Abstract
Purpose
The purpose of this study was to evaluate objectively the effectiveness of photobiomodulation therapy (PBMT) for the prevention of acute radiation dermatitis (ARD) by using biophysical skin measurements.
Methods
A randomized, placebo-controlled trial with 120 breast cancer patients who underwent an identical radiotherapy (RT) regimen post-lumpectomy was performed (TRANSDERMIS trial). Patients were randomized to receive PBM (808 nm CW/905 nm pulsed, 168 mW/cm2, spot size 19.6 cm2, fluence 4 J/cm2) or placebo treatments from the first day of RT (2×/week). Biophysical skin measurements were collected to assess the skin pigmentation and barrier function. Measurements were collected at the first day of RT, a RT dose of 40 Gray (Gy), and the end of RT (66 Gy).
Results
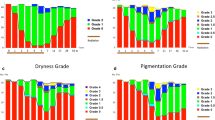
The incidence of moist desquamation was significantly higher in the control than in the PBMT group at the end of RT (30 vs. 7%, respectively, odds ratio = 6, p = 0.004). The biophysical skin measures showed that the mean percentage change from the baseline transepidermal water loss (TEWL), erythema, and melanin values was significantly higher in the control than in the PBMT group at the end of RT (ps < 0.05). Logistic regression analysis revealed that the risk on moist desquamation was significantly increased for patients with a large (> 800 cc) breast volume (odds ratio = 4, p = 0.017).
Conclusions
This is the first randomized controlled trial demonstrating by objective measurements that PBMT is effective in reducing the incidence of moist desquamation in breast cancer patients undergoing RT. Additionally, a large breast volume is an important risk factor for the development of moist desquamation.


Similar content being viewed by others
Notes
DIBH was used when the patients matched the following criteria: bilateral breast cancer; left-sided breast cancer and lymph node metastases under the age of 70 years; left-sided breast cancer and lymph node metastases above the age of 70 years and undergoing chemotherapy; left-sided breast cancer without lymph node metastasis but with a MHD ≥ 35 Gy. DIBH was applied using the Varian Real-Time Position Management (RPM) gating system (Varian Medical System, Palo Alto, CA).
References
Wells M, MacBride S (2003) Radiation skin reactions. Elsevier, New York
Seite S, Bensadoun RJ, Mazer JM (2017) Prevention and treatment of acute and chronic radiodermatitis. Breast Cancer (Dove Med Press) 9:551–557. https://doi.org/10.2147/BCTT.S149752
Robijns J, Laubach H-J (2018) Acute and chronic radiodermatitis: clinical signs, pathophysiology, risk factors and management options. JEWDS 15(1):2–9. https://doi.org/10.1097/01.EWX.0000529960.52517.4c
Proksch E, Brandner JM, Jensen JM (2008) The skin: an indispensable barrier. Exp Dermatol 17(12):1063–1072
Cox JD, Stetz J, Pajak TF (1995) Toxicity criteria of the Radiation Therapy Oncology Group (RTOG) and the European Organization for Research and Treatment of Cancer (EORTC). Int J Radiat Oncol Biol Phys 31(5):1341–1346. https://doi.org/10.1016/0360-3016(95)00060-C
Hu SC, Hou MF, Luo KH, Chuang HY, Wei SY, Chen GS, Chiang W, Huang CJ (2014) Changes in biophysical properties of the skin following radiotherapy for breast cancer. J Dermatol 41(12):1087–1094. https://doi.org/10.1111/1346-8138.12669
Wong RK, Bensadoun RJ, Boers-Doets CB, Bryce J, Chan A, Epstein JB, Eaby-Sandy B, Lacouture ME (2013) Clinical practice guidelines for the prevention and treatment of acute and late radiation reactions from the MASCC Skin Toxicity Study Group. Support Care Cancer 21(10):2933–2948. https://doi.org/10.1007/s00520-013-1896-2
Hamblin M, Ferraresi C, Huang YY, de Freitas LF, Carroll J (2018) Low-Level Light Therapy: Photobiomodulation. Tutorial Texts in Optical Engineering, vol TT115. SPIE Press, Bellingham 390
