Abstract
Background
Human papillomavirus (HPV)-related cancers have been associated with different demographic profiles and disease characteristics than HPV-unrelated cancers in head and neck patients, but distress and other symptoms have not been compared. The aim of this study was to assess whether distress levels, fatigue, pain, anxiety, depression, and common psychological and practical problems differ between head and neck cancer patients with HPV-related vs. HPV-unrelated carcinomas (using oropharyngeal carcinoma (OPC) and non-OPC cancers as surrogates for HPV status).
Methods
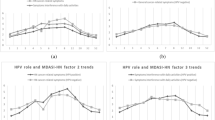
Distress, depression, anxiety, fatigue, pain, and common problems were examined in 56 OPC and 90 non-OPC patients at 4 timepoints during the first year following diagnosis. Two-level hierarchical linear modeling was used to examine effects.
Results
The HPV-related OPC group was more likely to be younger (p = 0.05), Caucasian (p = 0.001), non-smokers (p = 0.01), earn more (p = 0.04), and present with more advanced stage (p < 0.0001). At baseline, OPC patients reported only higher pain scores (p = 0.01) than non-OPC patients. Total problems decreased more in the OPC group (p = 0.08) than the non-OPC group from baseline to 12-month follow-up. In both groups, scores on distress, depression, psychosocial problems, and practical problems decreased similarly over time.
Conclusions
Despite a difference in the clinico-demographic characteristics of HPV-related vs. HPV-unrelated patients, only baseline pain levels and total problems over time differed between the two groups.


Similar content being viewed by others
References
Carlson L, Bultz B (2003) Cancer distress screening needs, models and methods. J Psychosom Res 55(5):403–409
Carlson L, Angen M, Callum J, Goodey E, Koopmans J, Lamont L, MacRae J, Martin M, Pelletier G, Robinson J, Simplson J, Speca M, Tillotson L, Bultz B (2004) High levels of untreated distress and fatigue in cancer patients. Br J Cancer 90(12):2297–2304
Zabora J, BrintzenhofeSzoc K, Curbow B, Hooker C, Piantadosi S (2001) The prevalence of psychological distress by cancer site. Psychooncology 10(1):19–28
Holland J, Bultz B (2007) The NCCN guideline for distress management: a case for making distress the sixth vital sign. J Natl Compr Cancer Netw 5(1):3–7
National Comprehensive Cancer Network (2012). Practice guidelines in oncolology-v.2.2012: Distress management
Bultz B, Waller A, Callum J, Jones P, Halland J, Groff S, Leckie C, Shirt L, Blanchard S, Lau H, Easaw J, Fassbender K, Carlson L (2013) Implementing routine screening for distress, the sixth vital sign, for patients with head and neck and neurologic cancers. J Natl Compr Cancer Netw 11(10):1249–1261
Auluck A, Hislop G, Bajdik C, Poh C, Zhang L, Rosin M (2010) Trends in oropharyngeal and oral cavity cancer incidence of human papillomavirus (HPV)-related and HPV-unrelated sites in a multicultural population. Cancer 116(11):2635–2644
Hocking J, Stein A, Conway E, Regan D, Grulich A, Law M, Brotherton J (2011) Head and neck cancer in Australia between 1982-2005 show increasing incidence of potentially HPV-associated oropharyngeal cancers. Br J Cancer 104(5):886–891
Ryerson A, Peters E, Coughlin S, Chen V, Gillison M, Reichman M, Wu X, Chaturvedi A, Kawaoka K (2008) Burden of potentially human papillomavirus-associated cancers of the oropharynx and oral cavity in the US, 1998-2003. Cancer 113(10 Suppl):2901–2909
Chaturvedi A, Engels E, Anderson W, Gillison M (2008) Incidence trends for human papillomavirus-related and -unrelated oral squamous cell carcinomas in the United States. J Clin Oncol 26(4):612–619
Herrero R, Castellsague X, Pawlita M, Lissowska J, Kee F, Balaram P, Rakjumar T, Sridhar H, Rose B, Pintos J, Fernandez L, Idris A, Sanchez M, Nieto A, Talamini R, Tavani A, Bosch F, Reidel U, Snijders P, Meijer C, Viscidi R, Munoz N, Franceschi S (2003) Human papillomavirus and oral cancer: the International Agency for Research on Cancer Multicentre Study. J Natl Cancer Inst 95(23):1772–1783
Gold D (2012) The psychosocial care needs of patients with HPV-related head and neck cancer. Otolaryngol Clin N Am 45:879–897
Carlson L, Waller A, Groff S, Zhong L, Bultz B (2012) Online screening for distress, the 6th vital sign, in newly diagnosed oncology outpatients: randomized controlled trial of computerized vs. personalized triage. Br J Cancer 107(4):617–625. doi:10.1038/bjc.2012.309
Carlson L, Waller A, Groff S, Giese-Davis J, Bultz B (2013) What goes up does not always come down: patterns of distress, physical and psychosocial morbidity in people with cancer over a one year period. Psychooncology 22:168–176
National Comprehensive Cancer Network Incorporated (2016) Practice guidelines in oncology—v.1.2016. Distress management. National Comprehensive Cancer Network, Inc., Fort Washington
