Abstract
Objectives
Cancer patients constitute an important group in pediatric palliative care. Though the patients’ home is the preferred place of care, little is known about the characteristics of patients attended by units that provide home assistance. Our objective is to describe the characteristics of cancer patients and healthcare delivered by a pediatric palliative care unit with a home hospitalization program.
Methods
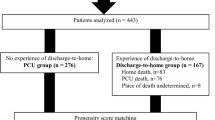
Retrospective study based on clinical records of deceased patients attended by the pediatric palliative care unit of Madrid over 10 years. Data collected included general characteristics, type of cancer, whether they received home assistance, place of death, healthcare delivered (hospitalizations, devices, oncological treatments…), and symptom prevalence.
Results
After excluding 47 patients, the clinical records of 144 patients were analyzed. The median age at referral was 9.4 years (IQR: 5.6–14.1), 61.2% were males; 44.2% had solid non-CNS tumors, 35.4% CNS tumors, and 20.4% hematological malignancies; 137 received home care with 89 not requiring further hospital admissions and 70.1% dying at home. The median follow-up time was 1.6 months (IQR: 0.5–2.9). The most used devices were venous ports (71.4%) and oxygen (49.4%); 53.5% of the patients received oncological support therapies. The most common symptoms were pain (91.8%) dyspnea (49.0%) and fatigue (46.9%).
Conclusions
Home assistance was provided in a high number of patients, with a large proportion needing one or no hospital admissions and 70.1% of them dying at home. Further studies characterizing these patients and the factors which promote early access to palliative care are needed.



Similar content being viewed by others
Data availability
The data used in this article could be available upon request and after approval of the institution where it was taken from (H. Infantil Universitario del Niño Jesús).
Code availability
The code used for this article is available upon request.
References
Crane K (2011) Pediatric palliative care gains recognition. J Natl Cancer Inst 103(19):1432–3. [cited 2018 Aug 3] Available from: https://academic.oup.com/jnci/article-lookup/doi/10.1093/jnci/djr401
Zernikow B, Szybalski K, Hübner-Möhler B, Wager J, Paulussen M, Lassay L et al (2019) Specialized pediatric palliative care services for children dying from cancer: a repeated cohort study on the developments of symptom management and quality of care over a 10-year period. Palliat Med 33(3):381–391
Snaman JM, Kaye EC, Baker JN, Wolfe J (2018) Pediatric palliative oncology: the state of the science and art of caring for children with cancer. Curr Opin Pediatr 30(1):40–48
Wolfe J, Hammel JF, Edwards KE, Duncan J, Comeau M, Breyer J et al (2008) Easing of suffering in children with cancer at the end of life: is care changing? J Clin Oncol 26(10):1717–23. [cited 2019 Jan 10] Available from: http://ascopubs.org/doi/10.1200/JCO.2007.14.0277
Friedrichsdorf SJ, Postier A, Dreyfus J, Osenga K, Sencer S, Wolfe J (2015) Improved quality of life at end of life related to home-based palliative care in children with cancer. J Palliat Med 18(2):143–150
Coller RJ, Nelson BB, Sklansky DJ, Saenz AA, Klitzner TS, Lerner CF et al (2014) Preventing hospitalizations in children with medical complexity: a systematic review. Pediatrics 134(6):e1628-1647
Wolfe J, Grier HE, Klar N, Levin SB, Ellenbogen JM, Salem-Schatz S et al (2000) Symptoms and suffering at the end of life in children with cancer. N Engl J Med 342(5):326–333
Wolfe J, Orellana L, Ullrich C, Cook EF, Kang TI, Rosenberg A et al (2015) Symptoms and distress in children with advanced cancer: prospective patient-reported outcomes from the PediQUEST study. J Clin Oncol 33(17):1928–1935
Hechler T, Blankenburg M, Friedrichsdorf SJ, Garske D, Hübner B, Menke A et al (2008) Parents’ perspective on symptoms, quality of life, characteristics of death and end-of-life decisions for children dying from cancer. Klin Padiatr 220(3):166–174
Goldman A, Hewitt M, Collins GS, Childs M, Hain R, United Kingdom Children’s Cancer Study Group/Paediatric Oncology Nurses’ Forum Palliative Care Working Group (2006) Symptoms in children/young people with progressive malignant disease: United Kingdom Children’s Cancer Study Group/Paediatric Oncology Nurses Forum survey. Pediatrics. 117(6):e1179-1186
Brock KE, Snaman JM, Kaye EC, Bower KA, Weaver MS, Baker JN et al (2019) Models of pediatric palliative oncology outpatient care—benefits, challenges, and opportunities. JOP 15(9):476–87. [cited 2019 Oct 9] Available from: https://ascopubs.org/doi/10.1200/JOP.19.00100
Craig F, Abu-SaadHuijer H, Benini F, Kuttner L, Wood C, Feraris PC et al (2008) IMPaCCT: standards of paediatric palliative care. Schmerz 22(4):401–408
Brock KE, Steineck A, Twist CJ (2016) Trends in end-of-life care in pediatric hematology, oncology, and stem cell transplant patients. Pediatr Blood Cancer 63(3):516–522
Kassam A, Skiadaresis J, Alexander S, Wolfe J (2015) Differences in end-of-life communication for children with advanced cancer who were referred to a palliative care team. Pediatr Blood Cancer 62(8):1409–1413
