Abstract
Purpose
To investigate the incidence and risk factors for oral mucositis (OM) in patients with childhood cancer undergoing chemotherapy.
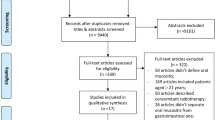
Methods
Eight hundred and twenty-nine cycles of chemotherapy were evaluated in 112 patients with childhood cancer undergoing chemotherapy. Chemotherapy protocol, hematological, hepatic, and renal function parameters were collected and compared to presence and severity of OM, as graded by the World Health Organization (WHO) scale. Patients received counseling on oral hygiene and those who presented with OM (grade ≥1) received photobiomodulation therapy (PBMT).
Results
Age ranged from 0 to 17 years (mean/SD, 8.58 ± 5.05) and fifty-one patients (45.54%) were females. The most common baseline diseases were leukemia (51%) followed by sarcomas (23%) and lymphomas (18%). Eight hundred and twenty-nine cycles of chemotherapy were evaluated, and OM was diagnosed in 527 cycles (63.57%). Higher incidence and severity of OM was observed in protocols using high-dose methotrexate (MTX-HD), MTX-HD cyclophosphamide/doxorubicin combination, and MTX-HD combined with cyclophosphamide (p <0.001). Patients with severe OM had lower levels of leukocytes (p = 0.003), hemoglobin (p = 0.005), platelets (p = 0.034), and higher levels of total bilirubin (p = 0.027), alanine aminotransferase (ALT) (p = 0.001), and creatinine (p = 0.007).
Conclusion
The study contributes to the elucidation of the risk factors for OM in pediatric cancer patients. Chemotherapy protocols using MTX-HD, MTX-HD associated with doxorubicin and cyclophosphamide, and MTX-HD and cyclophosphamide a have higher incidence of severe grades of OM. Other toxicities such as hematological, hepatic, and renal also developed in patients with OM.

Similar content being viewed by others
References
Ward ZJ, Yeh JM, Bhakta N, Frazier AL, Atun R (2019) Estimating the total incidence of global childhood cancer: a simulation-based analysis. Lancet Oncol 20(4):483–493. https://doi.org/10.1016/S1470-2045(18)30909-4
Malkin D, Himelfarb J (2019) Issues in pediatric cancers. Cancer prevention and screening: concepts, principles and controversies. (ed) Early diagnosis 1rd edn. John Wiley & Sons, Inc pp 19-29
Rühle A, Huber PE, Saffrich R, Lopez Perez R, Nicolay NH (2018) The current understanding of mesenchymal stem cells as potential attenuators of chemotherapy-induced toxicity. Int J Cancer 143(11):2628–2639. https://doi.org/10.1002/ijc.31619
Al-Dasooqi N, Sonis ST, Bowen JM, Bateman E, Blijlevens N, Gibson RJ, Logan MR, Nair RJ, Stringer AM, Yazbeck R, Elad S, Lalla RV (2013) Emerging evidence on the pathobiology of mucositis. Support Care Cancer 21(7):2075–2083. https://doi.org/10.1007/s00520-013-1810-y
Bezinelli LM, de Paula EF, da Graça Lopes RM et al (2014) Cost-effectiveness of the introduction of specialized oral care with laser therapy in hematopoietic stem cell transplantation. Hematol Oncol 32(1):31–39. https://doi.org/10.1002/hon.2050
Migliorati C, Yan H, Lalla RV, Antunes HS, Estilo CL, Hodgson B, Lopes NNF, Schubert MM, Bowen J, Elad S (2012) Systematic review of laser and other light therapy for the management of oral mucositis in cancer patients. Support Care Cancer 21(1):333–341. https://doi.org/10.1007/s00520-012-1605-6
Mazhari F, Shirazi AS, Shabzendehdar M (2019) Management of oral mucositis in pediatric patients receiving cancer therapy: a systematic review and meta-analysis. Pediatr Blood Cancer 66(3):e27403. https://doi.org/10.1002/pbc.27403
Hong CHL, Gueiro LA, Fulton JS, Cheng KKF, Kandwal A, Galiti D, Fall-Dickson JM, Johansen J, Ameringer S, Kataoka T, Weikel D, Eilers J, Ranna V, Vaddi A, Lalla RJ, Bossi P, Elad S (2019) Systematic review of basic oral care for the management of oral mucositis in cancer patients and clinical practice guidelines. Support Care Cancer 27(10):3949–3967. https://doi.org/10.1007/s00520-019-04848-4
