Abstract
Purpose
To evaluate the impact of disclosure/nondisclosure of cancer diagnosis on patients’ posttraumatic stress symptoms (PTSS), posttraumatic growth (PTG), and quality of life (QOL).
Methods
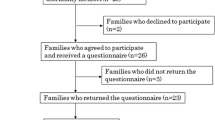
Patients with primary hepatocellular carcinoma (HCC) who were admitted for potentially curative treatments in a teaching hospital were recruited. Patients were interviewed at admission regarding their QOL and their attitude towards disclosure of diagnosis. They were interviewed again for QOL, PTSS, and PTG at discharge and at 1 month after discharge.
Results
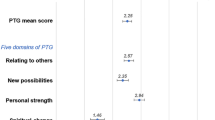
There were 300 patients recruited, 88.3% of whom preferred disclosure of cancer diagnosis. In fact, 162 patients (54.0%) received disclosure of their cancer diagnosis before discharge (disclosed group). However, for the 138 patients whose diagnoses were concealed by their families (uninformed group), 116 patients (84.1%) had learned of their diagnosis of HCC independently within 1 month after discharge. Comparing the scores at 1 month after discharge with scores at discharge showed that the PTSS score significantly declined for patients in the disclosed group and the PTG score significantly decreased for the uninformed patients at 1 month after discharge (p < 0.001 for both comparisons). Additionally, compared with the uninformed group, patients in the disclosed group had lower scores for PTSS (p < 0.001), higher scores for PTG (p < 0.001), better emotional functioning (p < 0.001), and better global QOL (p = 0.006) at 1 month after discharge.
Conclusions
Our findings indicate that concealing the diagnosis of cancer from patients is unlikely to succeed. Additionally, disclosure of diagnosis is beneficial for HCC patients in reducing PTSS and improving PTG and QOL.
Similar content being viewed by others
References
Waly Raphael S, Yangde Z, Yuxiang C (2012) Hepatocellular carcinoma: focus on different aspects of management. ISRN Oncol 2012:421673
Wang DC, Guo CB, Peng X et al (2011) Is therapeutic non-disclosure still possible? A study on the awareness of cancer diagnosis in China. Support Care Cancer 19(8):1191–1195
Jie B, Qiu Y, Feng ZZ et al (2016) Impact of disclosure of diagnosis and patient autonomy on quality of life and illness perceptions in Chinese patients with liver cancer. Psycho-Oncology 25(8):927–932
Fan X, Huang H, Luo Q et al (2011) Quality of life in Chinese home-based advanced cancer patients: does awareness of cancer diagnosis matter? J Palliat Med 14(10):1104–1108
Liu Y, Yang J, Huo D et al (2018) Disclosure of cancer diagnosis in china: the incidence, patient’s situation, and different preferences between patients and their family members and related influence factors. Cancer Manag Res 10:2173–2181
Li J, Yuan XL, Gao XH et al (2012) Whether, when, and who to disclose bad news to patients with cancer: a survey in 150 pairs of hospitalized patients with cancer and family members in China. Psycho-Oncology 21(7):778–784
Jiang Y, Liu C, Li JY et al (2007) Different attitudes of Chinese patients and their families toward truth telling of different stages of cancer. Psycho-oncology 16(10):928–936
Adellund HK, Jensen PT, Gilså HD (2016) Rehabilitation of women with gynecological cancer: the association between adult attachment, post-traumatic stress disorder and depression. Psycho-oncology 25(6):691–698
Abbey G, Thompson SB, Hickish TA (2015) A meta-analysis of prevalence rates and moderating factors for cancer-related post-traumatic stress disorder. Psycho-oncology 24(4):371–381
Li YX, Zhang GQ (2013) The symptomatic characteristics of posttraumatic stress disorder of cancer patients and social psychology related factors. China J Health Psychol 21(4):515–517
Parikh D, De Ieso P, Garvey G et al (2015) Post-traumatic stress disorder and post-traumatic growth in breast cancer patients—a systematic review. Asian Pac J Cancer Prev 16(2):641–646
Su LP, Shi TY, Lu J et al (2014) Psychological experiences of post-traumatic growth in patients with primary liver cancer. Chin Nurs Res 28(10B):3632–3634
Montazeri A, Hole DJ, Milroy R et al (2004) Does knowledge of cancer diagnosis affect quality of life? A methodological challenge. BMC Cancer 19(4):21
Bozcuk H, Erdogan V, Eken C et al (2002) Does awareness of diagnosis make any difference to quality of life? Determinants of emotional functioning in a group of cancer patients in Turkey. Support Care Cancer 10(1):51–57
Justo Roll I, Simms V, Harding R (2009) Multidimensional problems among advanced cancer patients in Cuba: awareness of diagnosis is associated with better patient status. J Pain Symptom Manag 37(3):325–330
MontazeriA TA, Mohagheghi MA et al (2009) Disclosure of cancer diagnosis and quality of life in cancer patients: should it be the same everywhere? BMC Cancer 9:39. https://doi.org/10.1186/1471-2407-9-39
Aggarwal AN, Singh N, Gupta D (2016) Does awareness of diagnosis influence health related quality of life in north Indian patients with lung cancer? Indian J Med Res 143(Supplement):S38–S44
Weathers FW, Litz BT, Huska JA et al (1994) PCL-C for DSM-IV. National Center for PTSD—Behavioral Science Division, Boston
Wang XM, Liu J, Wang Q et al (2013) PTSD Checklist-civilian (PCL-C) Chinese reversion in cancer patients. Med Inf 26(3):62–63
Tedeschi RG, Calhoun LG (1996) The posttraumatic growth inventory: measuring the positive legacy of trauma. J Trauma Stress 9(3):455–471
Dong L, Hu Y, Xu G et al (2013) Reliability and validity of the Chinese version of post-traumatic growth inventory scale in breast cancer survivors. J Nurs Sci 28(22):21–23
