Abstract
Purpose
To assess the proportion of breast cancer patients treated with total mastectomy who are interested in undergoing breast reconstruction, the factors associated with their desire to undergo this procedure, and the motives stated for their decision.
Methods
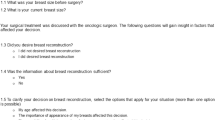
Women with stage I–III breast cancer, public health insurance, and history of total mastectomy treated at a center in Monterrey, Mexico, were invited to answer a series of questionnaires regarding their clinical and demographic characteristics, information received about breast reconstruction, body image, and relationship satisfaction.
Results
A total of 100 patients were interviewed, of which 68% desired to undergo breast reconstruction. Only 35% recalled talking about this procedure with a physician and 85% claimed not to have enough information to make an informed decision. Those who desired breast reconstruction were younger (p < 0.001), more likely to be in a relationship (p = 0.025), and had a higher probability of having talked to a physician about the procedure (p = 0.019). Furthermore, they felt less sexually attractive (p < 0.001), more deformed (p = 0.006), and less feminine (p = 0.005) since the mastectomy. The main motives to undergo this procedure were to have breast symmetry and greater freedom on which clothes to wear, while the main deterrent was the high economical cost.
Conclusions
Insufficient information about the procedure and high economical cost were identified as potential barriers to undergo breast reconstruction. The findings of this study emphasize the pressing need to optimize patient care by providing information in a standardized manner and improving access to breast reconstruction within the Mexican public healthcare system.
Similar content being viewed by others
Data availability
All data generated or analyzed during this study are available upon reasonable request to the corresponding author.
References
Bray F, Ferlay J, Soerjomataram I, Siegel RL, Torre LA, Jemal A (2018) Global cancer statistics 2018: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin 68:394–424. https://doi.org/10.3322/caac.21492
Feigelson HS, James TA, Single RM, Onitilo AA, Aiello Bowles EJ, Barney T, Bakerman JE, McCahill LE (2013) Factors associated with the frequency of initial total mastectomy: results of a multi-institutional study. J Am Coll Surg 216:966–975. https://doi.org/10.1016/j.jamcollsurg.2013.01.011
Goss PE, Lee BL, Badovinac-Crnjevic T, Strasser-Weippl K, Chavarri-Guerra Y, Louis JS, Villarreal-Garza C, Unger-Saldaña K, Ferreyra M, Debiasi M, Liedke PER, Touya D, Werutsky G, Higgins M, Fan L, Vasconcelos C, Cazap E, Vallejos C, Mohar A, Knaul F, Arreola H, Batura R, Luciani S, Sullivan R, Finkelstein D, Simon S, Barrios C, Kightlinger R, Gelrud A, Bychkovsky V, Lopes G, Stefani S, Blaya M, Souza FH, Santos FS, Kaemmerer A, de Azambuja E, Zorilla AFC, Murillo R, Jeronimo J, Tsu V, Carvalho A, Gil CF, Sternberg C, Dueñas-Gonzalez A, Sgroi D, Cuello M, Fresco R, Reis RM, Masera G, Gabús R, Ribeiro R, Knust R, Ismael G, Rosenblatt E, Roth B, Villa L, Solares AL, Leon MX, Torres-Vigil I, Covarrubias-Gomez A, Hernández A, Bertolino M, Schwartsmann G, Santillana S, Esteva F, Fein L, Mano M, Gomez H, Hurlbert M, Durstine A, Azenha G (2013) Planning cancer control in Latin America and the Caribbean. Lancet Oncol 14:391–436. https://doi.org/10.1016/S1470-2045(13)70048-2
Tsai H-Y, Kuo RN-C, Chung K (2017) Quality of life of breast cancer survivors following breast-conserving therapy versus mastectomy: a multicenter study in Taiwan. Jpn J Clin Oncol 47:909–918. https://doi.org/10.1093/jjco/hyx099
Enien M, Ibrahim N, Makar W, Darwish D, Gaber M (2018) Health-related quality of life: Impact of surgery and treatment modality in breast cancer. J Cancer Res Ther 14:957–963. https://doi.org/10.4103/0973-1482.183214
