Abstract
Purpose
To identify modifiable and non-modifiable risk factors for peripheral intravenous catheter (PIV) failure among patients requiring intravenous treatment for oncology and haematology conditions.
Methods
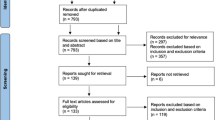
A single-centre prospective cohort study was conducted between October 2017 and February 2019. Adult in-patients requiring a PIV for therapy were prospectively recruited from two cancer units at a tertiary hospital in Queensland, Australia. The primary outcome was a composite of complications leading to PIV failure (local and bloodstream infection; occlusion; infiltration/extravasation; leakage; dislodgement; and/or phlebitis). Secondary outcomes were (i) PIV dwell time; (ii) insertion and (iii) failure of a CVAD; (iv) adverse events; (v) length of hospital stay. Outcomes were investigated using Bayesian multivariable linear regression modelling and survival analysis.
Results
Of 200 participants, 396 PIVs were included. PIV failure incidence was 34.9%; the most common failure type was occlusion/infiltration (n = 74, 18.7%), then dislodgement (n = 33, 8.3%), and phlebitis (n = 30, 7.6%). While several patient and treatment risk factors were significant in univariable modelling, in the final multivariable model, only the use of non-sterile tape (external to the primary dressing) was significantly associated with decreased PIV dislodgement (hazard ratio 0.06, 95% confidence interval 0.01, 0.48; p = 0.008).
Conclusion
PIV failure rates among patients receiving cancer treatment are high, the sequelae of which may include delayed treatment and infection. Larger studies on risk factors and interventions to prevent PIV failure in this population are needed; however, the use of secondary securements (such as non-sterile tape) to provide further securement to the primary PIV dressing is particularly important.
Trial registration
Study methods were registered prospectively with the Australian New Zealand Clinical Trials Registry on the 27th March 2017 (ACTRN12617000438358); https://www.anzctr.org.au/Trial/Registration/TrialReview.aspx?id=372191&isReview=true


Similar content being viewed by others
References
Bertoglio S, van Boxtel T, Goossens GA, Dougherty L, Furtwangler R, Lennan E, Pittiruti M, Sjovall K, Stas M (2017) Improving outcomes of short peripheral vascular access in oncology and chemotherapy administration. J Vasc Access 18(2):89–96. https://doi.org/10.5301/jva.5000668
Gallieni M, Pittiruti M, Biffi R (2008) Vascular access in oncology patients. CA Cancer J Clin 58(6):323–346. https://doi.org/10.3322/CA.2008.0015
Chernecky C (2001) Satisfaction versus dissatisfaction with venous access devices in outpatient oncology: a pilot study. Oncol Nurs Forum 28(10):1613–1616
Freytes CO (1997) Vascular access problems revisited: the Multinational Association of Supportive Care in Cancer (MASCC) experience. Support Care Cancer 6(1):13–19. https://doi.org/10.1007/s005200050126
Daneman N, Downing M, Zagorski BM (2012) How long should peripherally inserted central catheterization be delayed in the context of recently documented bloodstream infection? J Vasc Interv Radiol 23(1):123–125. https://doi.org/10.1016/j.jvir.2011.09.024
Leal A, Kadakia K, Looker S, Hilger C, Sorgatz K, Anderson K, Jacobson A, Grendahl D, Seisler D, Hobday T (2014) Fosaprepitant-induced phlebitis: a focus on patients receiving doxorubicin/cyclophosphamide therapy. Support Care Cancer 22(5):1313–1317. https://doi.org/10.1007/s00520-013-2089-8
Webster J, Clarke S, Paterson D, Hutton A, Sv D, Gale C, Hopkins T (2008) Routine care of peripheral intravenous catheters versus clinically indicated replacement: randomised controlled trial. Br Med J 337(7662):157–160. https://doi.org/10.1136/bmj.a339
Bausone-Gazda D, Lefaiver CA, Walters S (2010) A randomized controlled trial to compare the complications of 2 peripheral intravenous catheter-stabilization systems. J Infus Nurs 33(6):371–384. https://doi.org/10.1097/NAN.0b013e3181f85be2
Schulmeister L (2011) Extravasation Management: Clinical Update. Semin Oncol Nurs 27(1):82–90. https://doi.org/10.1016/j.soncn.2010.11.010
Ener RA, Meglathery SB, Styler M (2004) Extravasation of systemic hemato-oncological therapies. Ann Oncol 15(6):858–862. https://doi.org/10.1093/annonc/mdh214
Wells S (2008) Venous access in oncology and haematology patients: part one. Nurs Stand 22(52):39–46. https://doi.org/10.7748/ns2008.09.22.52.39.c6649
Centers for Disease Control and Prevention National Healthcare Safety Network. (2019) Bloodstream Infection Event (Central Line-Associated Bloodstream Infection and Non-central Line Associated Bloodstream Infection) Chapter 17:1-30.
