Abstract
Background
Oral mucositis (OM) is an oral toxicity caused by cancer treatment, found often in patients with head and neck cancer. Low-intensity laser therapy for OM has anti-inflammatory, analgesic, and tissue reparative properties.
Objective
The objective of this work is to perform a systematic review and meta-analysis of the randomized clinical trials of OM laser therapy in patients undergoing treatment for head and neck cancers, followed by a cost-effectiveness analysis of the therapy.
Method
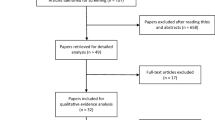
The search terms, mucositis and phototherapy, laser therapy and mucositis, photobiomodulation and mucositis, and low-level laser therapy and mucositis, were used to search the databases of PubMed, Web of Science, and MEDLINE. Randomized clinical trials were divided into two groups: one treated with laser therapy and the other given a placebo. Only 13 studies were included in the systematic review, and 6 studies in the meta-analysis.
Results
The results of the systematic review and meta-analysis show that the laser therapy presented good results in clinical improvement and pain reduction, decreasing the patients’ likelihood of developing OM, with degrees of debilitating lesions, to 64% (RR = 0.36 [95% CI = 0.29–0.44]). The cost-effectiveness analysis revealed an incremental cost of R$ 3687.53 for the laser group, with an incremental effectiveness of 132.2. The incremental cost-effectiveness ratio (ICER) was 27.89, for the severe OM cases that were avoided.
Conclusion
It was concluded, therefore, that photobiomodulation for OM in patients receiving head and neck cancer treatment was clinically effective and cost-effective.



Similar content being viewed by others
References
Bensadoun RJ, Nair RG (2012) Low-level laser therapy in the prevention and treatment of cancer therapy-induced mucositis: state of the art based on literature review and meta-analysis. Curr Opin Oncol 24(4):363–370. https://doi.org/10.1097/cco.0b013e328352eaa3
Mañas A, Cerezo L, de la Torre A et al (2012) Epidemiology and prevalence of oropharyngeal candidiasis in Spanish patients with head and neck tumors undergoing radiotherapy treatment alone or in combination with chemotherapy. Clin Transl Oncol 14(10):740–746. https://doi.org/10.1007/s12094-012-0861-8
Gautam AP, Fernandes DJ, Vidyasagar MS, Maiya GA (2012) Low level helium neon laser therapy for chemoradiotherapy induced oral mucositis in oral câncer patients: a randomized controlled trial. Oral Oncol 48(9):893–897. https://doi.org/10.1016/j.oraloncology.2012.03.008
Cruz LB, Ribeiro AS, Rech A, Rosa LGN, Castro CG Jr, Brunetto AL (2007) A influence of low-energy laser in the prevention of oral mucositis in children with cancer receiving chemotherapy. Pediatr Blood Cancer 48:435–444. https://doi.org/10.1002/pbc.20943
Lima AG, Villar RC, Castro GJ et al (2012) Oral mucositis prevention by low-level laser therapy in head-and-neck cancer patients undergoing concurrent chemoradiotherapy: a phase III randomized study. Int J Radiat Oncol Biol Phys 82(1):270–275. https://doi.org/10.1016/j.ijrobp.2010.10.012
Jensen SB, Jarvis V, Zadik Y et al (2013) Systematic review of miscellaneous agents for the management of oral mucositis in cancer patients. Support Care Cancer 21(11):3223–3232. https://doi.org/10.1007/s00520-013-1884-6
Saunders DP, Epstein JB, Elad S et al (2013) Systematic review of antimicrobials, mucosal coating agents, anesthetics, and analgesics for the management of oral mucositis in cancer patients. Support Care Cancer 21(11):3191–3207. https://doi.org/10.1007/s00520-014-2542-3
Graham ID, Logan J, Harrison MB, Straus SE, Tetroe J, Caswell W, Robinson N (2006) Lost in knowledge translation: time for a map? J Contin Educ Heal Prof 26(1):13–24. https://doi.org/10.1002/chp.47
Hagiwara S, Iwasaka H, Okuda K, Noguchi T (2007) GaIAIs (830nm) low-level laser enhances peripheral endogenous opioid analgesia in rats. Lasers Surg Med 39(10):797–802. https://doi.org/10.1002/lsm.20583
Soárez PC (2014) Decision models for economic evaluations of health technologies. Rev Ciência Saúde Coletiva 19(10):4209–4222. https://doi.org/10.1590/1413-812320141910.02402013
Changik JO (2014) Cost-of-illness studies: concepts, scopes, and methods. Clin Mol Hepatol 20(4):327–337. https://doi.org/10.3350/cmh.2014.20.4.327
Elting LS, Cooksley CD, Chambers MS, Garden AS (2007) Risk, outcomes, and costs of radiation-induced oral mucositis among patients with head-and-neck malignancies. Int J Radiat Oncol BiolPhys 68(4):1110–1120. https://doi.org/10.1016/j.ijrobp.2007.01.053
