Abstract
Background
The effect of sarcopenia on digestive carcinoma surgery outcomes is controversial. We aimed to assess the effect of sarcopenia defined by the European Working Group on Sarcopenia in Older People (EWGSOP) or the Asian Working Group for Sarcopenia (AWGS) on outcomes following digestive carcinoma surgery.
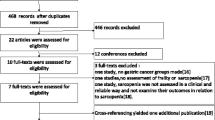
Methods
Eligible studies were searched from PubMed, EMBASE and other databases from inception to April 2018. We conducted a meta-analysis to estimate the risk ratios or mean differences of outcomes in the sarcopenia group versus the non-sarcopenia group. Stratified analyses and sensitivity analyses were performed.
Results
We included 11 cohort studies, with a sarcopenia prevalence ranging from 11.6 to 33.0%. Sarcopenia was associated with an increased risk of total complications (RR = 1.87, P < 0.00001), major complications (RR = 2.45, P = 0.002), re-admissions (RR = 2.53,P < 0.0001), infections (RR = 2.23, P = 0.09), severe infections (RR = 2.96, P = 0.04), 30-day mortality (RR = 3.36, P = 0.001), longer hospital stay (MD = 4.61, P = 0.001) and increased hospitalization expenditures (SMD = 0.25, P = 0.02). Sarcopenia differentially affected outcomes when stratified, and the results were stable.
Conclusions
Sarcopenia defined by the EWGSOP or AWGS Consensus was a high-risk factor for digestive carcinoma surgery outcomes. Different tumour site and muscle mass measurements are the sources of heterogeneity. More high-quality studies are needed.


Similar content being viewed by others
References
Bray F, Ferlay J, Soerjomataram I, Siegel RL, Torre LA, Jemal A (2018) Global cancer statistics 2018: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin 68(6):394–424. https://doi.org/10.3322/caac.21492
Thrumurthy SG, Chaudry MA, Hochhauser D, Mughal M (2013) The diagnosis and management of gastric cancer. BMJ (Clinical research ed) 347(nov04 1):f6367
Papenfuss WA, Kukar M, Oxenberg J, Attwood K, Nurkin S, Malhotra U, Wilkinson NW (2014) Morbidity and mortality associated with gastrectomy for gastric cancer. Ann Surg Oncol 21(9):3008–3014
Nations DEU (2013) World population prospects: the 2012 revision highlights and advance tables. New York United Nations Department of Economic & Social Affairs
Wagner D, Demarco MA, Amini N, Buttner S, Segev D, Gani F, Pawlik TM (2016) Role of frailty and sarcopenia in predicting outcomes among patients undergoing gastrointestinal surgery. World J Gastrointest Surg 8(1):27–40
Takeshita H, Ichikawa D, Kubota T, Okamoto K, Shiozaki A, Fujiwara H, Otsuji E (2013) Surgical outcomes of gastrectomy for elderly patients with gastric cancer. World J Surg 37(12):2891–2898
Rosenberg IH (1997) Sarcopenia: origins and clinical relevance. J Nutr 127(5 Suppl):990s–991s. https://doi.org/10.1093/jn/127.5.990S
Binay Safer V, Safer U, Kaplan M, Terekeci H, Top C (2015) Limitations of the definition of sarcopenia in cancer surgery. J Surg Oncol 112(1):116–116
Cruz-Jentoft AJ, Jean Pierre B, Bauer JM, Yves B, Tommy C, Francesco L, Martin FC, Jean-Pierre M, Yves R, Schneider SM (2010) Sarcopenia: European consensus on definition and diagnosis: report of the European Working Group on Sarcopenia in Older People. Age Ageing 39:412–423
Chen LK, Liu LK, Woo J, Assantachai P, Auyeung TW, Bahyah KS, Chou MY, Chen LY, Hsu PS, Krairit O, Lee JS, Lee WJ, Lee Y, Liang CK, Limpawattana P, Lin CS, Peng LN, Satake S, Suzuki T, Won CW, Wu CH, Wu SN, Zhang T, Zeng P, Akishita M, Arai H (2014) Sarcopenia in Asia: consensus report of the Asian Working Group for Sarcopenia. J Am Med Dir Assoc 15(2):95–101
Makiura D, Ono R, Inoue J, Kashiwa M, Oshikiri T, Nakamura T, Kakeji Y, Sakai Y, Miura Y (2016) Preoperative sarcopenia is a predictor of postoperative pulmonary complications in esophageal cancer following esophagectomy: a retrospective cohort study. Journal of Geriatric Oncology 7(6):430–436
Wang SL, Zhuang CL, Huang DD, Pang WY, Lou N, Chen FF, Zhou CJ, Shen X, Yu Z (2016) Sarcopenia adversely impacts postoperative clinical outcomes following gastrectomy in patients with gastric cancer: a prospective study. Ann Surg Oncol 23(2):556–564
