Abstract
Purpose
Despite having an excellent prognosis, patients with ductal carcinoma in situ (DCIS) report significant anxiety and depression following diagnosis. This study evaluated psychological morbidity using the Edmonton Symptom Assessment Scale (ESAS) in patients with DCIS compared with women with early-stage invasive breast cancer (EIBC) receiving radiotherapy (RT).
Methods
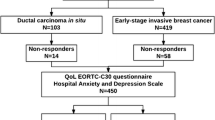
We identified patients diagnosed with DCIS or EIBC (stage I or II breast cancer) from 2011 to 2017 who had at least one ESAS completed pre- and post-RT. Data on systemic treatment, radiation, patient demographics, and disease stage were extracted from existing databases. Psychological morbidity was evaluated through measurement of depression, anxiety, and overall wellbeing within the ESAS. The Wilcoxon rank-sum test or chi-square test was performed for continuous or categorical variables.
Results
This study included 137 women with DCIS and 963 women with EIBC. ESAS was completed on average 28 days before RT (baseline) and 142 days after RT. Baseline ESAS scores showed significantly higher rates of depression among women with EIBC compared with those with DCIS (p = 0.006). Patients with EIBC also reported higher levels of anxiety and lower overall wellbeing than patients with DCIS, but this difference was not statistically significant. Post-RT ESAS scores showed significantly higher anxiety in patients with EIBC compared with DCIS (p = 0.049). Post-RT measures of anxiety and overall wellbeing were higher in patients with EIBC but differences were not statistically significant.
Conclusion
Women with DCIS experience relatively less psychological morbidity than women with EIBC, pre- and post-RT.
Similar content being viewed by others
References
Elshof L, Schaapveld M, Rutgers E, Schmidt M, de Munck L, van Leeuwen F, Wesseling J (2017) The method of detection of ductal carcinoma in situ has no therapeutic implications: results of a population-based cohort study. Breast Cancer Res 19(1):26
Duffy S, Dibden A, Michalopoulos D, Offman J, Parmar D, Jenkins J et al (2016) Screen detection of ductal carcinoma in situ and subsequent incidence of invasive interval breast cancers: a retrospective population-based study. Lancet Oncol 17(1):109–114
Siegel R, J MJ, Zou Z, Jemal A (2014) Cancer statistics, 2014. CA Cancer J Clin 64(1):9–29
Fallowfield L, Matthews L, Francis A, Jenkins V, Rea D (2014) Low grade ductal carcinoma in situ (DCIS): how best to describe it? Breast 23(5):693–696
Giannakeas V, Sopik V, Narod S (2018) Association of radiotherapy with survival in women treated for ductal carcinoma in situ with lumpectomy or mastectomy. JAMA Netw Open 1(4):e181100
Saadatmand S, Bretveld R, Siesling S, Tilanus-Linthorst M (2015) Influence of tumour stage at breast cancer detection on survival in modern times: population based study in 173 797 patients. BMJ 351:4901
National Comprehensive Cancer Network (2003) Distress management clinical practice guidelines in oncology. J Natl Compr Cancer Netw 1(3):344
Ozanne E, Schneider K, Soeteman D, Stout N, Schrag D, Fordis M, Punglia R (2015) onlineDeCISion.org: a web-based decision aid for DCIS treatment. Breast Cancer Res Treat 154(1):181–190. https://doi.org/10.1007/s10549-015-3605-y
Ruddy K, Meyer M, Giobbie-Hurder A, Emmons K, Weeks J, Winer E, Partridge A (2013) Long-term risk perceptions of women with ductal carcinoma in situ. Oncologist 18(4):362–368. https://doi.org/10.1634/theoncologist.2012-0376
van Gestel YRBM, Voogd AC, Vingerhoets AJJM, Mols F, Nieuwenhuijzen GAP, van Driel OJR, van Berlo CLH, van de Poll-Franse LV (2007) A comparison of quality of life, disease impact and risk perception in women with invasive breast cancer and ductal carcinoma in situ. Eur J Cancer 43(3):549–556
Lauzier S, Maunsell E, Levesque P, Mondor M, Robert J, Andre´ R et al (2010) Psychological distress and physical health in the year after diagnosis of DCIS or invasive breast cancer. Breast Cancer Res Treat 120(3):685–691
Liu Y, Pe’rez M, Schootman M, Aft RL, Gillanders WE, Jeffe DB (2011) Correlates of fear of cancer recurrence in women with ductal carcinoma in situ and early invasive breast cancer. Breast Cancer Res Treat 130(1):165–173
Jeffe DB, Perez M, Liu Y, Collins KK, Aft RL, Schootman M (2012) Quality of life over time in women diagnosed with ductal carcinoma in situ, early-stage invasive breast cancer, and agematched controls. Breast Cancer Res Treat 134(1):379–391
King MT, Winters ZE, Olivotto IA, Spillane AJ, Chua BH, Saunders C, Westenberg AH, Mann GB, Burnett P, Butow P, Rutherford C (2017) Patient reported outcomes in ductal carcinoma in situ: a systematic review. Eur J Cancer 71:95–108
Rakovitch E, Franssen E, Kim J, Ackerman I, Pignol JP, Paszat L, Pritchard KI, Ho C, Redelmeier DA (2003) A comparison of risk perception and psychological morbidity in women with ductal carcinoma in situ and early invasive breast cancer. Breast Cancer Res Treat 77(3):285–293
Gregorowitsch M, van den Bongard H, Young-Afat D, Pignol J, van Gils C, May A, Verkooijen H (2017) Severe depression more common in patients with ductal carcinoma in situ than early-stage invasive breast cancer patients. Breast Cancer Res Treat 167(1):205–213
Bruera E, Kuehn N, Miller MJ, Selmser P, Macmillan K (1991) The Edmonton Symptom Assessment System (ESAS): a simple method for the assessment of palliative care patients. J Palliat Care 7:6–9
Kim C, Liang L, Wright F, Hong N, Groot G, Helyer L et al (2017) Interventions are needed to support patient–provider decision-making for DCIS: a scoping review. Breast Cancer Res Treat 168(3):579–592
Stacey D, Légaré F, Lewis K et al (2017) Decision aids for people facing health treatment or screening decisions. Cochrane Database Syst Rev 4:1–297
Funding
This study received financial support of Bratty Family Fund, Michael and Karyn Goldstein Cancer Research Fund, Joey and Mary Furfari Cancer Research Fund, Pulenzas Cancer Research Fund, Joseph and Silvana Melara Cancer Research Fund, and Ofelia Cancer Research Fund.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
This study was approved by the Sunnybrook Health Sciences Centre research ethics board (REB #151-2017).
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
ESM 1
(DOCX 15 kb)
Rights and permissions
About this article
Cite this article
Pidduck, W., Wan, B.A., Zhang, L. et al. Psychological morbidity in women diagnosed with ductal carcinoma in situ compared with women with early breast cancer receiving radiotherapy. Support Care Cancer 28, 2247–2254 (2020). https://doi.org/10.1007/s00520-019-05034-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00520-019-05034-2