developed to determine the symptom status of cancer patients receiving chemotherapy treatment [20]. The Turkish version of the C-SAS was studied by Aslan et al. (2006) [19]. It includes 24 different symptoms that may occur during chemotherapy. Patients are asked to identify the status of experiencing each symptom as “yes”/”no.” Since each symptom is evaluated separately, the arithmetic mean values are not used in evaluating the scale scores. In the Turkish validity and reliability study of the scale, the Cronbach alpha coefficient was found as 0.82 [19, 20]. In this study, Cronbach’s alpha coefficient was calculated as 0.62.
Body Perception Scale (BPS)
This scale was developed by Secord and Jourard (1953) [27]. It contains 40 five-point Likert-type questions about body region or function. These 40 items include five assessment criteria related to each organ or body function (starting from 1 = “I do not like” to 5 = “I like very much”). Total score that can be obtained from the scale varies between 40 and 200. An increase in the total score indicates that a person’s satisfaction with the part or functionality that makes up his/her body increases. The Turkish validity and reliability study of the scale was conducted by Hovardaoğlu (1993) and the Cronbach alpha coefficient was found as 0.91 [28]. In this study, the Cronbach’s alpha coefficient value was calculated to be 0.84.
Hospital Anxiety and Depression Scale (HADS)
HADS was developed by Zigmond and Snaith (1983) [29] to determine the risk status for anxiety and depression in patients with physical disorders, and its Turkish version was studied by Aydemir et al. (1997) [30]. It includes 14 questions and two sub-dimensions as anxiety and depression. Seven questions (odd numbered) measure anxiety (HAD-A) while the other seven questions (even numbered) measure depression (HAD-D). In the scale, questions are scored on a four-point Likert scale, each ranging from 0 to 3. The lowest score that a patient can get from each sub-dimension is 0, and the highest score is 21. As the total scores increase, patients are considered at risk for anxiety and depression. In the Turkish validity and reliability study of the scale, the Cronbach alpha coefficient was found as 0.85 and 0.77 for the anxiety and depression sub-dimensions, respectively [30]. In this study, the Cronbach’s alpha coefficient values were calculated as 0.86 and 0.79 for the anxiety and depression sub-dimensions in this study, respectively.
Data collection procedure
Baseline data (T1) were collected on the day of the first paclitaxel infusion, before the first infusion was given, using the demographic and clinical information form, C-SAS, BPS, and HADS from the patients who met the inclusion criteria. The patients were prospectively followed by the principal investigator (PI) during the paclitaxel regimen for a total of 12 weeks. The C-SAS, BPS, and the HADS were reapplied to the patients by the PI at the end of the first cycle (first week, T2), fourth cycle (fourth week, T3), eighth cycle (eighth week, T4), and twelfth cycle (twelfth week, T5) during the paclitaxel regimen.
Statistical analysis
Data analysis was performed using Statistical Package for the Social Sciences (SPSS version 23; IBM, Armonk, New York). Descriptive statistics (mean, median, standard deviation, minimum, maximum, percentage, and frequency) were used in the evaluation of the socio-demographic data. Data were analyzed for normality using Kolmogorov–Smirnov test. The Cochran’s Q test, a nonparametric way, was used to determine the changes in the frequency of symptoms evaluated by C-SAS. Longitudinal processing was used for the analysis of repeated measurements. Linear mix model of repeated measurements was used to analyze the progression of BPS and HADS scores at T1 (reference category), T2, T3, T4, and T5. The statistical significance value in the study was set as p < 0.05.
Ethical considerations
Ethical approval was obtained from the Hacettepe University Non-Interventional Clinical Research Ethics Committee (2019/06–10), and institutional permissions were obtained from hospital administrations. All information was collected in accordance with the Declaration of Helsinki. Informed consent forms were obtained from all the patients included in the study. The PI gave information to the patients about the importance, purpose, and contributions of the study in the first interview, received the contact numbers of the patients, and applied the data collection tools using a face-to-face interview technique.