Morley JE (2012) Sarcopenia in the elderly. Fam Pract 29(Suppl 1):i44–i48. https://doi.org/10.1093/fampra/cmr063
Walston JD (2012) Sarcopenia in older adults. Curr Opin Rheumatol 24(6):623–627
Haehling SV, Morley JE, Anker SD (2010) An overview of sarcopenia: facts and numbers on prevalence and clinical impact. J Cachexia Sarcopenia Muscle 1(2):129–133
Morley JE, Anker SD, Haehling SV (2014) Prevalence, incidence, and clinical impact of sarcopenia: facts, numbers, and epidemiology—update 2014. J Cachexia Sarcopenia Muscle 5(4):253–259
Muscaritoli M, Anker SJ, Aversa Z, Bauer JM, Biolo G, Boirie Y, Bosaeus I, Cederholm T, Costelli P, Fearon KC (2010) Consensus definition of sarcopenia, cachexia and pre-cachexia: joint document elaborated by Special Interest Groups (SIG) “cachexia-anorexia in chronic wasting diseases” and “nutrition in geriatrics”. Clin Nutr 29(2):154–159
Laviano A, Meguid MM, Inui A, Muscaritoli M, Rossi-Fanelli F (2005) Therapy insight: cancer anorexia-cachexia syndrome—when all you can eat is yourself. Nat Clin Pract Oncol 2(3):158–165
Scott D, Blizzard L, Fell J, Giles G, Jones G (2010) Associations between dietary nutrient intake and muscle mass and strength in community-dwelling older adults: the Tasmanian Older Adult Cohort Study. J Am Geriatr Soc 58(11):2129–2134
Valenzuela RER, Ponce JA, Morales-Figueroa GG, Muro KA, Carreón VR, Alemán-Mateo H (2013) Insufficient amounts and inadequate distribution of dietary protein intake in apparently healthy older adults in a developing country: implications for dietary strategies to prevent sarcopenia. Clin Interv Aging 8(2):1143–1148
Zhang G, Meng S, Li R, Ye J, Zhao L (2017) Clinical significance of sarcopenia in the treatment of patients with primary hepatic malignancies, a systematic review and meta-analysis. Oncotarget 8(60):102474–102485
Voron T, Tselikas L, Pietrasz D, Pigneur F, Laurent A, Compagnon P, Salloum C, Luciani A, Azoulay D (2015) Sarcopenia impacts on short- and long-term results of hepatectomy for hepatocellular carcinoma. Ann Surg 261(6):1173–1183
Peng P, Hyder O, Firoozmand A, Kneuertz P, Schulick RD, Huang D, Makary M, Hirose K, Edil B, Choti MA (2012) Impact of sarcopenia on outcomes following resection of pancreatic adenocarcinoma. J Gastrointest Surg 16(8):1478–1486
Lieffers JR, Bathe OF, Fassbender K, Winget M, Baracos VE (2012) Sarcopenia is associated with postoperative infection and delayed recovery from colorectal cancer resection surgery. Br J Cancer 107(6):931–936
Nakashima Y, Saeki H, Nakanishi R, Sugiyama M, Kurashige J, Oki E, Maehara Y (2017) Assessment of sarcopenia as a predictor of poor outcomes after esophagectomy in elderly patients with esophageal cancer. Ann Surg 267:1
Huang DD, Wang SL, Zhuang CL, Zheng BS, Lu JX, Chen FF, Zhou CJ, Shen X, Yu Z (2015) Sarcopenia, as defined by low muscle mass, strength and physical performance, predicts complications after surgery for colorectal cancer. Colorectal Dis Off J Assoc Coloproctol Great Britain Ireland 17(11):O256–O264
Jones K, Gordon-Weeks A, Coleman C, Silva M (2017) Radiologically determined sarcopenia predicts morbidity and mortality following abdominal surgery: a systematic review and meta-analysis. World J Surg 41(9):2266–2279
Simonsen C, De HP, Bjerre ED, Suetta C, Hojman P, Pedersen BK, Svendsen LB, Christensen JF (2018) Sarcopenia and postoperative complication risk in gastrointestinal surgical oncology: a meta-analysis. Ann Surg 268(1):1
Fukuda Y, Yamamoto K, Hirao M, Nishikawa K, Nagatsuma Y, Nakayama T, Tanikawa S, Maeda S, Uemura M, Miyake M (2015) Sarcopenia is associated with severe postoperative complications in elderly gastric cancer patients undergoing gastrectomy. Gastric Cancer : official journal of the International Gastric Cancer Association and the Japanese Gastric Cancer Association 34(3):S227–S227
Moher D, Liberati A, Tetzlaff J, Altman DG (2009) Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. BMJ (Clinical research ed)
Dindo D, Demartines N, Clavien P (2004) Classification of surgical complications: a new proposal with evaluation in a cohort of 6336 patients and results of a survey. Ann Surg 240(2):205–213