Fan SY, Eiser C, Ho MC et al (2013) Health-related quality of life in patients with hepatocellular carcinoma: the mediation effects of illness perceptions and coping. Psycho-Oncology 22(6):1353–1360
Wan C, Meng Q, Yang Z et al (2008) Validation of the simplified Chinese version of EORTC QLQ-C30 from the measurement of five types of inpatients with cancer. Ann Oncol 19(12):2053–2060
Bou Khalil R (2013) Attitudes, beliefs and perceptions regarding truth disclosure of cancer-related information in the Middle East: a review. Palliat Support Care 11(1):69–78
Zhang S, Yang Y, Yan D et al (2018) Internet videos and colorectal cancer in mainland China: a content analysis. BMC Med Inform Decis Mak 18(1):129. https://doi.org/10.1186/s12911-018-0711-x
China Internet Network Information Center Basic Data (2017) https://cnnic.com.cn/IDR/ReportDownloads/201706/P020170608523740585924.pdf Accessed on 18 June 2017
Richardson AE, Morton RP, Broadbent E (2016) Coping strategies predict post-traumatic stress in patients with head and neck cancer. Eur Arch Otorhinolaryngol 273:3385–3391
Mehnert A, Lehmann C, Graefen M et al (2010) Depression, anxiety, post-traumatic stress disorder and health-related quality of life and its association with social support in ambulatory prostate cancer patients. J Cancer Care (Engl) 19(6):736–745
Koutrouli N, Anagnostopoulos F, Potamianos G (2012) Posttraumatic stress disorder and posttraumatic growth in breast cancer patients: a systematic review. Women Health 52:503–516
Danhauer SC, Case LD, Tedeschi R et al (2013) Predictors of posttraumatic growth in women with breast cancer. Psycho-Oncology 22:2676–2683
Shand LK, Cowlishaw S, Brooker JE et al (2015) Correlates of post-traumatic stress symptoms and growth in cancer patients: a systematic review and meta-analysis. Psycho-oncology 24(6):624–634
Figueiredo MI, Fries E, Ingram KM (2004) The role of disclosure patterns and unsupportive social interactions in the well-being of breast cancer patients. Psycho-oncology 13:96–105
Goldsmith DJ, Miller LE, Caughlin JP (2009) Openness and avoidance in couples communication about cancer. In: Beck CS (ed) Communication Year book, vol 31. New York, Routledge, pp 62–117
Zhou Q, Shen JC, Liu YZ et al (2014) Effects of doctor-patient communication on quality of life among breast cancer patients in southern China. Asian Pac J Cancer Prev 15(14):5639–5644
Acknowledgments
The authors sincerely appreciate the patients for their participation and cooperation.
Funding
This study is supported by the grant from the National Social Science Fund of China (No. 16BSH096).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
This study was approved by the Ethics Committee of the Third Military Medical University (approval no. S-16096).
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
ESM 1
(DOCX 16 kb)
Appendix 1 The routine procedure of disclosure of cancer diagnosis in Chinese hospitals and the procedure of consent in this study
Appendix 1 The routine procedure of disclosure of cancer diagnosis in Chinese hospitals and the procedure of consent in this study
In Chinese hospitals, the patient’s family members act as legitimate agents to receive information and make decisions for patients. In addition, according to the China’s Law on Medical Practitioners, medical professionals are obligated to try to avoid adverse effects on patients when informing them about the disease, and the Law allows physicians to circumvent direct patient disclosure by telling the truth to the patient’s family.
When it is related to disclosure/nondisclosure of cancer diagnosis, Chinese healthcare professionals and researchers have a consensus, which is, asking the patient’s family’s opinion first. In detail, when the physicians have made the definitive diagnosis of cancer, the patients would be informed of the cancer diagnosis if they state that they would like to know and their family members agree to tell the truth. However, if the patient’s family members insist on concealing the cancer diagnosis from the patient, he/she would be informed of the diagnosis of benign disease, such as hepatic hemangioma or benign liver tumor in this study, which is a lie about diagnosis.
Regarding the consent for study, we talked to patients’ family members about our research and made it clear that we would respect their family decisions and take no intervention on them or on the patients. With the verbal consent of the patient’s family, we then talked to the patient. Considering for patients whose families made the decision of nondisclosure, we could not tell them that we were doing a research on cancer patients who were informed/uninformed of their diagnosis. Therefore, we told all of the possible participants that we were studying the quality of life (QOL) and psychological rehabilitation of patients undergoing liver surgery (They were really going to have liver surgery). We also told them that we would interview them and assess their QOL and psychological status by questionnaires. Then the patient signed a written informed consent form if he/she agreed to participate in our study.
Rights and permissions
About this article
Cite this article
Jie, B., Zhou, YH., Qiu, Y. et al. Impact of the disclosure of diagnosis on posttraumatic stress and growth and quality of life in Chinese patients with hepatocellular carcinoma. Support Care Cancer 28, 3371–3379 (2020). https://doi.org/10.1007/s00520-019-05141-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00520-019-05141-0