Abstract
Purpose
Cancer treatment may relate to appetite reduction and malnutrition. We investigated taste alterations and dish-type preferences during chemo- and/or radiation therapy in breast cancer patients.
Methods
Breast cancer patients (BC, n = 59) scheduled to receive cancer therapy and healthy subjects (control group or CTRL, n = 49) were voluntarily recruited. Taste detection thresholds (DTs) and recognition thresholds (RT) were compared between pre-treatment BC patients and CTRL for sweet (sucrose), salty (NaCl), bitter (caffeine), and sour (citric acid) solutions. Changes in taste thresholds and dish preferences during treatment were monitored in the BC group. Blood chemistry and anthropometric data were collected.
Results
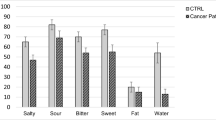
At baseline, BC patients demonstrated lower sweet and salty DTs and RTs and a higher sour RT compared to CTRL. Bitter DT and RT were similar in both groups. Mild/soft dishes were preferred over fried/oily dishes by BC patients. Throughout treatment in BC patients, sweet thresholds significantly declined, while salty, bitter, and sour DTs and RTs were not affected, and there was no increase in preference for a dish. However, preference towards mild/soft dishes remained. While sweet-sour fruits and sweetened nuts were not favored during therapy.
Conclusions
Sensitivities to sweet, salty, and sour but not bitter tastes differed between BC patients and CTRL. During treatment, sweet taste sensitivity increased while other tastes were unaffected. BC patients preferred mild/soft dishes over fried and sweetened dishes compared to CTRL. Our findings may contribute to developing dishes for breast cancer patients to increase food intake and thereby lower the risk of malnutrition.




Similar content being viewed by others
References
DeSantis CE, Bray F, Ferlay J, Lortet-Tieulent J, Anderson BO, Jemal A (2015) Cumulative logistic regression with food preference score as an ordinal variable was used to compare the preference of BC patients and CTRLs. The analyses were adjusted for age.1.International Variation in Female Breast Cancer Incidence and Mortality Rates Cancer Epidemiology, Biomarkers & Prevention 24 (10):1495–1506
Andre F, Mazouni C, Hortobagyi GN, Pusztai L (2006) DNA arrays as predictors of efficacy of adjuvant/neoadjuvant chemotherapy in breast cancer patients: current data and issues on study design. Biochim Biophys Acta (BBA)-Rev Cancer 1766(2):197–204
Group EEBCTC (2005) Effects of radiotherapy and of differences in the extent of surgery for early breast cancer on local recurrence and 15-year survival: an overview of the randomised trials. The Lancet. 366(9503):2087–2106
Steinbach S, Hummel T, Böhner C, Berktold S, Hundt W, Kriner M, Heinrich P, Sommer H, Hanusch C, Prechtl A (2009) Qualitative and quantitative assessment of taste and smell changes in patients undergoing chemotherapy for breast cancer or gynecologic malignancies. J Clin Oncol 27(11):1899–1905
Jensen SB, Mouridsen HT, Bergmann OJ, Reibel J, Brünner N, Nauntofte B (2008) Oral mucosal lesions, microbial changes, and taste disturbances induced by adjuvant chemotherapy in breast cancer patients. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 106(2):217–226
Bernhardson B-M, Tishelman C, Rutqvist LE (2008) Self-reported taste and smell changes during cancer chemotherapy. Support Care Cancer 16(3):275–283
Mattes RD, Arnold C, Boraas M (1987) Learned food aversions among cancer chemotherapy patients. Incidence, nature, and clinical implications. Cancer 60(10):2576–2580
Capra S, Ferguson M, Ried K (2001) Cancer: impact of nutrition intervention outcome—nutrition issues for patients. Nutrition 17(9):769–772
Epstein JB, Barasch A (2010) Taste disorders in cancer patients: pathogenesis, and approach to assessment and management. Oral Oncol 46(2):77–81
Gonella S (2013) Taste disorders in cancer patients. Assist Inferm Ric 32(4):223–232
Holmes S (1993) Food avoidance in patients undergoing cancer chemotherapy. Support Care Cancer 1(6):326–330
Huhmann MB, Cunningham RS (2005) Importance of nutritional screening in treatment of cancer-related weight loss. Lancet Oncol 6(5):334–343
Comeau TB, Epstein JB, Migas C (2001) Taste and smell dysfunction in patients receiving chemotherapy: a review of current knowledge. Support Care Cancer 9(8):575–580
Van Cutsem E, Arends J (2005) The causes and consequences of cancer-associated malnutrition. Eur J Oncol Nurs 9(Supplement 2):S51–S63
Speck RM, DeMichele A, Farrar JT, Hennessy S, Mao JJ, Stineman MG, Barg FK (2013) Taste alteration in breast cancer patients treated with taxane chemotherapy: experience, effect, and coping strategies. Support Care Cancer 21(2):549–555
Keast RSJ, Roper J (2007) A complex relationship among chemical concentration, detection threshold, and suprathreshold intensity of bitter compounds. Chem Senses 32(3):245–253
Sánchez-Lara K, Sosa-Sánchez R, Green-Renner D, Rodríguez C, Laviano A, Motola-Kuba D, Arrieta O (2010) Influence of taste disorders on dietary behaviors in cancer patients under chemotherapy. Nutr J 9:15
Hoehl K, Schoenberger GU, Busch-Stockfisch M (2010) Water quality and taste sensitivity for basic tastes and metallic sensation. Food Qual Prefer 21(2):243–249