Helm RE, Klausner JD, Klemperer JD, Flint LM, Huang E (2019) Accepted but unacceptable: peripheral IV catheter failure. J Infus Nurs 42(3):151–164. https://doi.org/10.1097/NAN.0000000000000326
Doellman D, Hadaway L, Bowe-Geddes LA, Franklin M, LeDonne J, Papke-O'Donnell L, Pettit J, Schulmeister L, Stranz M (2009) Infiltration and extravasation: update on prevention and management. J Infus Nurs 32(4):203–211. https://doi.org/10.1097/NAN.0b013e3181aac042
Rickard CM, Marsh N, Webster J, Runnegar N, Larsen E, McGrail MR, Fullerton F, Bettington E, Whitty JA, Choudhury MA (2018) Dressings and securements for the prevention of peripheral intravenous catheter failure in adults (SAVE): a pragmatic, randomised controlled, superiority trial. Lancet 392(10145):419–430. https://doi.org/10.1016/S0140-6736(18)31380-1
Harris PA, Taylor R, Thielke R, Payne J, Gonzalez N, Conde JG (2009) Research electronic data capture (REDCap)—a metadata-driven methodology and workflow process for providing translational research informatics support. J Biomed Inform 42(2):377–381. https://doi.org/10.1016/j.jbi.2008.08.010
Ullman AJ, Mihala G, O’Leary K, Marsh N, Woods C, Bugden S, Scott M, Rickard CM (2019) Skin complications associated with vascular access devices: a secondary analysis of 13 studies involving 10,859 devices. Int J Nurs Stud 91:6–13. https://doi.org/10.1016/j.ijnurstu.2018.10.006
Mallett S, Royston P, Dutton S, Waters R, Altman DG (2010) Reporting methods in studies developing prognostic models in cancer: a review. BMC Med 8(1):20. https://doi.org/10.1186/1741-7015-8-20
Marsh N, Webster J, Larson E, Cooke M, Mihala G, Rickard CM (2018) Observational study of peripheral intravenous catheter outcomes in adult hospitalized patients: a multivariable analysis of peripheral intravenous catheter failure. J Hosp Med 13(2):83–89. https://doi.org/10.12788/jhm.2867
StataCorp (2017) Stata Statistical Software: Release 15. StataCorp LLC, College Station
von Elm E, Altman DG, Egger M, Pocock SJ, Gotzsche PC, Vandenbroucke JP (2007) The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement: guidelines for reporting observational studies. Lancet 370(9596):1453–1457. https://doi.org/10.1016/s0140-6736(07)61602-x
Martínez J, Piazuelo M, Almela M, Blecua P, Gallardo R, Rodríguez S, Escalante Z, Robau M, Trilla A (2009) Evaluation of add-on devices for the prevention of phlebitis and other complications associated with the use of peripheral catheters in hospitalised adults: a randomised controlled study. J Hosp Infect 73(2):135–142. https://doi.org/10.1016/j.jhin.2009.06.031
Fidalgo JP, Fabregat LG, Cervantes A, Margulies A, Vidall C, Roila F (2012) Management of chemotherapy extravasation: ESMO–EONS clinical practice guidelines. Ann Oncol 23:vii167–vii173. https://doi.org/10.1093/annonc/mds294
Kassner E (2000) Evaluation and treatment of chemotherapy extravasation injuries. J Pediatr Oncol Nurs 17(3):135–148. https://doi.org/10.1053/jpon.2000.8063
Russell E, Chan RJ, Marsh N, New K (2013) A point prevalence study of cancer nursing practices for managing intravascular devices in an Australian tertiary cancer center. Eur J Oncol Nurs 18(3):231–235. https://doi.org/10.1016/j.ejon.2013.11.010
Wallis MC, McGrail M, Webster J, Marsh N, Gowardman J, Playford EG, Rickard CM (2014) Risk factors for peripheral intravenous catheter failure: a multivariate analysis of data from a randomized controlled trial. Infect Control Hosp Epidemiol 35(1):63–68. https://doi.org/10.1086/674398
Salgueiro-Oliveira A, Parreira P, Veiga P (2012) Incidence of phlebitis in patients with peripheral intravenous catheters: the influence of some risk factors. Aust J Adv Nurs 30(2):32–39
Nassaji-Zavareh M, Ghorbani R (2007) Peripheral intravenous catheter-related phlebitis and related risk factors. Singap Med J:733–736
Furtado LCR (2011) Incidence and predisposing factors of phlebitis in a surgery department. Br J Nurs 20(Sup7):S16–S25. https://doi.org/10.12968/bjon.2011.20.Sup7.S16
Miliani K, Taravella R, Thillard D, Chauvin V, Martin E, Edouard S, Astagneau P (2017) Peripheral venous catheter-related adverse events: evaluation from a multicentre epidemiological study in France (the CATHEVAL Project). PLoS One 12(1). https://doi.org/10.1371/journal.pone.0168637