Aerts L, Christiaens MR, Enzlin P, Neven P, Amant F (2014) Sexual functioning in women after mastectomy versus breast conserving therapy for early-stage breast cancer: a prospective controlled study. Breast 23:629–636. https://doi.org/10.1016/j.breast.2014.06.012
Archangelo SCV, Sabino Neto M, Veiga DF, Garcia EB, Ferreira LM. Sexuality, depression and body image after breast reconstruction. Clinics (Sao Paulo). 2019 May 30;74:e883. https://doi.org/10.6061/clinics/2019/e883. PMID: 31166474; PMCID: PMC6542498
Fanakidou I, Zyga S, Alikari V, Tsironi M, Stathoulis J, Theofilou P (2018) Mental health, loneliness, and illness perception outcomes in quality of life among young breast cancer patients after mastectomy: the role of breast reconstruction. Qual Life Res 27:539–543. https://doi.org/10.1007/s11136-017-1735-x
Cortés-Flores AO, Vargas-Meza A, Morgan-Villela G, Jiménez-Tornero J, del Valle CJZF, Solano-Genesta M, Miranda-Ackerman RC, Vázquez-Reyna I, García-González LA, Cervantes-Cardona GA, Cervantes-Guevara G, Fuentes-Orozco C, González-Ojeda A (2017) Sexuality among women treated for breast cancer: a survey of three surgical procedures. Aesthetic Plast Surg 41:1275–1279. https://doi.org/10.1007/s00266-017-0960-6
Wong SM, Chun YS, Sagara Y, Golshan M, Erdmann-Sager J (2019) National patterns of breast reconstruction and nipple-sparing mastectomy for breast cancer, 2005–2015. Ann Surg Oncol 26:3194–3203. https://doi.org/10.1245/s10434-019-07554-x
Song WJ, Kang SG, Kim EK, Song SY, Lee JS, Lee JH, Jin US (2020) Current status of and trends in post-mastectomy breast reconstruction in Korea. Arch Plast Surg 47:118–125. https://doi.org/10.5999/aps.2019.01676
Jeevan R, Cromwell DA, Browne JP, Caddy CM, Pereira J, Sheppard C, Greenaway K, van der Meulen JHP (2014) Findings of a national comparative audit of mastectomy and breast reconstruction surgery in England. J Plast Reconstr Aesthetic Surg 67:1333–1344. https://doi.org/10.1016/j.bjps.2014.04.022
Ishak A, Yahya MM, Halim AS (2018) Breast reconstruction after mastectomy: a survey of surgeons’ and patients’ perceptions. Clin Breast Cancer 18:e1011–e1021. https://doi.org/10.1016/j.clbc.2018.04.012
Martínez RSP, Segura CÁR, SA AV, Mateus LG (2012) Caracterización de los tiempos de atención y de mujeres con cáncer de mama que asistieron a un hospital de tercer nivel, 2005-2009. Rev Fac Nac Salud Pública 30:183–191
Connors SK, Goodman MS, Myckatyn T, Margenthaler J, Gehlert S (2016) Breast reconstruction after mastectomy at a comprehensive cancer center. Springerplus 5:955. https://doi.org/10.1186/s40064-016-2375-2
Zahedi S, Colvill K, Lopez M, Phillips LG (2019) Implications of demographics and socioeconomic factors in breast cancer reconstruction. Ann Plast Surg 83:388–391. https://doi.org/10.1097/SAP.0000000000001919
Brennan ME, Spillane AJ (2013) Uptake and predictors of post-mastectomy reconstruction in women with breast malignancy-systematic review. Eur J Surg Oncol 39:527–541. https://doi.org/10.1016/j.ejso.2013.02.021
Haddad Tame JL, Torres Gómez B, Bello Santamaría JA, Sánchez Forgach E, Ruiz Morales S, Chávez Abraham V et al (2001) Reconstrucción mamaria en el Servicio de Cirugía Plástica del Hospital General de México, 1995-2000. Rev Médica Del Hosp Gen México 64:210–219
López Hernández PI, Priego Álvarez HR, Sylvie C, Noygues B, Ramos GA (2015) ¿Por qué las mujeres mastectomizadas no recurren a la reconstrucción mamaria en el sistema de seguridad social? Psicol y Salud 25:253–260
Hopwood P, Fletcher I, Lee A, Al GS (2001) A body image scale for use with cancer patients. Eur J Cancer 37:189–197. https://doi.org/10.1016/S0959-8049(00)00353-1
Sabastian J, Manos D, Bueno MJ, Mateos N (2007) Imagen corporal y autoestima en mujeres con cáncer de mama participantes en un programa de intervención psicosocial. Clin y Salud 18:137–161