Pritchard M, Burghen E, Srivastava DK, Okuma J, Anderson L, Powell B et al (2008) Cancer-related symptoms most concerning to parents during the last week and last day of their child’s life. Pediatrics 121(5):e1301-1309
Hui D, Didwaniya N, Vidal M, Shin SH, Chisholm G, Roquemore J et al (2014) Quality of end-of-life care in patients with hematologic malignancies: a retrospective cohort study. Cancer 120(10):1572–1578
Snaman JM, Kaye EC, Lu JJ, Sykes A, Baker JN (2017) Palliative care involvement is associated with less intensive end-of-life care in adolescent and young adult oncology patients. J Palliat Med. 20(5):509–16. [cited 2019 Oct 9] Available from: http://www.liebertpub.com/doi/10.1089/jpm.2016.0451
Haines ER, Frost AC, Kane HL, Rokoske FS (2018) Barriers to accessing palliative care for pediatric patients with cancer: a review of the literature. Cancer 124(11):2278–2288
World Health Organization. WHO definition of palliative care. Available on: http://www.who.int/cancer/palliative/definition/en/. Access Nov 2017
Cherny N, Catane R, Schrijvers D, Kloke M, Strasser F (2010) European Society for Medical Oncology (ESMO) Program for the integration of oncology and Palliative Care: a 5-year review of the Designated Centers’ incentive program. Ann Oncol 21(2):362–369
Smith TJ, Temin S, Alesi ER, Abernethy AP, Balboni TA, Basch EM et al (2012) American Society of Clinical Oncology provisional clinical opinion: the integration of palliative care into standard oncology care. J Clin Oncol 30(8):880–887
Mark Melissa San Julian, Yang Gang, Ding Lili, Norris Robin E, Thienprayoon Rachel (2019) Location of death and end-of-life characteristics of young adults with cancer treated at a pediatric hospital. J Adolesc Young Adult Oncol 8(4):417–422. https://doi.org/10.1089/jayao.2018.0123
Bluebond-Langner M, Beecham E, Candy B, Langner R, Jones L (2013) Preferred place of death for children and young people with life-limiting and life-threatening conditions: a systematic review of the literature and recommendations for future inquiry and policy. Palliat Med 27(8):705–713
Craig F, Henderson EM, Bluebond-Langner M (2015) Management of respiratory symptoms in paediatric palliative care. Curr Opin Support Palliat Care 9(3):217–26. [cited 2018 Sep 11] Available from: http://content.wkhealth.com/linkback/openurl?sid=WKPTLP:landingpage&an=01263393-201509000-00005
Weltgesundheitsorganisation (ed) (2012) WHO guidelines on the pharmacological treatment of persisting pain in children with medical illnesses. World Health Organization, Geneva, 166 p
Stachelek GC, Terezakis SA, Ermoian R (2019) Palliative radiation oncology in pediatric patients. Ann Palliat Med [cited 2019 Oct 9];8(3):285–92. Available from: http://apm.amegroups.com/article/view/25922/24662
Ullrich CK, Mayer OH (2007) Assessment and management of fatigue and dyspnea in pediatric palliative care. Pediatr Clin N Am 54(5):735–56. [cited 2018 Sep 11] Available from: http://linkinghub.elsevier.com/retrieve/pii/S0031395507001150
Pereira J, Phan T (2004) Management of bleeding in patients with advanced cancer. Oncologist 9(5):561–570
Clerici CA, Veneroni L, Giacon B, Mariani L, Fossati-Bellani F (2009) Complementary and alternative medical therapies used by children with cancer treated at an Italian pediatric oncology unit. Pediatr Blood Cancer 53(4):599–604
Cheng L, Wang L, He M, Feng S, Zhu Y, Rodgers C (2018) Perspectives of children, family caregivers, and health professionals about pediatric oncology symptoms: a systematic review. Support Care Cancer 26(9):2957–2971
Collins JJ, Byrnes ME, Dunkel IJ, Lapin J, Nadel T, Thaler HT et al (2000) The measurement of symptoms in children with cancer. J Pain Symptom Manage 19(5):363–377
Madden K, MagnoCharone M, Mills S, Dibaj S, Williams JL, Liu D et al (2019) Systematic symptom reporting by pediatric palliative care patients with cancer: a preliminary report. J Palliat Med 22(8):894–901
Collins JJ, Devine TD, Dick GS, Johnson EA, Kilham HA, Pinkerton CR et al (2002) The measurement of symptoms in young children with cancer: the validation of the Memorial Symptom Assessment Scale in children aged 7–12. J Pain Symptom Manage 23(1):10–16
Snaman JM, Baker JN, Ehrentraut JH, Anghelescu DL (2016) Pediatric oncology: managing pain at the end of life. Paediatr Drugs 18(3):161–180
Author information
Authors and Affiliations
Contributions
I. de Noriega has participated in the collection, analysis of data, and writing of the manuscript; A. García-Salido has participated in the methodological approach and structuring of the manuscript; R. Martino has participated in the conceptualization and design of the study and its review; B. Herrero has participated in the conceptualization and design of the study and its review.
Corresponding author
Ethics declarations
Ethics approval
This study follows the approved ethical procedures of H. Infantil Universitario del Niño Jesús, an institution from where the data was collected.
Consent to participate
N/A.
Consent for publication
N/A.
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Noriega, Í.d., García-Salido, A., Martino, R. et al. Palliative home-based care to pediatric cancer patients: characteristics and healthcare delivered. Support Care Cancer 30, 59–67 (2022). https://doi.org/10.1007/s00520-021-06412-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00520-021-06412-5