Belqaid K, Orrevall Y, McGreevy J, Månsson-Brahme E, Wismer W, Tishelman C, Bernhardson B-M (2014) Self-reported taste and smell alterations in patients under investigation for lung cancer. Acta Oncol(Stockholm, Sweden) 53(10):1405–1412
Williams L, Cohen M (1978) Altered taste thresholds in lung cancer. Am J Clin Nutr 31(1):122–125
Settle R, Quinn M, Brand J, Kare M, Mullen J, Brown R (1979) Gustatory evaluation of cancer patients: preliminary results. Nutr Cancer:171–185
Ames H, Gee M, Hawrysh Z (1993) Taste perception and breast cancer: evidence of a role for diet. J Am Diet Assoc 93(5):541–546
Steinbach S, Hundt W, Zahnert T, Berktold S, Böhner C, Gottschalk N, Hamann M, Kriner M, Heinrich P, Schmalfeldt B (2010) Gustatory and olfactory function in breast cancer patients. Support Care Cancer 18(6):707–713
DeWys WD, Walters K (1975) Abnormalities of taste sensation in cancer patients. Cancer 36(5):1888–1896
Hayes JE, Bartoshuk LM, Kidd JR, Duffy VB (2008) Supertasting and PROP bitterness depends on more than the TAS2R38 gene. Chem Senses 33(3):255–265
Hayes JE, Wallace MR, Knopik VS, Herbstman DM, Bartoshuk LM, Duffy VB (2010) Allelic variation in TAS2R bitter receptor genes associates with variation in sensations from and ingestive behaviors toward common bitter beverages in adults. Chem Senses 36(3):311–319
Liang P, Jiang J, Ding Q, Tang X, Roy S (2018) Memory load influences taste sensitivities. Front Psychol 9:2533
Boltong A, Aranda S, Keast R, Wynne R, Francis PA, Chirgwin J, Gough K (2014) A prospective cohort study of the effects of adjuvant breast cancer chemotherapy on taste function, food liking, appetite and associated nutritional outcomes. PLoS One 9(7):e103512
Ovesen L, Sørensen M, Hannibal J, Allingstrup L (1991) Electrical taste detection thresholds and chemical smell detection thresholds in patients with cancer. Cancer 68(10):2260–2265
Hamed MS, Bondok AA (1977) Effect of vincristine on the histological structure of taste buds. Cells Tissues Organs 99(4):445–449
Kusaba T, Mori Y, Masami O, Hiroko N, Adachi T, Sugishita C, Sonomura K, Kimura T, Kishimoto N, Nakagawa H, Okigaki M, Hatta T, Matsubara H (2009) Sodium restriction improves the gustatory threshold for salty taste in patients with chronic kidney disease. Kidney Int 76(6):638–643
de Vries Y, van den Berg M, de Vries J, Boesveldt S, de Kruif JTC, Buist N, Haringhuizen A, Los M, Sommeijer D, Timmer-Bonte J (2017) Differences in dietary intake during chemotherapy in breast cancer patients compared to women without cancer. Support Care Cancer 25(8):2581–2591
Kim KO, Park H, Chun M, Lee EH, Kim H-S (2013) Eating patterns and use of nutritional information in breast cancer survivors treated with radiation therapy in South Korea (eating patterns and use of nutritional information in breast cancer survivors treated with radiation therapy in South Korea). J Nutr Health 46(3):250–260
Bessaoud F, Daures J-P, Gerber M (2008) Dietary factors and breast cancer risk: a case control study among a population in southern France. Nutr Cancer 60(2):177–187
Milliron B-J, Vitolins MZ, Tooze JA (2014) Usual dietary intake among female breast cancer survivors is not significantly different from women with no cancer history: results of the National Health and Nutrition Examination Survey, 2003-2006. J Acad Nutr Diet 114(6):932–937
de Vries Y, Winkels R, van den Berg M, de Graaf C, Kelfkens C, de Kruif JTC, Göker E, Grosfeld S, Sommeijer D, van Laarhoven H (2018) Altered food preferences and chemosensory perception during chemotherapy in breast cancer patients: a longitudinal comparison with healthy controls. Food Qual Prefer 63:135–143
Thomson CA, Flatt SW, Rock CL, Ritenbaugh C, Newman V, Pierce JP (2002) Increased fruit, vegetable and fiber intake and lower fat intake reported among women previously treated for invasive breast cancer. J Am Diet Assoc 102(6):801–808
Boltong A, Keast R (2012) The influence of chemotherapy on taste perception and food hedonics: a systematic review. Cancer Treat Rev 38(2):152–163
Acknowledgments
We thank Hyon Jung Park, Eun Ju Jeong, Woo Young Sim, Na Rae Yoon, Se Hyun Hu, and Hye Won Han for their assistance with subject enrollment and data collection.
Funding
This research was supported by the BK21 Plus project of the National Research Foundation of Korea Grant. The funder had no role in the study design, data collection and analysis, decision to publish, or preparation of the manuscript.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
The study protocol was approved by the Institutional Review Boards of Human Research Protection Center at Severance Hospital Yonsei University Health System (Board Approval Number 4-2012-0915), and each subject signed an informed consent prior to participating in the study.
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
ESM 1
(DOCX 399 kb)
Rights and permissions
About this article
Cite this article
Kim, Yh., Kim, G.M., Son, S. et al. Changes in taste and food preferences in breast cancer patients receiving chemotherapy: a pilot study. Support Care Cancer 28, 1265–1275 (2020). https://doi.org/10.1007/s00520-019-04924-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00520-019-04924-9