Abstract
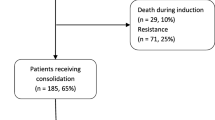
Invasive fungal infections (IFIs) are a major cause of morbidity and mortality in patients undergoing induction chemotherapy for acute myeloid leukemia (AML). In this patient population, antifungal prophylaxis (AP) has been associated with decreased incidence of IFIs and better survival. However, some centers have not adopted AP during induction chemotherapy for AML, as it is unclear whether AP improves outcomes in settings where the incidence of invasive mold infections is low. We retrospectively assessed the differences in clinical outcomes and resource utilization in patients undergoing 7 + 3 induction chemotherapy for AML, after implementing a policy of AP as part of a dedicated inpatient malignant hematology service (HS) at Rhode Island Hospital. Between January 1, 2007 and April 1, 2019, 56 patients with AML received AP during 7 + 3 induction chemotherapy and 52 patients did not, without significant differences in their baseline characteristics. Use of AP was associated with less proven or probable IFI (0% vs. 6%, P = 0.1) and lower all-cause in-hospital mortality (7% vs. 21%, P < 0.05), without significant increases in resource utilization or toxicities. Empiric and targeted antifungal therapies were more frequently started in the non-AP group (69%) than changed in the AP group (41%, P < 0.005). Having a dedicated inpatient malignant hematology service was also associated with improved outcomes. However, use of AP was associated with better survival (30-day post-induction survival log-rank P < 0.05), prior to the implementation of this clinical service as well, which is suggestive of an independent benefit from AP.

Similar content being viewed by others
References
Halpern AB, Lyman GH, Walsh TJ, Kontoyiannis DP, Walter RB (2015) Primary antifungal prophylaxis during curative-intent therapy for acute myeloid leukemia. Blood 126(26):2790–2797. https://doi.org/10.1182/blood-2015-07-627323
Cornely OA, Maertens J, Winston DJ, Perfect J, Ullmann AJ, Walsh TJ, Helfgott D, Holowiecki J, Stockelberg D, Goh YT, Petrini M, Hardalo C, Suresh R, Angulo-Gonzalez D (2007) Posaconazole vs. fluconazole or itraconazole prophylaxis in patients with neutropenia. N Engl J Med 356(4):348–359. https://doi.org/10.1056/NEJMoa061094
Lupianez CB, Canet LM, Carvalho A, Alcazar-Fuoli L, Springer J, Lackner M, Segura-Catena J, Comino A, Olmedo C, Rios R, Fernandez-Montoya A, Cuenca-Estrella M, Solano C, Lopez-Nevot MA, Cunha C, Oliveira-Coelho A, Villaescusa T, Fianchi L, Aguado JM, Pagano L, Lopez-Fernandez E, Potenza L, Luppi M, Lass-Florl C, Loeffler J, Einsele H, Vazquez L, Group PS, Jurado M, Sainz J (2015) Polymorphisms in host immunity-modulating genes and risk of invasive aspergillosis: results from the AspBIOmics consortium. Infect Immun 84(3):643–657. https://doi.org/10.1128/IAI.01359-15
Network NCC (2020) Prevention and Treatment of Cancer-Related Infections (Version 1.2020). http://www.nccn.org/professionals/physician_gls/pdf/infections.pdf. Accessed Feb 17 2020
Maertens JA, Girmenia C, Bruggemann RJ, Duarte RF, Kibbler CC, Ljungman P, Racil Z, Ribaud P, Slavin MA, Cornely OA, Peter Donnelly J, Cordonnier C, European Conference on Infections in Leukaemia ajvotEGfB, Marrow Transplantation tEOfR, Treatment of Cancer tIHSa, European Conference on Infections in Leukaemia ajvotEGfB, Marrow Transplantation tEOfR, Treatment of Cancer tIHS, the European L (2018) European guidelines for primary antifungal prophylaxis in adult haematology patients: summary of the updated recommendations from the European Conference on Infections in Leukaemia. J Antimicrob Chemother 73 (12):3221–3230. https://doi.org/10.1093/jac/dky286
De Pauw BE, Donnelly JP (2007) Prophylaxis and aspergillosis--has the principle been proven? N Engl J Med 356(4):409–411. https://doi.org/10.1056/NEJMe068266
Hammond SP, Marty FM, Bryar JM, DeAngelo DJ, Baden LR (2010) Invasive fungal disease in patients treated for newly diagnosed acute leukemia. Am J Hematol 85(9):695–699. https://doi.org/10.1002/ajh.21776