National Comprehensive Cancer Network Incorporated (2017) Practice guidelines in oncology—v.2.2017. Cancer-related fatigue. National Comprehensive Cancer Network, Inc., Fort Washington
Butt Z, Wagner L, Beaumont J, Paice J, Peterman A, Shevrin D, Von Roenn J, Carro G, Straus J, Muir J, Cella D (2008) Use of a single-item screening tool to detect clinically significant fatigue, pain, distress, and anorexia in ambulatory cancer practice. J Pain Symptom Manag 35(1):20–30
Bultz B, Groff S, Fitch M, Cancer Journey Action Group (CJAG) (2009) Guide to implementing screening for distress, the 6th vital sign. Part A: background, recommendations, and implementation. CPAC Guide to implementing screening: www.partnershipagainstcancer.ca/wp-content/uploads/2.4.0.1.4.5-Guide_CJAG.pdf
Linden W, Wodermaier A, McKenzie R, Barroetavena M, Yi D, Doll R (2009) The psychosocial screen for cancer (PSSCAN): further validation and normative data. Health Qual Life Outcomes 7(16):1–8
Howren M, Christensen A, Karnell L, Van Liew J, Funk G (2012) Influence of pretreatment social support on health-related quality of life in head and neck cancer survivors: results from a prospective study. Head Neck. doi:10.1002/hed.23029
Neilson K, Pollard A, Boonzaier A, Corry J, Castle D, Smith D, Trauer T, Couper J (2012) A longitudinal study of distress (depression and anxiety) up to 18 months after radiotherapy for head and neck cancer. Psychooncology. doi:10.1002/pon.3228
Landis S, El-Hariry I, van Herk-Sukel M, van den Haak P, Janssen-Heijnen M, Penning-van Beest F, Herings R (2012) Prevalence and incidence of acute and chronic comorbidity in patients with squamous cell carcinoma of the head and neck. Head Neck 34(2):238–244
Sherman A, Simonton S, Adams D, Vural E, Hanna E (2000) Coping with head and neck cancer during different phases of treatment. Head Neck 22(8):787–793
de Graeff A, de Leeuw R, Ros W, Hordijk G, Blijham G, Winnubst J (2000) Pretreatment factors predicting quality of life after treatment for head and neck cancer. Head Neck 22(4):398–407
Isayeva T, Li Y, Maswahu D, Branwein-Gensier M (2012) Human papillomavirus in non-oropharyngeal head and neck cancers: a systematic literature review. Head Neck Pathol 6(Suppl 1):S104–S120. doi:10.1007/s12105-012-0368-1
Mehanna H, Beech T, Nicholson T, El-Hariry I, McConkey C, Paleri V, Roberts S (2012) Prevalence of human papillomavirus in oropharyngeal and nonoropharyngeal head and neck cancer—systematic review and meta-analysis of trends by time and region. Head Neck 35(5):747–755
Acknowledgements
The collection of distress screening data was funded by the Alberta Cancer Research Institute Research Initiatives Program/Alberta Cancer Foundation.
Author information
Authors and Affiliations
Contributions
MS collected the clinical data, assimilated the existing databases, and participated in drafting the manuscript. LC was involved in the design and coordination of the study, data analysis and interpretation, and as well as helped to draft the manuscript. HL participated in the design of the study and manuscript preparation. LZ performed the statistical analyses and interpretation, and drafted the methods and results section of the manuscript. BB spearheaded the collection of the distress data, reviewed, and edited the manuscript. AW participated in collection of the distress data, reviewed and edited the manuscript. SG participated in the collection the distress data, and edited the manuscript. DH conceived of the study, participated in its design and coordination and helped to draft and edit the manuscript.
All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
The Alberta Cancer Research Ethics Committee approved this study.
Competing interests
The authors declare that they have no competing interests.
Author’s information
LEC holds the Enbridge Research Chair in Psychosocial Oncology, cofunded by the Canadian Cancer Society and Alberta Cancer Foundation, and along with BDB has been responsible for developing and testing methods of implementing screening for distress as the “6th vital sign” in cancer care worldwide. The data in this paper was extracted from clinical trials which evaluated the efficacy of routine online screening for distress on subsequent psychosocial and physical outcomes.
Role of the funding source
The Alberta Cancer Research Institute Research Initiatives Program/Alberta Cancer Foundation provided funding for the collection of distress screening data used in this study.
Rights and permissions
About this article
Cite this article
Schorr, M., Carlson, L.E., Lau, H.Y. et al. Distress levels in patients with oropharyngeal vs. non-oropharyngeal squamous cell carcinomas of the head and neck over 1 year after diagnosis: a retrospective cohort study. Support Care Cancer 25, 3225–3233 (2017). https://doi.org/10.1007/s00520-017-3733-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00520-017-3733-5