Corley A, Ullman AJ, Marsh N, Larsen EN, Mihala G, Harris PNA, Rickard CM (2019) SECURE -ment bundles to prevent peripheral vascular access device failure – The SECURE -PVAD trial: Study protocol for a pilot randomized control trial. Vasc Access 13(3):6–14
Pagnutti L, Bin A, Donato R, Di Lena G, Fabbro C, Fornasiero L, Gerratana A, Rigon L, Gonella S, Palese A (2015) Difficult intravenous access tool in patients receiving peripheral chemotherapy: a pilot-validation study. Eur J Oncol Nurs 20:58–63. https://doi.org/10.1016/j.ejon.2015.06.008
Van Loon F, Buise M, Claassen J, Dierick-van Daele A, Bouwman AJ, Bjoa (2018) Comparison of ultrasound guidance with palpation and direct visualisation for peripheral vein cannulation in adult patients: a systematic review and meta-analysis. Br J Anaesth 121(2):358–366. https://doi.org/10.1016/j.bja.2018.04.047
Chopra V, Flanders SA, Saint S, Woller SC, O'Grady NP, Safdar N, Trerotola SO, Saran R, Moureau N, Wiseman S (2015) The Michigan Appropriateness Guide for Intravenous Catheters (MAGIC): results from a multispecialty panel using the RAND/UCLA appropriateness method. Ann Intern Med 163(Sup6):S1–S40. https://doi.org/10.7326/M15-0744
Chopra V, Anand S, Krein SL, Chenoweth C, Saint S (2012) Bloodstream infection, venous thrombosis, and peripherally inserted central catheters: reappraising the evidence. Am J Med 125(8):733–741. https://doi.org/10.1016/j.amjmed.2012.04.010
Infusion Nurses Society (2016) Infusion Therapy Standards of Practice, pp S1–S159
Freifeld A, Marchigiani D, Walsh T, Chanock S, Lewis L, Hiemenz J, Hiemenz S, Hicks JE, Gill V, Steinberg SM (1999) A double-blind comparison of empirical oral and intravenous antibiotic therapy for low-risk febrile patients with neutropenia during cancer chemotherapy. N Engl J Med 341(5):305–311. https://doi.org/10.1056/NEJM199907293410501
Armenteros-Yeguas V, Gárate-Echenique L, Tomás-López MA, Cristóbal-Domínguez E, Moreno-de Gusmão B, Miranda-Serrano E, Moraza-Dulanto MI (2017) Prevalence of difficult venous access and associated risk factors in highly complex hospitalised patients. J Clin Nurs 26(23-24):4267–4275. https://doi.org/10.1111/jocn.13750
Larsen E, Keogh S, Marsh N, Rickard C (2017) Experiences of peripheral IV insertion in hospital: a qualitative study. Br J Nurs 26(19):S18–S25. https://doi.org/10.12968/bjon.2017.26.19.S18
Fink RM, Ellen Hjort RNN, Barbara Wenger R, Mary Cunningham R, Aimee Orf R, Wendy Pare R, Jennifer Zwink R (2009) The impact of dry versus moist heat on peripheral IV catheter insertion in a hematology-oncology outpatient population. Oncol Nurs Forum 36(4):E198–E204. https://doi.org/10.1188/09.ONF.E198-E204
Byers T, Wender RC, Jemal A, Baskies AM, Ward EE, Brawley OW (2016) The American Cancer Society challenge goal to reduce US cancer mortality by 50% between 1990 and 2015: results and reflections. CA Cancer J Clin 66(5):359–369. https://doi.org/10.3322/caac.21348
Miller KD, Siegel RL, Lin CC, Mariotto AB, Kramer JL, Rowland JH, Stein KD, Alteri R, Jemal A (2016) Cancer treatment and survivorship statistics, 2016. CA Cancer J Clin 66(4):271–289. https://doi.org/10.3322/caac.21349
Richards M, Corner J, Maher J (2011) The National Cancer Survivorship Initiative: new and emerging evidence on the ongoing needs of cancer survivors. Br J Cancer 105(1):S1–S4. https://doi.org/10.1038/bjc.2011.416
Hallam C, Weston V, Denton A, Hill S, Bodenham A, Dunn H, Jackson T (2016) Development of the UK Vessel Health and Preservation (VHP) framework: a multi-organisational collaborative. J Infect Prev 17(2):65–72. https://doi.org/10.1177/1757177415624752
Camp-Sorrell D, Matey L (2017) Access device standards of practice for oncology nursing. Oncology Nursing Society.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Human Research Ethics Committee (HREC) approval was obtained from the Royal Brisbane and Women’s Hospital (HREC/17/RBWH/7) and Griffith University (NRS/2017/154).
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Larsen, E.N., Marsh, N., O’Brien, C. et al. Inherent and modifiable risk factors for peripheral venous catheter failure during cancer treatment: a prospective cohort study. Support Care Cancer 29, 1487–1496 (2021). https://doi.org/10.1007/s00520-020-05643-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00520-020-05643-2