De Pauw B, Walsh TJ, Donnelly JP, Stevens DA, Edwards JE, Calandra T, Pappas PG, Maertens J, Lortholary O, Kauffman CA, Denning DW, Patterson TF, Maschmeyer G, Bille J, Dismukes WE, Herbrecht R, Hope WW, Kibbler CC, Kullberg BJ, Marr KA, Munoz P, Odds FC, Perfect JR, Restrepo A, Ruhnke M, Segal BH, Sobel JD, Sorrell TC, Viscoli C, Wingard JR, Zaoutis T, Bennett JE, European Organization for R, Treatment of Cancer/Invasive Fungal Infections Cooperative G, National Institute of A, Infectious Diseases Mycoses Study Group Consensus G (2008) Revised definitions of invasive fungal disease from the European Organization for Research and Treatment of Cancer/Invasive Fungal Infections Cooperative Group and the National Institute of Allergy and Infectious Diseases Mycoses Study Group (EORTC/MSG) Consensus Group. Clin Infect Dis 46(12):1813–1821. https://doi.org/10.1086/588660
Network NCC (2020) Acute myeloid leukemia (Version 3.2020). https://www.nccn.org/professionals/physician_gls/pdf/aml.pdf. Accessed Feb 17 2020
Foundation ABoIM (2012) Choosing wisely: EKGs and exercise stress tests. American Board of Internal Medicine Foundation, Washington, DC
Pagano L, Caira M, Candoni A, Aversa F, Castagnola C, Caramatti C, Cattaneo C, Delia M, De Paolis MR, Di Blasi R, Di Caprio L, Fanci R, Garzia M, Martino B, Melillo L, Mitra ME, Nadali G, Nosari A, Picardi M, Potenza L, Salutari P, Trecarichi EM, Tumbarello M, Verga L, Vianelli N, Busca A, Group S (2012) Evaluation of the practice of antifungal prophylaxis use in patients with newly diagnosed acute myeloid leukemia: results from the SEIFEM 2010-B registry. Clin Infect Dis 55(11):1515–1521. https://doi.org/10.1093/cid/cis773
Nomura K, Kawasugi K, Morimoto T (2006) Cost-effectiveness analysis of antifungal treatment for patients on chemotherapy. Eur J Cancer Care 15(1):44–50. https://doi.org/10.1111/j.1365-2354.2005.00618.x
Busca A, Lessi F, Verga L, Candoni A, Cattaneo C, Cesaro S, Dragonetti G, Delia M, De Luca A, Guglielmi G, Tumbarello M, Martino G, Nadali G, Fanci R, Picardi M, Potenza L, Nosari A, Aversa F, Pagano L, on the behalf of the SG (2017) SEIFEM 2010-E: economic evaluation of posaconazole for antifungal prophylaxis in patients with acute myeloid leukemia receiving induction chemotherapy. Leuk Lymphoma 58(12):2859–2864. https://doi.org/10.1080/10428194.2017.1318438
Lundberg J, Hoglund M, Bjorkholm M, Akerborg O (2014) Economic evaluation of posaconazole versus fluconazole or itraconazole in the prevention of invasive fungal infection in high-risk neutropenic patients in Sweden. Clin Drug Investig 34(7):483–489. https://doi.org/10.1007/s40261-014-0199-9
Cho SY, Lee DG, Choi JK, Lee HJ, Kim SH, Park SH, Choi SM, Choi JH, Yoo JH, Kim YJ, Kim HJ, Min WS, Back H, Kang S, Lee EK (2015) Cost-benefit analysis of posaconazole versus fluconazole or itraconazole as a primary antifungal prophylaxis in high-risk hematologic patients: a propensity score-matched analysis. Clin Ther 37(9):2019–2027. https://doi.org/10.1016/j.clinthera.2015.06.014
Camara R, Gozalbo I, Jurado M, Sanz J, Aragon B, Grau S (2017) Cost-effectiveness of posaconazole tablets for invasive fungal infections prevention in acute myelogenous leukemia or myelodysplastic syndrome patients in Spain. Adv Ther 34(9):2104–2119. https://doi.org/10.1007/s12325-017-0600-1
Hillner BE, Smith TJ, Desch CE (2000) Hospital and physician volume or specialization and outcomes in cancer treatment: importance in quality of cancer care. J Clin Oncol 18(11):2327–2340. https://doi.org/10.1200/JCO.2000.18.11.2327
Giri S, Pathak R, Aryal MR, Karmacharya P, Bhatt VR, Martin MG (2015) Impact of hospital volume on outcomes of patients undergoing chemotherapy for acute myeloid leukemia: a matched cohort study. Blood 125(21):3359–3360. https://doi.org/10.1182/blood-2015-01-625764
Zeidan AMPN, Wang X et al (2019) Patterns of care and clinical outcomes with 7+3 induction chemotherapy for patients (pts) with acute myeloid leukemia (AML) in the United States (US): a large population-based study. Blood 134(116)
Author information
Authors and Affiliations
Contributions
AH, RM, KV, JLR, and DF all helped write and revise the manuscript. AH and RM verified and extracted the data. AH, JLR, and DF analyzed the data. AH and DF created tables and figures.
Corresponding author
Ethics declarations
Conflict of interest
Farmakiotis: Astellas: Research Funding; Viracor-Eurofins: Consultancy, Research Funding.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Hsu, A., Matera, R., Vieira, K. et al. Antifungal prophylaxis during 7 + 3 induction chemotherapy for acute myeloid leukemia is associated with improved survival, in a setting with low incidence of invasive mold infections. Support Care Cancer 29, 707–712 (2021). https://doi.org/10.1007/s00520-020-05535-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00520-020-05535-5