Results
The descriptive characteristics of the patients are given in Table 1. Most of the sample had completed primary school (60.7%) and did not work (73.8%); however, half of the patients reported having a mid-level income. The great majority of participants were married (85.7%) and had children (89.3%). A total of 47.6% of the patients had stage-2 BC, 77.4% had undergone breast surgery and chemotherapy treatments before, and 26.2% had come from other cities to receive their scheduled treatment. The big majority of patients (94%) lived with their family, and nearly half (45.2%) of those had at least one additional chronic disease. The mean age of patients was 49.57 ± 8.14 years. The mean value of the body mass index was 29.49 ± 5.50, and the average number of children was 2.14 ± 1.04. The mean time of diagnosis was 5.51 ± 1.66 months; the time since diagnosis was 3–6 months in 81% of the patients.
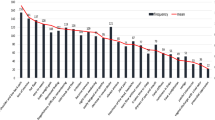
Changes in symptom frequency among the patients were prospectively evaluated at five different time points (T1, T2, T3, T4, and T5) during the 12-week paclitaxel regimen (Table 2). Cochran’s Q test results showed the differences in matched sets of symptoms in this longitudinal study. When the symptoms of nausea and vomiting (after treatment), constipation, weight loss or weight gain, changes in appetite, problems with the eyes, feelings of extraordinary fatigue, headaches, anxiety or distress, pessimism and sadness, changes in sexual life, and changes in the menstrual cycle were compared with symptom statuses of the baseline assessment (T1), a significant decrease was observed in the aforementioned symptoms in all the subsequent measurements (T2, T3, T4, and T5) (p < 0.05). Besides, the frequency of feeling needling, numbness, and pain in the hands and feet increased in the subsequent assessments (T2, T3, T4, and T5) compared to the baseline assessment (T1) (p < 0.05). In addition, according to the baseline assessment (T1) and the assessment at the end of the first cycle (T2), the increase in the frequency of sleep disturbances in the fifth assessment (T5) cycle remained statistically significant (p < 0.05). Finally, the frequency of skin and nail changes gradually increased from T2 to T5 (p < 0.05). However, the differences between the measurements (T1, T2, T3, T4, T5) were not statistically significant in terms of nausea and vomiting (before treatment), diarrhea, dyspnea, signs of infection, bleeding or bruising, hair loss, weakness, and problems with the mouth and throat (p > 0.05).
Regarding the changes in the mean BPS scores of the patients during the paclitaxel regimen, the corresponding scores were 134.75 ± 13.73 at T1, 130.54 ± 14.63 at T2, 132.33 ± 12.01 at T3, 129.60 ± 12.62 at T4, and 124.07 ± 10.44 at T5 (Table 3). When the reference category was taken as the T1 (before the first paclitaxel infusion), body perception scores at T2 time were 4.214 less than the T1. The corresponding scores at T4 time were 5.155 less than T1. Body perception scores at T5 time were 10.679 less than T1. No significant effect was found at T3 time compared to the reference category (T1) (Table 4). Considering Table 3, the effects of measurements repeated at different times on BPS scores were statistically significant based on the linear mix model established (F = 8.152, p < 0.001).