Hendrick SS (1988) A generic measure of relationship satisfaction. J Marriage Fam 50:93. https://doi.org/10.2307/352430
Moral dela Rubia J (2008) Validación de la escala de valoracion de la relacion en una muestra mexicana. Rev Electron Metologia Apl 13:1–12. https://doi.org/10.17811/rema.13.1.2008.1-12
Miaja Avila M, Moral de la Rubia J, Villarreal-Garza C (2018) Fase cualitativa del desarrollo de una Escala de Motivos a favor y en contra de la Reconstrucción Mamaria (EMRM). Psicooncología 15:327–344. https://doi.org/10.5209/psic.68249
Moral De La Rubia J, Miaja Avila M, Bajonero Canónico P, Villarreal Garza C (2019) Psychometric properties of the questionnaire of motives for and against breast reconstruction. Psicooncologia 16:287–313. https://doi.org/10.5209/psic.65592
Keith DJW, Walker MB, Walker LG, Heys SD, Sarkar TK, Hutcheon AW, Eremin O (2003) Women who wish breast reconstruction: characteristics, fears, and hopes. Plast Reconstr Surg 111:1051–1056. https://doi.org/10.1097/01.PRS.0000046247.56810.40
Aráuz Siles KD, Armas Machado EE, Herdocia Baus G, Tercero Madriz FR (2014) Percepción de las mujeres mastectomizadas sobre su condición física y la necesidad de construcción mamaria postmastectomía, HEODRA, 2004-2011. Universidad Nacional Autónoma de Nicaragua, León
Ogrodnik A, MacLennan S, Weaver D, James T (2017) Barriers to completing delayed breast reconstruction following mastectomy: a critical need for patient and clinician education. J Cancer Educ 32:700–706. https://doi.org/10.1007/s13187-016-1046-x
Sergesketter AR, Thomas SM, Lane WO, Shammas RL, Greenup RA, Hollenbeck ST (2019) The influence of marital status on contemporary patterns of postmastectomy breast reconstruction. J Plast Reconstr Aesthetic Surg 72:795–804. https://doi.org/10.1016/j.bjps.2018.12.012
Adachi K, Ueno T, Fujioka T, Fujitomi Y, Ueo H (2007) Psychosocial factors affecting the therapeutic decision-making and postoperative mood states in Japanese breast cancer patients who underwent various types of surgery: body image and sexuality. Jpn J Clin Oncol 37:412–418. https://doi.org/10.1093/jjco/hym041
Flitcroft K, Brennan M, Spillane A (2017) Making decisions about breast reconstruction: a systematic review of patient-reported factors influencing choice. Qual Life Res 26:2287–2319. https://doi.org/10.1007/s11136-017-1555-z
Wilkins EG, Alderman AK (2004) Breast reconstruction practices in North America: current trends and future priorities. Semin Plast Surg 18:149–155. https://doi.org/10.1055/s-2004-829049
Offodile AC, Guo L (2016) Disparate British breast reconstruction utilization: is universal coverage sufficient to ensure expanded care? Plast Reconstr Surg - Glob Open 4:e738. https://doi.org/10.1097/GOX.0000000000000762
Figueroa-Padilla J, Soto-Perez-de-Celis E, Maciel-Miranda A, Vargas-Salas D, Santamaria E, Esparza-Arias N, Gutiérrez-Zacarías LM, Cabrera-Galeana P, Bargalló-Rocha E (2018) Implementation of a microsurgical breast reconstruction program in Mexico. Microsurgery 38:831–833. https://doi.org/10.1002/micr.30383
Héquet D, Zarca K, Dolbeault S, Couturaud B, Ngô C, Fourchotte V, de la Rochefordière A, Féron JG, Fitoussi A, Bélichard C, Reyal F, Laki F, Hajage D, Sigal B, Asselain B, Alran S, Institut Curie Breast Cancer Group, Roman Rouzier (2013) Reasons of not having breast reconstruction: a historical cohort of 1937 breast cancer patients undergoing mastectomy. Springerplus 2:325. https://doi.org/10.1186/2193-1801-2-325
Lardi AM, Myrick ME, Haug M, Schaefer DJ, Bitzer J, Simmen U, Güth U (2013) The option of delayed reconstructive surgery following mastectomy for invasive breast cancer: why do so few patients embrace this offer? Eur J Surg Oncol 39:36–43. https://doi.org/10.1016/j.ejso.2012.08.010
