Abstract
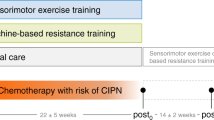
Chemotherapy-induced peripheral neuropathy (CIPN) is a prevalent and clinically relevant side effect of chemotherapy. The symptoms diminish patients’ quality of life and represent a decisive limiting factor for medical therapy. To date, effective treatment options are lacking. Specific exercise interventions have proven promising to target relevant symptoms. We conducted a prospective, four-armed, randomized, controlled trial, to evaluate the effects of sensorimotor training (SMT) and whole-body vibration training (WBV) on patients with CIPN. Participants (N = 40) were randomized to either one of two intervention groups (SMT N = 10 or WBV N = 10) or oncological control group (N = 10) and matched by gender and age with a healthy control (N = 10). The intervention groups exercised twice a week for 6 weeks. Primary endpoint was the reduction of CIPN-related symptoms (improve peripheral deep sensitivity, Achilles tendon reflex (ASR) and patellar tendon reflex (PSR), light-touch perception, sense of position, and lower leg strength). Secondary endpoints were nerve conduction velocity and amplitude, balance control, quality of life, and CIPN-related pain. Patients exercising improved sensory and associated motor symptoms. Significant intergroup differences were found for the tendon reflexes (ASR P = .017 and PSR P = .020), peripheral deep sensitivity (P = .010), and pain (P = .043). Furthermore, tendencies were found regarding the subjective improvement of symptoms (P = .075) and two subscales of the EORTC-QLQ-C30 questionnaire: pain (P = .054) and dyspnea (P = .054). The results for the SMT group were superior regarding the tendon reflexes, and a tendency regarding the subjective report of symptoms, while WBV was superior regarding pain. SMT and WBV behold a large potential to reduce CIPN-related symptoms and can be considered feasible and safe for patients with CIPN (compliance 97.5%, no adverse events).
Registration: DRKS00013027

Similar content being viewed by others
References
Seretny M, Currie GL, Sena ES, Ramnarine S, Grant R, MacLeod MR, Colvin LA, Fallon M (2014) Incidence, prevalence, and predictors of chemotherapy-induced peripheral neuropathy: a systematic review and meta-analysis. Pain 155:2461–2470
Wonders KY, Reigle BS, Drury DG (2010) Treatment strategies for chemotherapy-induced peripheral neuropathy: potential role of exercise. Oncol Rev 4:117–125
Pietrangeli A, Leandri M, Terzoli E, Jandolo B, Garufi C (2006) Persistence of high-dose oxaliplatin-induced neuropathy at long-term follow-up. Eur Neurol 56:13–16
Lehky TJ, Leonard GD, Wilson RH, Grem JL, Floeter MK (2004) Oxaliplatin-induced neurotoxicity: acute hyperexcitability and chronic neuropathy. Muscle Nerve 29:387–392
Kneis S, Wehrle A, Freyler K et al (2015) Balance impairments and neuromuscular changes in breast cancer patients with chemotherapy-induced peripheral neuropathy. Clin Neurophysiol. (2):1481–1490
Kolb NA, Smith AG, Singleton JR, Beck SL, Stoddard GJ, Brown S, Mooney K (2016) The association of chemotherapy-induced peripheral neuropathy symptoms and the risk of falling. JAMA Neurol 73:860–866
Winters-Stone KM, Horak F, Jacobs PG, Trubowitz P, Dieckmann NF, Stoyles S, Faithfull S (2017) Falls, functioning, and disability among women with persistent symptoms of chemotherapy-induced peripheral neuropathy. J Clin Oncol 35:2604–2612
Stubblefield MD, Burstein HJ, Burton AW et al (2009) NCCN Task Force report: management of neuropathy in cancer. J Natl Compr Canc Netw 7(Suppl 5):S1–S26 quiz S27–28
Ang CD, Alviar MJ, Dans AL et al (2008) Vitamin B for treating peripheral neuropathy. Cochrane Database Syst Rev; CD004573
Hershman DL, Lacchetti C, Dworkin RH, Lavoie Smith EM, Bleeker J, Cavaletti G, Chauhan C, Gavin P, Lavino A, Lustberg MB, Paice J, Schneider B, Smith ML, Smith T, Terstriep S, Wagner-Johnston N, Bak K, Loprinzi CL (2014) Prevention and management of chemotherapy-induced peripheral neuropathy in survivors of adult cancers: American Society of Clinical Oncology clinical practice guideline. J Clin Oncol 32:1941–1967
Streckmann F, Kneis S, Leifert JA, Baumann FT, Kleber M, Ihorst G, Herich L, Grüssinger V, Gollhofer A, Bertz H (2014a) Exercise program improves therapy-related side-effects and quality of life in lymphoma patients undergoing therapy. Ann Oncol 25:493–499
Streckmann F, Zopf EM, Lehmann HC, May K, Rizza J, Zimmer P, Gollhofer A, Bloch W, Baumann FT (2014b) Exercise intervention studies in patients with peripheral neuropathy: a systematic review. Sports Med 44:1289–1304
Gruber M, Gruber SB, Taube W et al (2007) Differential effects of ballistic versus sensorimotor training on rate of force development and neural activation in humans. J Strength Cond Res 21:274–282
Freeman MA, Dean MR, Hanham IW (1965) The etiology and prevention of functional instability of the foot. J Bone Joint Surg. British volume; 47: 678–685
Verhagen E, van der Beek A, Twisk J, Bouter L, Bahr R, van Mechelen W (2004) The effect of a proprioceptive balance board training program for the prevention of ankle sprains: a prospective controlled trial. Am J Sports Med 32:1385–1393
Granacher U, Gollhofer A, Strass D (2006) Training induced adaptations in characteristics of postural reflexes in elderly men. Gait Posture 24:459–466