During the paclitaxel regimen in this study, the mean scores of the HADS-A sub-dimension were 6.61 ± 4.74 at T1, 5.63 ± 3.86 at T2, 4.48 ± 3.33 at T3, 4.18 ± 3.01 at T4, and 4.30 ± 3.15 at T5 (Table 3). When the reference category was taken as the T1 (before the first paclitaxel infusion), anxiety scores at T3 time were 2.131 lower than T1. Anxiety scores at T4 time were 2.429 less than T1. Anxiety scores at T5 time were 2.310 less than T1 (Table 5). No significant effect was found at T2 time compared to the reference category (T1). As for the mean scores of the HADS-D sub-dimension, it was found to be 6.00 ± 4.16 at T1, 5.64 ± 3.37 at T2, 6.13 ± 3.65 at T3, 6.90 ± 3.23 at T4, and 7.44 ± 2.85 at T5. The mean depression scores decreased in T2 compared to T1, increased in T3 compared to T2 and T4 compared to T3, and increased again in T5 compared to T4 (Table 3). Depression scores at T5 time were 1.440 higher than T1. And no significant effect was determined at T2, T3, and T4 times compared to the reference category (Table 5). Table 5 summarizes the results of the mixed linear model analysis for HADS-A and HADS-D scores, respectively. The effects of measurements repeated at different times on anxiety (F = 6.865, p < 0.001) and depression (F = 3.708, p = 0.006) scores were statistically significant.
Discussion
In this prospective study, we investigated the symptom status, body perception level changes, and the symptoms of anxiety and depression in BC patients receiving paclitaxel treatment using five different measurement points. While frequency of symptoms nausea-vomiting, fatigue, headaches, anxiety-distress decreased, needling, numbness, pain in the hands and feet, sleep disturbances, and skin-nail changes increased during the paclitaxel regimen in the present study. Like our findings, neuropathy, skin and nail toxicities, arthralgia, and myalgia were frequently reported in patients receiving paclitaxel regimen [8, 31,32,33]. Chemotherapy is reported to first affect the receptors in the gastrointestinal tract, inducing neurotransmitter release and stimulating the muscles in the stomach to create nausea/vomiting response in the relevant part of the brain [34], and triggers the mechanisms of acute, delayed, and anticipatory emesis. Previous studies have highlighted that chemotherapy-induced peripheral neurotoxicity, neuropathic pain, anxiety, and depression have been reported to be important risk factors for sleep disturbance and poor sleep quality in BC survivors [35]. Fatigue may be associated with cancer itself, and ongoing treatment, sleep problems, anxiety, depression, and peripheral neuropathy may also contribute to neuromuscular fatigue [36]. As paclitaxel cannot cross the blood–brain barrier, it frequently causes problems in the periphery, such as neuropathy. Proposed mechanisms for taxane-induced peripheral neuropathy and neuropathic pain include inflammation, peripheral nerve toxicity with nociceptor sensitization, resultant hyperalgesia, and immune system activation [35, 37]. In this prospective study, we firstly evaluated the symptom status before and after the treatment in BC patients and also reported that anxiety decreased and pain increased [38]. Bao et al. (2016) [39] confirmed that 58.4% of the BC patients receiving taxane chemotherapy had numbness in their hands and feet. In contrast to the present study, Azim et al. (2011) showed that women receiving adjuvant therapy had more serious sexual problems compared to those receiving other treatments [40]. In the current study, BC patients receive paclitaxel regimen.
In after four cycles of AC chemotherapy were followed within the scope of the standard paclitaxel regimen used only in the treatment of early-stage BC. Due to the high side effect profile of the AC cycle, many symptoms were found to be quite high at the beginning of the cycle and relatively lower at the end of the first cycle. The researchers assumed that the gradual decrease in the symptom frequency perceived by the BC patients in the later stages of adjuvant paclitaxel courses in the study sample could be due to easier tolerance for the paclitaxel therapy as against for the systematic and aggressive chemotherapy protocol, including the AC treatment. It is also known that repeated courses of paclitaxel cause peripheral neuropathy due to axonal degeneration at cumulative doses [41]. In our study, the increase in numbness and pain in the hands and feet confirms the previous literature.
This study also evaluated the changes in body perception levels during the paclitaxel regimen. Based on the findings, the body perception scores of the patients were found to be highest at T1, and lowest at T5. Similarly, Villar et al. (2017) found that the body perception levels of the BC patients receiving chemotherapy decreased in the last evaluation compared to the first evaluation [38]. Two studies carried out in Brazil and Israel reported that the body perception levels of BC patients receiving chemotherapy decreased by 74.8% and 80.9%, respectively [42, 43]. In a systematic review conducted by Paterson et al. (2016), the body perception of BC patients was negatively affected in 35 out of the 36 studies [14]. It is presumed that the changes in symptom status such as alopecia, skin and nail changes, and neuropathic pain in BC patients during the paclitaxel regimen might be influential on the perceived negative changes in body perception. These conditions may lead to a significant decrease in the body perception levels over time.