Zadik Y, Arany PR, Fregnani ER et al (2019) Systematic review of photobiomodulation for the management of oral mucositis in cancer patients and clinical practice guidelines. Support Care Cancer 27(10):3969–3983. https://doi.org/10.1007/s00520-019-04890-2
Miranda-Silva W, Gomes-Silva W, Zadik Y et al (2020) Mucositis Study Group of the Multinational Association of Supportive Care in Cancer / International Society for Oral Oncology (MASCC/ISOO).MASCC/ISOO clinical practice guidelines for the management of mucositis: sub-analysis of current interventions for the management of oral mucositis in pediatric cancer patients. Support Care Cancer. https://doi.org/10.1007/s00520-020-05803-4
Correa MEP, Cheng KKF, Chiang K et al (2019) Systematic review of oral cryotherapy for the management of oral mucositis in cancer patients and clinical practice guidelines. Support Care Cancer 28(5):2449–2456. https://doi.org/10.1007/s00520-019-05217-x
Allen G, Logan R, Revesz T, Keefe D, Gue S (2018) The prevalence and investigation of risk factors of oral mucositis in a pediatric oncology inpatient population; a prospective study. J Pediatr Hematol Oncol 40(1):15–21. https://doi.org/10.1097/MPH.0000000000000970
Nishii M, Soutome S, Kawakita A, Youtori H, Iwata E, Akashi M, Hasegawa T, Kojima Y, Funahara M, Umeda M, Komori T (2020) Factors associated with severe oral mucositis and candidiasis in patients undergoing radiotherapy for oral and oropharyngeal carcinomas: a retrospective multicenter study of 326 patients. Support Care Cancer 28(3):1069–1075. https://doi.org/10.1007/s00520-019-04885-z
Shouval R, Kouniavski E, Fein J, Danylesko I, Shem-Tov N, Geva M, Yerushalmi R, Avichai S, Nagler A (2019) Risk factors and implications of oral mucositis in recipients of allogeneic hematopoietic stem cell transplantation. Eur J Haematol 4(103):402–409. https://doi.org/10.1111/ejh.13299
Basile D, Di Nardo P, Corvaja C, Garattini SK, Pelizzari G, Lisanti C, Bortot L, Da Ros L, Bartoletti M, Borghi M, Gerratana L, Lombardi D, Puglisi F (2019) Mucosal injury during anti-cancer treatment: from pathobiology to bedside. Cancers 11:857. https://doi.org/10.3390/cancers11060857
Liu SG, Gao C, Zhang RD, Zhao XX, Cui L, Li WJ, Chen ZP, Yue ZX, Zhang YY, Wu MY, Wang JX, Li ZG, Zheng HY (2017) Polymorphisms in methotrexate transporters and their relationship to plasma methotrexate levels, toxicity of high-dose methotrexate, and outcome of pediatric acute lymphoblastic leukemia. Oncotarget 8(23):37761–37772. https://doi.org/10.18632/oncotarget.17781
Common Terminology Criteria for Adverse Events (CTCAE) Version 5.0CTCAE v5.0 ( 2017). https://ctep.cancer.gov/
Weissheimer C, Curra M, Gregianin LJ, Daudt LE, Wagner VP, Martins MAT, Martins MD (2017) New photobiomodulation protocol prevents oral mucositis in hematopoietic stem cell transplantation recipients—a retrospective study. Lasers Med Sci 32(9):2013–2021. https://doi.org/10.1007/s10103-017-2314-7
Hurrell L, Burgoyne L, Logan R, Revesz T, Gue S (2019) The management of pediatric oncology inpatients with oral mucositis. J Pediatr Hematol Oncol 41(8):e510–e516. https://doi.org/10.1097/MPH.0000000000001546
Ip WY, Epstein JB et al (2014) Oral mucositis in pediatric patients after chemotherapy for cancer. Hong Kong Med J 20(6):S4–S8. https://doi.org/10.5005/jp-journals-10005-1633
Cheng KK, Lee V, Li CH et al (2011) Incidence and risk factors of oral mucositis in paediatric and adolescent patients undergoing chemotherapy. Oral Oncol 47(3):153–162. https://doi.org/10.1016/j.oraloncology.2010.11.019
Ribeiro I, de Andrade Lima Neto E, Valença AM (2019) Chemotherapy in pediatric oncology patients and the occurrence of oral mucositis. Int J Clin Pediatr Dent 12(4):261–267. https://doi.org/10.5005/jp-journals-10005-163
Osmanoglu Yurdakul Z, Esenay FI (2019) Complementary and integrative health methods used for the treatment of oral mucositis in children with cancer in Turkey. J Spec Pediatr Nurs 24(3):e12260. https://doi.org/10.1111/jspn.12260
Damascena LCL, de Lucena NNN, Ribeiro ILA, Pereira TL, Lima-Filho LMA, Valença AMG (2020) Severe oral mucositis in pediatric cancer patients: survival analysis and predictive factors. Int J Environ Res Public Health 17(4):1235