Cárdenas-Sánchez J, Erazo Valle-Solís AA, Arce-Salinas C, Bargalló-Rocha JE, Bautista-Piña V, Cervantes-Sánchez G et al (2019) Consenso Mexicano sobre diagnóstico y tratamiento del cáncer mamario. Octava revisión. Colima 2019. Gac Mex Oncol 18:141–231. https://doi.org/10.24875/j.gamo.M19000180
Momoh AO, Griffith KA, Hawley ST, Morrow M, Ward KC, Hamilton AS, Shumway D, Katz SJ, Jagsi R (2019) Patterns and correlates of knowledge, communication, and receipt of breast reconstruction in a modern population-based cohort of patients with breast cancer. Plast Reconstr Surg 144:303–313. https://doi.org/10.1097/PRS.0000000000005803
Takahashi M, Kai I, Hisata M, Higashi Y (2006) The association between breast surgeons’ attitudes toward breast reconstruction and their reconstruction-related information-giving behaviors: a nationwide survey in Japan. Plast Reconstr Surg 118:1507–1514. https://doi.org/10.1097/01.prs.0000233149.36751.d2
Alderman AK, Hawley ST, Waljee J, Morrow M, Katz SJ (2007) Correlates of referral practices of general surgeons to plastic surgeons for mastectomy reconstruction. Cancer 109:1715–1720. https://doi.org/10.1002/cncr.22598
Lee CNH, Ubel PA, Deal AM, Blizard LB, Sepucha KR, Ollila DW, Pignone MP (2016) How informed is the decision about breast reconstruction after mastectomy? A prospective, cross-sectional study. Ann Surg 264:1103–1109. https://doi.org/10.1097/SLA.0000000000001561
de Ligt KM, van Bommel ACM, Schreuder K, Maduro JH, Vrancken Peeters MTFD, Mureau MAM, Siesling S, NABON Breast Cancer Audit Working Group (2018) The effect of being informed on receiving immediate breast reconstruction in breast cancer patients. Eur J Surg Oncol 44:717–724. https://doi.org/10.1016/j.ejso.2018.01.226
Frisell A, Lagergren J, Halle M, Boniface J (2020) Influence of socioeconomic status on immediate breast reconstruction rate, patient information and involvement in surgical decision-making. BJS Open 4:232–240. https://doi.org/10.1002/bjs5.50260
Wong A, Snook K, Brennan M, Flitcroft K, Tucker M, Hiercz D, Spillane A (2014) Increasing breast reconstruction rates by offering more women a choice. ANZ J Surg 84:31–36. https://doi.org/10.1111/ans.12471
Acknowledgments
The authors thank Fernanda Mesa-Chavez, Paulina Blanco-Murillo, and Sarai de Monserrat Cervantes-Sifuentes for their kind contributions.
Author information
Authors and Affiliations
Contributions
Paulina Bajonero-Canonico: Conceptualization, methodology, investigation, and writing—review and editing. Ana S. Ferrigno: Formal analysis and writing—original draft. Jorge A. Saldaña-Rodríguez: Investigation. David E. Hinojosa Gonzalez: Investigation. Cristel G. de la O-Maldonado: Investigation. Carlos de la Cruz-de la Cruz: Data curation and formal analysis. Brizio Moreno-Jaime: Conceptualization. Mariela Hernandez-Pavon: Conceptualization. Jose Moral-de la Rubia: Conceptualization. Melina Miaja-Avila: Conceptualization, methodology, and supervision. Cynthia Villarreal-Garza: Conceptualization, methodology, project administration, supervision, and writing—review and editing.
Corresponding authors
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethics approval
This research protocol was approved by the Institutional Research Board of Escuela de Medicina del Instituto Tecnologico y de Estudios Superiores de Monterrey.
Consent to participate
Informed consent for participation in this study was obtained from each patient prior to inclusion.
Consent for publication
Informed consent was obtained from each patient for the use of their anonymized data for scientific purposes.
Code availability
Not applicable.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Bajonero-Canonico, P., Ferrigno, A.S., Saldaña-Rodriguez, J.A. et al. Factors associated with the desire to undergo post-mastectomy breast reconstruction in a Mexican breast cancer center. Support Care Cancer 29, 2679–2688 (2021). https://doi.org/10.1007/s00520-020-05784-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00520-020-05784-4