Another important finding of this study was that the mean scores of the HAD-A subscale decreased in the first four measurements (T1, T2, T3, and T4) and relatively increased in the last measurement (T5). Similarly, Villar et al. (2017) reported that the anxiety levels decreased significantly following the chemotherapy and radiotherapy treatments in BC patients [38]. Moreira and Canavarro (2010) also concluded that the anxiety levels of BC patients decreased during the period following surgery and chemotherapy [22]. Bergerot et al. (2017) stated that the anxiety levels of the cancer patients were highest on the first day and lowest on the last day of chemotherapy [44]. Considering all the findings of the studies, higher anxiety levels in the patients before the paclitaxel regimen may be related to the initiation of a new chemotherapy regimen and the uncertainties that may be experienced during the process. The decrease in the anxiety levels of the BC patients over time may be due to the relatively lower and moderate symptom severity during the paclitaxel regimen, and the improvement of physiological and psychological, individual coping strategies along with the increase in knowledge of and experience related to BC and its treatment.
We have also examined the changes in depression scores. Accordingly, the depression scores decreased at the end of T2 compared to T1 and gradually increased at T3, T4, and T5. Confirming the findings of this study, Byar et al. (2006) had reported earlier that depression levels were low at the beginning and increased as the treatment progressed in BC patients receiving adjuvant chemotherapy [45]. Oh and Cho (2020) also stated that while the depression rate was 4% in South Korean BC patients before the chemotherapy started, it reached 30% after the chemotherapy [46]. Considering all the results, the lower levels of depression at the end of the first cycle and the higher levels as the course progressed may be related to the symptoms, the lack of comprehensive management of these symptoms, and the changes in body perception and anxiety levels following 12 weeks of paclitaxel regimen. The increase in the symptoms of depression at the end of the treatment may be attributed to the uncertainties in the prognoses and the treatment options to be continued.
Limitations
Our findings should be interpreted in the context of some limitations. Since the treatment hours were at the same time in all the three study centers, some patients were missed and could never include in the study. Another limitation is that the first, fourth, eighth, and the twelfth (end of cure) assessments of 36 patients were compulsorily completed via phone interviews due to the announcement of the COVID-19 pandemic and the suspension of research in hospitals in Turkey as March 2020. Finally, we were limited with our demographic and clinical information form including cancer stage, previous treatments, number of children that may be associated with perceived anxiety, and depression. Therefore, further studies examining different variables that may increase the level of anxiety and depression, for example, providing care for children or older people, presence of family support, and employment status, are needed.
Conclusions
To the best of our knowledge, this is the first study evaluating BC patients receiving paclitaxel in terms of symptom status, body perception levels, and the risk of anxiety and depression at five different time points during the paclitaxel protocol. Findings from this longitudinal study indicate that an increase in symptoms including pain, pins and needles in hands-feet, problems with the skin or nails, and difficulty sleeping, while a decrease in anxiety, and body perception and increase in depression at the end of paclitaxel regimen compared with the baseline. Paclitaxel regimen had a negative impact on both perceived physical and psychological health on a population of BC. Our findings indicate that BC patients are particularly susceptible to such disruptions. Oncology nurses should be aware which symptoms may increase or decrease in BC patients receiving paclitaxel and plan their interventions for better management of these symptoms, and periodically screen and consult them regarding the changes in body perception, and the risk of anxiety and depression. Thus, vulnerable BC patients may be identified at an early stage and referred to professionals for appropriate support. This study showed that a comprehensive follow-up of BC patients by oncology nurses becomes important to alleviate the symptoms, improve body perception, and decrease the risk of anxiety and depression.