Schindl M, Kerschan K, Schindl A, Schon H, Heinzl H, Schindl L (1999) Induction of complete wound healing in recalcitrant ulcers by low-intensity laser irradiation depends on ulcer cause and size. Photodermatol Photoimmunol Photomed 15(1):18–21
DeLand MM, Weiss RA, McDaniel DH, Geronemus RG (2007) Treatment of radiation-induced dermatitis with light-emitting diode (LED) photomodulation. Lasers Surg Med 39(2):164–168. https://doi.org/10.1002/lsm.20455
Fife D, Rayhan DJ, Behnam S, Ortiz A, Elkeeb L, Aquino L, Eduardo Roa D, Ramsinghani N, Kuo J, Newcomb R, Zachary CB, Kelly KM (2010) A randomized, controlled, double-blind study of light emitting diode photomodulation for the prevention of radiation dermatitis in patients with breast cancer. Dermatol Surg 36(12):1921–1927. https://doi.org/10.1111/j.1524-4725.2010.01801.x
Strouthos I, Chatzikonstantinou G, Tselis N, Bon D, Karagiannis E, Zoga E, Ferentinos K, Maximenko J, Nikolettou-Fischer V, Zamboglou N (2017) Photobiomodulation therapy for the management of radiation-induced dermatitis : a single-institution experience of adjuvant radiotherapy in breast cancer patients after breast conserving surgery. Strahlenther Onkol 193(6):491–498. https://doi.org/10.1007/s00066-017-1117-x
Censabella S, Claes S, Robijns J, Bulens P, Mebis J (2016) Photobiomodulation for the management of radiation dermatitis: the DERMIS trial, a pilot study of MLS® laser therapy in breast cancer patients. Support Care Cancer 24:1–9. https://doi.org/10.1007/s00520-016-3232-0
Robijns J, Censabella S, Claes S, Pannekoeke L, Bussé L, Colson D, Kaminski I, Bulens P, Maes A, Noé L, Brosens M, Timmermans A, Lambrichts I, Somers V, Mebis J (2018) Prevention of acute radiodermatitis by photobiomodulation: a randomized, placebo-controlled trial in breast cancer patients (TRANSDERMIS trial). Lasers Surg Med 50(7):763–771. https://doi.org/10.1002/lsm.22804
Burnet NG, Thomas SJ, Burton KE, Jefferies SJ (2004) Defining the tumour and target volumes for radiotherapy. Cancer Imaging 4(2):153–161. https://doi.org/10.1102/1470-7330.2004.0054
Nair RG, Bensadoun RJ (2016) Mitigation of cancer therapy side-effects with light. Morgan & Claypool Publishers, San Rafael
Zecha JA, Raber-Durlacher JE, Nair RG, Epstein JB, Elad S, Hamblin MR, Barasch A, Migliorati CA, Milstein DM, Genot MT, Lansaat L, van der Brink R, Arnabat-Dominguez J, van der Molen L, Jacobi I, van Diessen J, de Lange J, Smeele LE, Schubert MM, Bensadoun RJ (2016) Low-level laser therapy/photobiomodulation in the management of side effects of chemoradiation therapy in head and neck cancer: part 2: proposed applications and treatment protocols. Support Care Cancer 24(6):2793–2805. https://doi.org/10.1007/s00520-016-3153-y
Pinnagoda J, Tupker RA, Agner T, Serup J (1990) Guidelines for transepidermal water loss (TEWL) measurement. A report from the Standardization Group of the European Society of Contact Dermatitis. Contact Dermatitis 22(3):164–178
Rogiers V, E. Group (2001) EEMCO guidance for the assessment of transepidermal water loss in cosmetic sciences. Skin Pharmacol Appl Ski Physiol 14(2):117–128 56341
Heinrich U, Koop U, Leneveu-Duchemin MC, Osterrieder K, Bielfeldt S, Chkarnat C, Degwert J, Hantschel D, Jaspers S, Nissen HP, Rohr M, Schneider G, Tronnier H (2003) Multicentre comparison of skin hydration in terms of physical-, physiological- and product-dependent parameters by the capacitive method (Corneometer CM 825). Int J Cosmet Sci 25(1–2):45–53. https://doi.org/10.1046/j.1467-2494.2003.00172.x
Clarys P, Alewaeters K, Lambrecht R, Barel AO (2000) Skin color measurements: comparison between three instruments: the Chromameter(R), the DermaSpectrometer(R) and the Mexameter(R). Skin Res Technol 6(4):230–238