World Health Organization (2003) Making choices in health: WHO guide to cost-effectiveness analysis. https://www.who.int/choice/book/en/. Accessed 10 June 2019
Husereau D, Drummond M, Petrou S, Carswell C, Moher D, Greenberg D, Augustovski F, Briggs AH, Mauskopf J, Loder E, ISPOR Health Economic Evaluation Publication Guidelines-CHEERS Good Reporting Practices Task Force (2013) Consolidated health economic evaluation reporting standards (CHEERS) explanation and elaboration: a report of the ISPOR health economic evaluations publication guidelines good reporting practices task force. Value Health 16(2):231–250. https://doi.org/10.1016/j.jval.2013.02.002
Drummond MF, Sculpher MJ, Claxton K et al (2015) Methods for the economic evaluation of health care Programmes. Oxford University Press
Brazil Ministry of Health (2012) Executive secretary. Economic Area of Health and Development
Moraz G, Garcez AS, Assis EM et al (2015) Health cost-effectiveness studies in Brazil: a systematic review. Ciênc Saúde Coletiva 20(10):3211–3229. https://doi.org/10.1590/1413-812320152010.00962015
Antunes HS, Schluckebier LF, Herchenhorn D, Small IA, Araújo CMM, Viégas CMP, Rampini MP, Ferreira EMS, Dias FL, Teich V, Teich N, Ferreira CG (2016) Cost-effectiveness of low-level laser therapy (LLLT) in head and neck cancer patients receiving concurrent chemoradiation. Oral Oncol 52:85–90. https://doi.org/10.1016/j.oraloncology.2015.10.022
Silva EM, Silva MT, Augustovski F et al (2017) Guidelines for reporting economic evaluation studies. Epidemiol Serv Saude 26(4):895–898. https://doi.org/10.5123/S1679-49742017000400020
Gautam AP, Fernandes DJ, Vidyasagar MS, Maiya AG, Nigudgi S (2013) Effect of low-level laser therapy on patient reported measures of oral mucositis and quality of life in head and neck cancer patients receiving chemoradiotherapy—a randomized controlled trial. Support Care Cancer 21:1421–1428. https://doi.org/10.1007/s00520-012-1684-4
Gautam AP, Fernandes DJ, Vidyasagar MS, Maiya AG, Vadhiraja BM (2012) Low level laser therapy for concurrent chemoradiotherapy induced oral mucositis in head and neck cancer patients- a triple blinded randomized controlled trial. Radiother Oncol 104:349–354. https://doi.org/10.1016/j.radonc.2012.06.011
Gautam AP, Fernandes DJ, Vidyasagar MS, Maiya AG, Guddattu V (2015) Low level laser therapy against radiation induced oral mucositis in elderly head and neck cancer patients- a randomized placebo-controlled trial. J Photochem Photobiol B Biol 144:51–56. https://doi.org/10.1016/j.jphotobiol.2015.01.011
Oton-Leite AF, Elias LSA, Morais OM et al (2013) Effect of low-level laser therapy in the reduction of oral complications in patients with cancer of the head and neck submitted to radiotherapy. Spec Care Dentist 33(6):294–300. https://doi.org/10.1111/j.1754-4505.2012.00303.x
Oton-Leite AF, Silva GBL, Morais OM et al (2015) Effect of low-level laser therapy on Chemoradiotherapy-induced Oral Mucositis and salivary inflammatory mediators in head and neck Cancer patients. Lasers Surg Med 47:296–305. https://doi.org/10.1002/lsm.22349
Antunes HS, Herchenhorn D, Small IA, Araújo CMM, Viégas CMP, Cabral E, Rampini MP, Rodrigues PC, Silva TGP, Ferreira EMS, Dias FL, Ferreira CG (2013) Phase III trial of low-level laser therapy to prevent oral mucositis in head and neck cancer patients treated with concurrent chemoradiation. Radiother Oncol 109(2):297–302. https://doi.org/10.1016/j.radonc.2013.08.010
Antunes HS, Herchenhorn D, Small IA, Araújo CMM, Viégas CMP, de Assis Ramos G, Dias FL, Ferreira CG (2017) Long-term survival of a randomized phase III trial of head and neck cancer patients receiving concurrent chemoradiation therapy with or without low-level laser therapy (LLLT) to prevent oral mucositis. Oral Oncol 71:11–15. https://doi.org/10.1016/j.oraloncology.2017.05.018
Arora H, Pai KM, Maiya A, Vidyasagar MS, Rajeev A (2008) Efficacy of he-ne laser in the prevention and treatment of radiotherapy-induced oral mucositis in oral cancer patients. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 105(2):180–186. https://doi.org/10.1016/j.tripleo.2007.07.043
Carvalho PA, Jaguar GC, Pellizzon AC et al (2011) Evaluation of low-level laser therapy in the prevention and treatment of radiation-induced mucositis: a double-blind randomized study in head and neck cancer patients. Oral Oncol 47(12):1176–1181. https://doi.org/10.1016/j.oraloncology.2011.08.021
Shaw MJ, Kumar NDK, Duggal M, Fiske J, Lewis DA, Kinsella T, Nisbet T (2000) Oral management of patients following oncology treatment: literature review. Br Assoc Oral Maxillofac Surg 38:519–524. https://doi.org/10.1054/bjom.2000.0468