Data availability
The datasets generated during and/or analyzed during the current study are available from the corresponding author on reasonable request.
Code availability
Not applicable.
References
Mungan İ, Doğru O, Aygen E, Dağlı AF (2019) The relations of vascular endothelial growth factor–C and lymph node metastasis in breast cancer patients. J Surg Med 3:124–127
WHO (2018) [Erişim Tarihi: 05.12.2018]. International Agency for Research on Cancer [Internet]. [Online]. Available: https://gco.iarc.fr/today/data/factsheets/cancers/20-Breast-fact-sheet.pdf. [Accessed]
Desantis CE, Ma J, Goding Sauer A, Newman LA, Jemal A (2017) Breast cancer statistics, 2017, racial disparity in mortality by state. CA Cancer J Clin 67:439–448
Rowinsky EK, Donehower RC (1995) Paclitaxel (taxol). N Engl J Med 332:1004–1014
Shapiro CL, Recht A (2001) Side effects of adjuvant treatment of breast cancer. N Engl J Med 344:1997–2008
Erdemoğlu N, Şener B (2000) The antitumor effects of the taxane class compounds. Ankara Ecz Fak Derg 29:77–90
BC Cancer Kemoterapi Protokolleri. (2019,1 July). [Internet]. https://www.kanser.org/saglik/
Gornstein E, Schwarz TL (2014) The paradox of paclitaxel neurotoxicity: Mechanisms and unanswered questions. Neuropharmacology 76A:175–183
Sibaud V, Lebœuf NR, Roche H, Belum VR, Gladieff L, Deslandres M, Montastruc M, Eche A, Vigarios E, Dalenc F (2016) Dermatological adverse events with taxane chemotherapy. Eur J Dermato 26:427–443
Reeves BN, Dakhil SR, Sloan JA, Wolf SL, Burger KN, Kamal A, Le-Lindqwister NA, Soori GS, Jaslowski AJ, Kelaghan J (2012) Further data supporting that paclitaxel-associated acute pain syndrome is associated with development of peripheral neuropathy: North Central Cancer Treatment Group trial N08C1. Cancer 118:5171–5178
Pace A, Nisticò C, Cuppone F, Bria E, Galiè E, Graziano G, Natoli G, Sperduti I, Jandolo B, Calabretta F (2007) Peripheral neurotoxicity of weekly paclitaxel chemotherapy: a schedule or a dose issue? Clin Breast Cancer 7:550–554
Boehmke MM, Dickerson SS (2005) Symptom, symptom experiences, and symptom distress encountered by women with breast cancer undergoing current treatment modalities. Cancer Nurs 28:382–389
Begovic-Juhant A, Chmielewski A, Iwuagwu S, Chapman LA (2012) Impact of body image on depression and quality of life among women with breast cancer. J Psychosoc Oncol 30:446–460
Choi EK, Kim IR, Chang O, Kang D, Nam SJ, Lee JE, Lee SK, Im YH, Park YH, Yang JH (2014) Impact of chemotherapy-induced alopecia distress on body image, psychosocial well-being, and depression in breast cancer patients. Psychooncology 23:1103–1110
Paterson C, Lengacher CA, Donovan KA, Kip KE, Tofthagen CS (2016) Body image in younger breast cancer survivors: a systematic review. Cancer nurs 39:E39–E58
Tazegül Ü (2018) Sporcularin kişilik özellikleri ile bedenlerini beğenmeleri arasindaki ilişkinin belirlenmesi. Elektronik Sosyal Bilimler Dergisi 17:1518–1526
Cordero MJA, Villar NM, Sánchez MN, Pimentel-Ramírez ML, García-Rillo A, Valverde EG (2015) Breast cancer and body image as a prognostic factor of depression: a case study in México City. Nutr hosp 31:371–379
Prates ACL, Freitas-Junior R, Prates MFO, Veloso MDF, Barros NDM (2017) Influence of body image in women undergoing treatment for breast cancer. Rev Bras Ginecol Obstet 39:175–183
Aslan Ö, Vural H, Kömürcü Ş, Özet A (2006) Kemoterapi Alan Kanser Hastalarina Verilen Eğitimin Kemoterapi Semptomlarina Etkisi. CÜ Hemsirelik Yüksekokulu Dergisi 10:15–28