Yamazaki H, Yoshida K, Kobayashi K, Tsubokura T, Kodani N, Aibe N, Ikeno H, Nishimura T (2012) Assessment of radiation dermatitis using objective analysis for patients with breast cancer treated with breast-conserving therapy: influence of body weight. Jpn J Radiol 30(6):486–491. https://doi.org/10.1007/s11604-012-0073-8
Primavera G, Carrera M, Berardesca E, Pinnaro P, Messina M, Arcangeli G (2006) A double-blind, vehicle-controlled clinical study to evaluate the efficacy of MAS065D (XClair), a hyaluronic acid-based formulation, in the management of radiation-induced dermatitis. Cutan Ocul Toxicol 25(3):165–171. https://doi.org/10.1080/15569520600860009
Yoshida EJ, Chen H, Torres MA, Curran WJ, Liu T (2011) Spectrophotometer and ultrasound evaluation of late toxicity following breast-cancer radiotherapy. Med Phys 38(10):5747–5755. https://doi.org/10.1118/1.3633942
Iacovelli NA, Naimo S, Bonfantini F, Cavallo A, Bossi P, Fallai C, Pignoli E, Alfieri S, Bergamini C, Favales F, Orlandi E (2017) Preemptive treatment with Xonrid(R), a medical device to reduce radiation induced dermatitis in head and neck cancer patients receiving curative treatment: a pilot study. Support Care Cancer 25(6):1787–1795. https://doi.org/10.1007/s00520-017-3569-z
Nystrom J, Geladi P, Lindholm-Sethson B, Rattfelt J, Svensk AC, Franzen L (2004) Objective measurements of radiotherapy-induced erythema. Skin Res Technol 10(4):242–250
Yamazaki H, Yoshida K, Kotsuma T, Kuriyama K, Masuda N, Nishimura T, Kobayashi K, Tsubokura T, Nishimura T (2009) Longitudinal practical measurement of skin color and moisture during and after breast-conserving therapy: influence of neoadjuvant systemic therapy. Jpn J Radiol 27(8):309–315. https://doi.org/10.1007/s11604-009-0345-0
Hamblin MR (2017) Mechanisms and applications of the anti-inflammatory effects of photobiomodulation. AIMS Biophys 4(3):337–361. https://doi.org/10.3934/biophy.2017.3.337
Gupta A, Keshri GK, Yadav A, Gola S, Chauhan S, Salhan AK, Bala Singh S (2015) Superpulsed (Ga-As, 904 nm) low-level laser therapy (LLLT) attenuates inflammatory response and enhances healing of burn wounds. J Biophotonics 8(6):489–501. https://doi.org/10.1002/jbio.201400058
Khoury JG, Goldman MP (2008) Use of light-emitting diode photomodulation to reduce erythema and discomfort after intense pulsed light treatment of photodamage. J Cosmet Dermatol 7(1):30–34. https://doi.org/10.1111/j.1473-2165.2008.00358.x
Barolet D, Boucher A (2008) LED photoprevention: reduced MED response following multiple LED exposures. Lasers Surg Med 40(2):106–112. https://doi.org/10.1002/lsm.20615
Chen CH, Wang CZ, Wang YH, Liao WT, Chen YJ, Kuo CH, Kuo HF, Hung CH (2014) Effects of low-level laser therapy on M1-related cytokine expression in monocytes via histone modification. Mediat Inflamm 2014:625048. https://doi.org/10.1155/2014/625048
Kim HK, Min KO, Choi JH, Kim SH (2016) Effects of low-level laser therapy, electroacupuncture, and radiofrequency on the pigmentation and skin tone of adult women. J Phys Ther Sci 28(5):1407–1411. https://doi.org/10.1589/jpts.28.1407
Lee SY, You CE, Park MY (2007) Blue and red light combination LED phototherapy for acne vulgaris in patients with skin phototype IV. Lasers Surg Med 39(2):180–188. https://doi.org/10.1002/lsm.20412
Barolet D (2018) Photobiomodulation in dermatology: harnessing light from visible to near infrared. MRA 6(1). https://doi.org/10.18103/mra.v6i1.1610
Baroni A, Buommino E, De Gregorio V, Ruocco E, Ruocco V, Wolf R (2012) Structure and function of the epidermis related to barrier properties. Clin Dermatol 30(3):257–262. https://doi.org/10.1016/j.clindermatol.2011.08.007