Chuling F, Hui H, Zuojun X (2016) The Newcastle-Ottawa Scale (NOS) for assessing the quality of nonrandomized studies
Doi SAR, Barendregt JJ, Khan S, Thalib L, Williams GM (2015) Advances in the meta-analysis of heterogeneous clinical trials I: the inverse variance heterogeneity model. Contemporary Clin Trials 45(Pt A):130–138
Shuster JJ (2011) Review: Cochrane handbook for systematic reviews for interventions, Version 5.1.0, published 3/2011. Julian P.T. Higgins and Sally Green, Editors. Res Synth Methods 2 (2):126–130
Harimoto N, Yoshizumi T, Izumi T, Motomura T, Harada N, Itoh S, Ikegami T, Uchiyama H, Soejima Y, Nishie A (2017) Clinical outcomes of living liver transplantation according to the presence of sarcopenia as defined by skeletal muscle mass, hand grip, and gait speed. Transplant Proc 49(9):2144–2152
Huang DD, Chen XX, Chen XY, Wang SL, Shen X, Chen XL, Yu Z, Zhuang CL (2016) Sarcopenia predicts 1-year mortality in elderly patients undergoing curative gastrectomy for gastric cancer: a prospective study. J Cancer Res Clin Oncol 142(11):1–10
Kaido T, Ogawa K, Fujimoto Y, Ogura Y, Hata K, Ito T, Tomiyama K, Yagi S, Mori A, Uemoto S (2013) Impact of sarcopenia on survival in patients undergoing living donor liver transplantation. Am J Transplant 13(6):1549–1556
Kawamura T, Makuuchi R, Tokunaga M, Tanizawa Y, Bando E, Yasui H, Aoyama T, Inano T, Terashima M (2018) Long-term outcomes of gastric cancer patients with preoperative sarcopenia. Ann Surg Oncol 4:1–8
Cai Z, Cai D, Yao D, Chen Y, Wang J, Li Y (2016) Associations between body composition and nutritional assessments and biochemical markers in patients with chronic radiation enteritis: a case-control study. Nutr J 15(1):57. https://doi.org/10.1186/s12937-016-0177-6
Makiura D, Ono R, Inoue J, Fukuta A, Kashiwa M, Miura Y, Oshikiri T, Nakamura T, Kakeji Y, Sakai Y (2018) Impact of sarcopenia on unplanned readmission and survival after Esophagectomy in patients with esophageal cancer. Ann Surg Oncol 25(2):1–9
Zhou CJ, Zhang FM, Zhang FY, Yu Z, Chen XL, Shen X, Zhuang CL, Chen XX (2017) Sarcopenia: a new predictor of postoperative complications for elderly gastric cancer patients who underwent radical gastrectomy. J Surg Res 211:137–146
Visser M, Deeg DP (2003) Low vitamin D and high parathyroid hormone levels as determinants of loss of muscle strength and muscle mass (sarcopenia): the Longitudinal Aging Study Amsterdam. J Clin Endocrinol Metab 88(12):5766–5772
Patrick K, Arny F, Juan L, Robert W, Evans WJ (2007) Effect of 10 days of bed rest on skeletal muscle in healthy older adults. Jama 297(16):1772–1774
Evans WJ, Farrell PA (2011) The aging pancreas: effects of aging on insulin secretion and action
Matteo C, Kritchevsky SB, Baumgartner RN, Atkinson HH, Penninx BWHJ, Leon L, Palla SL, Ambrosius WT, Tracy RP, Marco P (2005) Sarcopenia, obesity, and inflammation—results from the trial of angiotensin converting enzyme inhibition and novel cardiovascular risk factors study. Am J Clin Nutr 82(2):428
Baumgartner RN, Koehler KM, Gallagher D, Romero L, Heymsfield SB, Ross RR, Garry PJ, Lindeman RD (1998) Epidemiology of sarcopenia among the elderly in New Mexico. Am J Epidemiol 147(8):755–763
Evans WJ (2010) Skeletal muscle loss: cachexia, sarcopenia, and inactivity. Am J Clin Nutr 91(4):1123S–1127S
Chow WB, Rosenthal RA, Merkow RP, Ko CY, Esnaola NF (2012) Optimal preoperative assessment of the geriatric surgical patient: a best practices guideline from the American College of Surgeons National Surgical Quality Improvement Program and the American Geriatrics Society. J Am Coll Surg 215(4):453–466
Funding
This work was funded by the Postgraduate Research & Practice Innovation Program of Jiangsu Province awarded to Xu Xinyi.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Hua, H., Xu, X., Tang, Y. et al. Effect of sarcopenia on clinical outcomes following digestive carcinoma surgery: a meta-analysis. Support Care Cancer 27, 2385–2394 (2019). https://doi.org/10.1007/s00520-019-04767-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00520-019-04767-4