Brown V, Sitzia J, Richardson A, Hughes J, Hannon H, Oakley C (2001) The development of the Chemotherapy Symptom Assessment Scale (C-SAS): a scale for the routine clinical assessment of the symptom experiences of patients receiving cytotoxic chemotherapy. Int J Nurs Stud 38:497–510
Grogan S, Mechan J (2017) Body image after mastectomy: a thematic analysis of younger women’s written accounts. J Health Psychol 22:1480–1490
Cairo Notari S, Notari L, Favez N, Delaloye JF, Ghisletta P (2017) The protective effect of a satisfying romantic relationship on women’s body image after breast cancer: a longitudinal study. Psychooncology 26:836–842
Moreira H, Canavarro MC (2010) A longitudinal study about the body image and psychosocial adjustment of breast cancer patients during the course of the disease. Euro J Oncol Nurs 14:263–270
Burgess C, Cornelius V, Love S, Graham J, Richards M, Ramirez A (2005) Depression and anxiety in women with early breast cancer: five year observational cohort study. BMJ 330:702
İzci F, Özdem G, İlgün AS, Ağaçayak F, Duymaz T, Erdoğan Z, Alço G, Elbüken F, Öztürk A, Ordu Ç (2020) Pre-treatment and post-treatment anxiety, depression, sleep and sexual function levels in patients with breast cancer. Euro J Breast Health 16:219
Sevinç AI (2015) Erken evre meme kanserinde tedavi seçenekleri. In: IN: AYDıN S, A. T., EDITORS. (ed.) Tüm Yönleriyle Meme Kanseri. Adana: Nobel Kitabevi
Secord PF, Jourard SM (1953) The appraisal of body-cathexis: body-cathexis and the self. J Consult Psychol 17:343–347
Hovardaoğlu S (1993) Vücut algısı ölçeği. Psikiyatri, Psikoloji, Psikofarmakoloji (3P) Dergisi, 1, 26–7
Zigmond AS, Snaith RP (1983) The hospital anxiety and depression scale. Acta Psychiatr Scand 67:361–370
Aydemir O (1997) Hastane anksiyete ve depresyon olcegi Turkce formunun gecerlilik ve guvenilirligi. Turk Psikiyatri Derg 8:187–280
Abudayyak M, Yalçin CÖ, Korkut E (2018) Kemoterapi İle İndüklenmiş Periferal Nöropatinin Tedavisi ve Önlenmesine Yönelik Farmakolojik Yaklaşımlar. FABAD J Pharm Sci 43:113–127
Marupudi NI, Han JE, Li KW, Renard VM, Tyler BM, Brem H (2007) Paclitaxel: a review of adverse toxicities and novel delivery strategies. Expert Opin Drug Saf 6:609–621
Marks DH, Qureshi A, Friedman A (2018) Evaluation of prevention interventions for taxane-induced dermatologic adverse events: a systematic review. JAMA Dermatol 154:1465–1472
Rudd JA, Andrews PLR (2005) Mechanisms of acute, delayed, and anticipatory emesis induced by anticancer therapies. In: Hesketh PJ (ed) Management of Nausea and Vomiting in Cancer and Cancer Treatment. Jones and Bartlett, Sudbury, pp 15–65
Chan YN, Jheng YW, Wang YJ (2021) Chemotherapy-induced peripheral neurotoxicity as a risk factor for poor sleep quality in breast cancer survivors treated with docetaxel. Asia Pac J Oncol Nurs 8(1):68–73
Zangardi MLA (2017) Taxing consequence: taxane acute pain syndrome. JHOP 7(2):80–82
Park SB et al (2011) Early, progressive, and sustained dysfunction of sensory axons underlies paclitaxel-induced neuropathy. Muscle Nerve 43(3):367–374
Villar RR, Fernández SP, Garea CC, Pillado M, Barreiro VB and Martín CG (2017) Quality of life and anxiety in women with breast cancer before and after treatment. Revista Latino-Americana de Enfermagem 25:e2958