Schmuth M, Wimmer MA, Hofer S, Sztankay A, Weinlich G, Linder DM, Elias PM, Fritsch PO, Fritsch E (2002) Topical corticosteroid therapy for acute radiation dermatitis: a prospective, randomized, double-blind study. Br J Dermatol 146(6):983–991
Jensen JM, Gau T, Schultze J, Lemmnitz G, Folster-Holst R, May T, Abels C, Proksch E (2011) Treatment of acute radiodermatitis with an oil-in-water emulsion following radiation therapy for breast cancer: a controlled, randomized trial. Strahlenther Onkol 187(6):378–384. https://doi.org/10.1007/s00066-011-2224-8
Park SY, Kim JH, Cho SI, Kim KI, Cho HJ, Park CW, Lee CH, Kim HO (2014) Induction of a hardening phenomenon and quantitative changes of ceramides in stratum corneum. Ann Dermatol 26(1):35–42. https://doi.org/10.5021/ad.2014.26.1.35
Hawkins DH, Abrahamse H (2006) The role of laser fluence in cell viability, proliferation, and membrane integrity of wounded human skin fibroblasts following helium-neon laser irradiation. Lasers Surg Med 38(1):74–83. https://doi.org/10.1002/lsm.20271
Lanzafame RJ, Stadler I, Kurtz AF, Connelly R, Peter TA Sr, Brondon P, Olson D (2007) Reciprocity of exposure time and irradiance on energy density during photoradiation on wound healing in a murine pressure ulcer model. Lasers Surg Med 39(6):534–542. https://doi.org/10.1002/lsm.20519
Rizzi M, Migliario M, Tonello S, Rocchetti V, Reno F (2018) Photobiomodulation induces in vitro re-epithelialization via nitric oxide production. Lasers Med Sci 33:1003–1008. https://doi.org/10.1007/s10103-018-2443-7
Sperandio FF, Simoes A, Correa L, Aranha AC, Giudice FS, Hamblin MR, Sousa SC (2015) Low-level laser irradiation promotes the proliferation and maturation of keratinocytes during epithelial wound repair. J Biophotonics 8(10):795–803. https://doi.org/10.1002/jbio.201400064
Censabella S, Claes S, Orlandini M, Braekers R, Bulens P (2017) Efficacy of a hydroactive colloid gel versus historical controls for the prevention of radiotherapy-induced moist desquamation in breast cancer patients. Eur J Oncol Nurs 29:1–7. https://doi.org/10.1016/j.ejon.2017.04.003
De Langhe S, Mulliez T, Veldeman L, Remouchamps V, van Greveling A, Gilsoul M, De Schepper E, De Ruyck K, De Neve W, Thierens H (2014) Factors modifying the risk for developing acute skin toxicity after whole-breast intensity modulated radiotherapy. BMC Cancer 14:711. https://doi.org/10.1186/1471-2407-14-711
Acknowledgments
The corresponding author, Mrs. Jolien Robijns, received the Young Investigator Award of the MASCC for her scientific abstract.
Funding
This research is part of the Limburg Clinical Research Program (LCRP) UHasselt-ZOL-Jessa, financially supported by the foundation Limburg Sterk Merk, province of Limburg, Flemish government, Hasselt University, Ziekenhuis Oost-Limburg, and Jessa Hospital. Additionally, this research is supported by Kom op Tegen Kanker, Limburgs Kankerfonds, and ASA Srl.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no competing interests.
Ethical approval
The ethics committees of the Jessa Hospital and the University of Hasselt approved the study (B243201524443). All procedures performed in the study were in accordance with the ethical standards of the institutional and national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Electronic supplementary material
ESM 1
(DOCX 130 kb)
Rights and permissions
About this article
Cite this article
Robijns, J., Censabella, S., Claes, S. et al. Biophysical skin measurements to evaluate the effectiveness of photobiomodulation therapy in the prevention of acute radiation dermatitis in breast cancer patients. Support Care Cancer 27, 1245–1254 (2019). https://doi.org/10.1007/s00520-018-4487-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00520-018-4487-4