Schwenk M, Grewal GS, Holloway D, Muchna A, Garland L, Najafi B (2016) Interactive sensor-based balance training in older cancer patients with chemotherapy-induced peripheral neuropathy: a randomized controlled trial. Gerontology 62:553–563
Kawanabe K, Kawashima A, Sashimoto I, Takeda T, Sato Y, Iwamoto J (2007) Effect of whole-body vibration exercise and muscle strengthening, balance, and walking exercises on walking ability in the elderly. Keio J Med 56:28–33
Rittweger J (2010) Vibration as an exercise modality: how it may work, and what its potential might be. Eur J Appl Physiol 108:877–904
Blottner D, Salanova M, Puttmann B et al (2006) Human skeletal muscle structure and function preserved by vibration muscle exercise following 55 days of bed rest. Eur J Appl Physiol 97:261–271
Spiliopoulou SI, Amiridis IG, Tsigganos G, Economides D, Kellis E (2010) Vibration effects on static balance and strength. Int J Sports Med 31:610–616
Bogaerts A, Delecluse C, Boonen S, Claessens AL, Milisen K, Verschueren SMP (2011) Changes in balance, functional performance and fall risk following whole body vibration training and vitamin D supplementation in institutionalized elderly women. A 6 month randomized controlled trial. Gait Posture 33:466–472
Schonsteiner SS, Bauder Missbach H, Benner A et al (2017) A randomized exploratory phase 2 study in patients with chemotherapy-related peripheral neuropathy evaluating whole-body vibration training as adjunct to an integrated program including massage, passive mobilization and physical exercises. Exp Hematol Oncol 6:5
Oyer DS, Saxon D, Shah A (2007) Quantitative assessment of diabetic peripheral neuropathy with use of the clanging tuning fork test. Endocr Pract 13:5–10
Cochrane DJ (2011) Vibration exercise: the potential benefits. Int J Sports Med 32:75–99
Aaronson NKAS, Bergman B, Bullinger M, Cull A, Duez NJ, Filiberti A, Flechtner H, Fleishman SB dHJ, Kaasa S, Klee MC, Osoba D, Razavi D, Rofe PB, Schraub S, SM SKCA, Takeda F (1993) The European Organisation for Research and Treatment of Cancer QLQ-C30: a quality-of-life instrument for use in international clinical trials in oncology. J Natl Cancer Inst 85:365–376
Bennett MI, Attal N, Backonja MM, Baron R, Bouhassira D, Freynhagen R, Scholz J, Tölle TR, Wittchen HU, Jensen TS (2007) Using screening tools to identify neuropathic pain. Pain 127:199–203
Cohen J (1988) Statistical Power Analysis for the Behavioral Sciences, Erlbaum, Mahwah, NJ, USA
Wei LJ (1978) The adaptive biased coin design for sequential experiments. The Annals of Statistics; 6(1): 92–100
Faul F, Erdfelder E, Lang AG, Buchner A (2007) G*Power: A flexible statistical power analysis program for the social, behavioral, and biomedical sciences. Behavior Research Methods; 39:175–191
Gollhofer A (2003) Proprioceptive training: considerations for strength and power production. In: P.V.K. (ed) Strenght and Power in Sport, 2nd edn. Blackwell Publishing, Oxford, pp 331–342
Sjostrom PJ, Rancz EA, Roth A, Hausser M (2008) Dendritic excitability and synaptic plasticity. Physiol Rev 88:769–840
Taube W, Gruber M, Gollhofer A (2008) Spinal and supraspinal adaptations associated with balance training and their functional relevance. Acta Physiol (Oxf) 193:101–116
Park JS, Kim S, Hoke A (2015) An exercise regimen prevents development paclitaxel induced peripheral neuropathy in a mouse model. J Peripher Nerv Syst 20:7–14
Park JS, Hoke A (2014) Treadmill exercise induced functional recovery after peripheral nerve repair is associated with increased levels of neurotrophic factors. PLoS One 9:e90245
Acknowledgements
We acknowledge the contributions of Julia Rizza and Kathrin May as well as the advisory support of Prof. Wolfgang Potthast and Dr. Angela Höhne regarding the balance assessment. We are furthermore grateful to the patients and especially the healthy matched participants for their support and volunteering.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Our prospective, single-center, four-armed RCT was approved by the ethics committee of the German Sport University. All patients gave written informed consent in accordance with the Declaration of Helsinki.
Conflict of interest
The authors declare that they have no conflicts of interest.
Additional information
Relevance/Novelty of manuscript
Chemotherapy-induced peripheral neuropathy (CIPN) is a highly prevalent and clinically relevant side effect of chemotherapy. The symptoms severely diminish patients’ quality of life and represent a decisive limiting factor for medical therapy, consequently affecting the clinical outcome. To date, effective treatment options are lacking. Specific exercise interventions have now proven promising to reduce sensory symptoms of CIPN, revealing a high potential as treatment option, thus impacting supportive therapy in oncology.
Electronic supplementary material
ESM 1
(DOCX 30 kb)
Rights and permissions
About this article
Cite this article
Streckmann, F., Lehmann, H., Balke, M. et al. Sensorimotor training and whole-body vibration training have the potential to reduce motor and sensory symptoms of chemotherapy-induced peripheral neuropathy—a randomized controlled pilot trial. Support Care Cancer 27, 2471–2478 (2019). https://doi.org/10.1007/s00520-018-4531-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00520-018-4531-4