Rosenthal DI, Trotti A (2009) Strategies for managing radiation. Induced Mucositis in Head and Neck Cancer. Semin Radiat Oncol 19:29–34. https://doi.org/10.1016/j.semradonc.2008.09.006
Singh N, Scully C, Joyston-bechal S (1996) Oral complications of Cancer therapies: prevention and management. Clin Oncol 8:15–24. https://doi.org/10.1016/S0936-6555(05)80034-2
Genot-Klastersky MT, Klastersky J, Awada F et al The use of low-energy laser (LEL) for the prevention of chemotherapy- and/or radiotherapy-induced oral mucositis in cancer patients: results from two prospective studies. Support Care Cancer 16(12):1381–1387. https://doi.org/10.1007/s00520-008-0439-8
Simões A, Eduardo FP, Luiz AC, Campos L, Sá PHRN, Cristófaro M, Marques MM, Eduardo CP (2009) Laser phototherapy as topical prophylaxis against head and neck cancer radiotherapy-induced oral mucositis: comparison between low and high/low power lasers. Lasers Surg Med 41(4):264–270. https://doi.org/10.1002/lsm.20758
Worthington HV, Clarkson JE, Eden OB (2006) Interventions for preventing oral mucositis for patients with cancer receiving treatment. Cochrane Database Syst Rev 2. https://doi.org/10.1002/14651858.CD000978.pub2
Silva GB, Sacono NT, Oton-Leite AF et al (2015) Effect of low-level laser therapy on inflammatory mediator release during chemotherapy-induced oral mucositis: a randomized preliminary study. Lasers Med Sci 30(1):117–126. https://doi.org/10.1007/s10103-014-1624-2
Silva GB, Mendonça EF, Bariani C et al (2014) The prevention of induced oral mucositis with low-level laser therapy in bone marrow transplantation patients: a randomized clinical trial. Photomed Laser Surg 29(1):27–31. https://doi.org/10.1089/pho.2009.2699
Figueiredo ALP, Lins L, Cattony AC, Falcão AFP (2013) Laser therapy in the control of oral mucositis: a meta-analysis. Ver Ass Med Bras 59:467–474. https://doi.org/10.1016/j.ramb.2013.08.003
Lima VHS, Oliveira-Neto OB, Sales PHH et al (2020) Effectiveness of low-level laser therapy for oral mucositis prevention in patients undergoing chemoradiotherapy for the treatment of head and neck cancer: a systematic review and meta-analysis. Oral Oncol 102:104524. https://doi.org/10.1016/j.oraloncology.2019.104524
Zadik Y, Arany PR, Fregnani ER et al (2019) Systematic review of photobiomodulation for the management of oral mucositis in cancer patients and clinical practice guidelines. Support Care Cancer 27(10):3969–3983. https://doi.org/10.1007/s00520-019-04890-2
Bjordal JM, Bensadoun RJ, Tunèr J, Frigo L, Gjerde K, Lopes-Martins RAB (2011) A systematic review with meta-analysis of the effect of low-level laser therapy (LLLT) in cancer therapy-induced oral mucositis. Support Care Cancer 19(8):1069–1077. https://doi.org/10.1007/s00520-011-1202-0
Peng H, Chen BB, Chen L, Chen YP, Liu X, Tang LL, Mao YP, Li WF, Zhang Y, Lin AH, Sun Y, Ma J (2017) A network meta-analysis in comparing prophylactic treatments of radiotherapy-induced oral mucositis for patients with head and neck cancers receiving radiotherapy. Oral Oncol 75:89–94. https://doi.org/10.1016/j.oraloncology.2017.11.001
Bezinelli LM, Eduardo FP, Lopes RMG et al (2014) Cost-effectiveness of the introduction of specialized oral care with laser therapy in hematopoietic stem cell transplantation. Hematol Oncol 32:31–39. https://doi.org/10.1002/hon.2050
Zanin T, Zanin F, Carvalhosa AA, de Souza Castro PH, Pacheco MT, Zanin ICJ, Brugnera A Jr (2008) Use of 660-nm diode laser in the prevention and treatment of human oral mucositis induced by radiotherapy and chemotherapy. Photomed Laser Surg 28(2):233–237. https://doi.org/10.1089/pho.2008.2242
Hodgson BD, Margolis DM, Salzman DE, Eastwood D, Tarima S, Williams LD, Sande JE, Vaughan WP, Whelan HT (2012) Amelioration of oral mucositis pain by NASA near-infrared light-emitting diodes in bone marrow transplant patients. Support Care Cancer 20(7):1405–1415. https://doi.org/10.1007/s00520-011-1223-8
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest. The authors have full control of all primary data and allow the journal to review this data if requested.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Campos, T.M., do Prado Tavares Silva, C.A., Sobral, A.P.T. et al. Photobiomodulation in oral mucositis in patients with head and neck cancer: a systematic review and meta-analysis followed by a cost-effectiveness analysis. Support Care Cancer 28, 5649–5659 (2020). https://doi.org/10.1007/s00520-020-05613-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00520-020-05613-8