Anschau F, Webster J, Capra MEZ, de Azeredo da Silva ALF, Stein AT (2020) Efficacy of low-level laser for treatment of cancer oral mucositis: a systematic review and meta-analysis. Lasers Med Sci 34(6):1053–1062
Marín-Conde F, Castellanos-Cosano L, Pachón-Ibañez J, Serrera-Figallo MA, Gutiérrez-Pérez JL, Torres-Lagares D (2019) Photobiomodulation with low-level laser therapy reduces oral mucositis caused by head and neck radio-chemotherapy: prospective randomized controlled trial. Int J Oral Maxillofac Surg 48(7):917–923. https://doi.org/10.1016/j.ijom.2018.12.006
Rodrigues GH, Jaguar GC, Alves FA et al (2017) Variability of high dose melphalan exposure on oral mucositis in patients undergoing prophylactic low-level laser therapy. Lasers Med Sci 32(5):1089–1095. https://doi.org/10.1007/s10103-017-2211-0
Meeske KA, Ji L, Freyer DR et al (2015) Comparative toxicity by sex among children treated for acute lymphoblastic leukemia: a report from the Children’s Oncology Group. Pediatr Blood Cancer 62(12):2140–2149. https://doi.org/10.1002/pbc.25628
Bartlett NL, Wilson WH, Jung SH et al (2019) Dose-adjusted EPOCH-R compared with R-CHOP as frontline therapy for diffuse large B-cell lymphoma: clinical outcomes of the phase III Intergroup Trial Alliance/CALGB 50303. J Clin Oncol 37(21):1790–1799. https://doi.org/10.1200/JCO.18.01994
Heil SG (2019) Genetics of high-dose methotrexate-induced oral mucositis: current perspectives. Pharmacogenomics. 20(9):621–623. https://doi.org/10.2217/pgs-2019-0062
den Hoed MA, Lopez-Lopez E, te Winkel ML, et al (2015) Genetic and metabolic determinants of methotrexate-induced mucositis in pediatric acute lymphoblastic leukemia. Pharmacogenomics J. (2015):248–254. https://doi.org/10.1038/tpj.2014.63
Oosterom N, Griffioen PH, den Hoed MAH et al (2018) Global methylation in relation to methotrexate-induced oral mucositis in children with acute lymphoblastic leukemia. PLoS One 13(7):e0199574. https://doi.org/10.1371/journal.pone.0199574
Rivankar S (2017) An overview of doxorubicin formulations in cancer therapy. J Cancer Res Ther 10(4):853–858. https://doi.org/10.4103/0973-1482.139267
Bajpai J, Chandrasekharan A, Talreja V et al (2017) Outcomes in non-metastatic treatment naive extremity osteosarcoma patients treated with a novel non-high dose methotrexate-based, dose-dense combination chemotherapy regimen 'OGS-12'. Eur J Cancer 85:49–58. https://doi.org/10.1016/j.ejca.2017.08.013
Senerchia AA, Macedo CR, Ferman S et al (2017) Results of a randomized, prospective clinical trial evaluating metronomic chemotherapy in nonmetastatic patients with high-grade, operable osteosarcomas of the extremities: a report from the Latin American Group of Osteosarcoma Treatment. Cancer. 123(6):1003–1010. https://doi.org/10.1002/cncr.30411
MCTiernan A, Jinks RC, Sydes MR, Uscinska B, Hook JM, van Glabbeke M, et al (2012) Presence of chemotherapy-induced toxicity predicts improved survival in patients with localized extremity osteosarcoma treated with doxorubicin and cisplatin: A report from the European Osteosarcoma Intergroup. Eur J Cancer 48(5): 703-712. doi: https://doi.org/10.1016/j.ejca.2011.09.012
Ten Berg S, Loeffen EAH, van de Wetering MD et al (2019) Development of pediatric oncology supportive care indicators: evaluation of febrile neutropenia care in the north of the Netherlands. Pediatr Blood Cancer 66(2):e27504. https://doi.org/10.1002/pbc.27504
Freifeld AG, Bow EJ, Sepkowitz KA et al (2011) Clinical practice guideline for the use of antimicrobial agents in neutropenic patients with cancer: 2010 update by the infectious diseases society of america. Clin Infect Dis 52(4):e56–e93. https://doi.org/10.1093/cid/cir073
Mendonça RM, Md A, Levy CE et al (2015) Oral mucositis in pediatric acute lymphoblastic leukemia patients: evaluation of microbiological and hematological factors. Pediatr Hematol Oncol 32(5):322–330. https://doi.org/10.3109/08880018.2015.1034819