Bao T, Basal C, Seluzicki C, Li SQ, Seidman AD, Mao JJ (2016) Long-term chemotherapy-induced peripheral neuropathy among breast cancer survivors: prevalence, risk factors, and fall risk. Breast Cancer Res Treat 159:327–333
Azim H Jr, De Azambuja E, Colozza M, Bines J, Piccart M (2011) Long-term toxic effects of adjuvant chemotherapy in breast cancer. Ann Oncol 22:1939–1947
Gornstein E, Schwarz TL (2014) The paradox of paclitaxel neurotoxicity: Mechanisms and unanswered questions. Neuropharmacology 76:175–183
Pud D (2015) The psychometric properties of the Hebrew version of the Memorial Symptom Assessment Scale (MSAS-Heb) in patients with breast cancer. J Pain Symptom Manage 49:790–795
Guedes TSR, De Oliveira NPD, Holanda AM, Reis MA, Da Silva CP, e Silva BLR, De Camargo Cancela M, De Souza DLB (2018) Body image of women submitted to breast cancer treatment. Asian Pac J Cancer Prev 19:1487
Bergerot CD, Mitchell H-R, Ashing KT, Kim Y (2017) A prospective study of changes in anxiety, depression, and problems in living during chemotherapy treatments: effects of age and gender. Support Care Cancer 25(6):1897–1904
Byar KL, Berger AM, Bakken SL and Cetak MA Impact of adjuvant breast cancer chemotherapy on fatigue, other symptoms, and quality of life. Oncology nursing forum, 2006. Oncology Nursing Society, E18
Oh P-J, Cho J-R (2020) Changes in fatigue, psychological distress, and quality of life after chemotherapy in women with breast cancer: a prospective study. Cancer Nurs 43:E54–E60
Acknowledgements
The authors would like to thank all the participants, the nurses, and administrative staff working in the Hacettepe University Oncology Hospital, Dr. A.Y. Ankara Oncology Hospital, and Ankara City Hospital. Without the participants’ voluntary participation and support of the nurses and administrative staff, this study would not have been possible. The authors also express their thank to head of medical oncology unit Prof. Dr. Ömür Berna Çakmak Öksüzoğlu and nurse Zeynep Sipahi Karslı for their collaboration and great support.
Author information
Authors and Affiliations
Contributions
Gamze Gökçe Ceylan is the first author of this study. She has responsibility in conceptualization, data curation, formal analysis, investigation, methodology, resources, visualization, and writing. Zehra Gök Metin is the co-author of the study. She has responsibility in data curation, methodology, project administration, supervision, validation, and writing—review and editing. The final version of this manuscript is approved by all of the authors.
Corresponding author
Ethics declarations
Ethics approval
Ethical approval was obtained from Hacettepe University Non-Interventional Clinical Research Ethics Committee (2019/06–10), and institutional permissions were obtained from hospital administrations to start the study. All information was collected in accordance with the Declaration of Helsinki.
Consent to participate
Informed consent was obtained from all individual participants included in the study.
Consent for publication
Informed consent was obtained from all individual participants included in the study.
Conflicts of interest
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Gokce Ceylan, G., Gok Metin, Z. Symptom status, body perception, and risk of anxiety and depression in breast cancer patients receiving paclitaxel: a prospective longitudinal study. Support Care Cancer 30, 2069–2079 (2022). https://doi.org/10.1007/s00520-021-06619-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00520-021-06619-6