Denton CC, Rawlins YA, Oberley MJ, Bhojwani D, Orgel E (2018) Predictors of hepatotoxicity and pancreatitis in children and adolescents with acute lymphoblastic leukemia treated according to contemporary regimens. Pediatr Blood Cancer 65(3). https://doi.org/10.1002/pbc.26891
Fevery J (2008) Bilirubin in clinical practice: a review. Liver Int 28(5):592–605. https://doi.org/10.1111/j.1478-3231.2008.01716.x
Björnsson HK, Olafsson S, Bergmann OM, Björnsson ES (2016) A prospective study on the causes of notably raised alanine aminotransferase (ALT). Scand J Gastroenterol 51(5):594–600. https://doi.org/10.3109/00365521.2015.1121516
Xu WQ, Zhang LY, Chen XY et al (2014) Serum creatinine and creatinine clearance for predicting plasma methotrexate concentrations after high-dose methotrexate chemotherapy for the treatment for childhood lymphoblastic malignancies. Cancer Chemother Pharmacol 73(1):79–86. https://doi.org/10.1007/s00280-013-2319-2
Cheng KK (2008) Association of plasma methotrexate, neutropenia, hepatic dysfunction, nausea/vomiting and oral mucositis in children with cancer. Eur J Cancer Care (Engl) 17(3):306–311. https://doi.org/10.1111/j.1365-2354.2007.00843.x
Valer JB, Curra M, Gabriel AF, Schmidt TR, Ferreira MBC, Roesler R, Evangelista JMC, Martins MAT, Gregianin L, Martins MD (2020) Oral mucositis in childhood cancer patients receiving high-dose methotrexate: prevalence relationship with other toxicities and methotrexate elimination. Int J Paediatr Dent (Aug 20). https://doi.org/10.1111/ipd.12718
Acknowledgments
The authors are grateful to all the members of the Pediatric Oncology Service of Porto Alegre Clinical Hospital (HCPA/UFRGS) for support during the development of the present research.
Availability of data and material
Authors have full control of all primary data and allow the journal to review the data.
Code availability
Not applicable
Funding
This study was supported by the PRONON/Ministry of Health, Brazil (grant no. 25000.056.976/2015-52); Postgraduate Research Group of Porto Alegre Clinics Hospital (GPPG/FIPE: 2016-0608), Brazilian National Council for Scientific and Technological Development (CNPq student scholarship), Children’s Cancer Institute (student scholarship), and Coordenação de Aperfeiçoamento de Pessoal de Nível Superior-Brasil (CAPES)- finance code 001. Rafael Roesler and Manoela Domingues Martins are research fellows funded by the Brazilian National Council for Scientific and Technological Development (CNPq).
Author information
Authors and Affiliations
Contributions
Marina Curra: conceptualization; data curation; formal analysis; investigation; writing—original draft; writing—review and editing. Amanda F. Gabriel: conceptualization; data curation; formal analysis; investigation; writing—original draft; writing—review and editing. Maria Beatriz C. Ferreira: conceptualization; writing—review and editing. Marco Antonio T. Martins: conceptualization; data curation; writing—original draft; writing—review and editing. André T. Brunetto: conceptualization; data curation; formal analysis; writing—review and editing. Lauro J. Gregianin: conceptualization; data curation; formal analysis; writing—review and editing. Manoela D. Martins: conceptualization; data curation; formal analysis; investigation; methodology; project administration; writing original draft; writing—review and editing.
Corresponding author
Ethics declarations
Ethics approval
Institutional Human Research Ethics Committee (HCPA protocol 14-0581 and CAEE 40921215.6.0000.5327).
Consent to participate
Patients and/or their legal guardians signed an informed consent.
Consent for publication
Patients and/or their legal guardians signed an informed consent with consent for publication.
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Curra, M., Gabriel, A.F., Ferreira, M.B.C. et al. Incidence and risk factors for oral mucositis in pediatric patients receiving chemotherapy. Support Care Cancer 29, 6243–6251 (2021). https://doi.org/10.1007/s00520-021-06199-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00520-021-06199-5