Abstract
Objective
The aim of this study was to compare the effectiveness of two sedative regimens, a benzodiazepine with either meperidine or fentanyl, in relieving pain in patients with cervical cancer undergoing intracavitary brachytherapy in terms of pain score and quality of life.
Methods
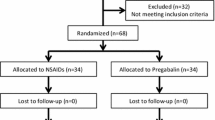
Forty unselected outpatients undergoing brachytherapy (160 fractions) were enrolled with informed consent and randomized to receive a benzodiazepine with either meperidine or fentanyl. The perceived pain score according to a standard 10-item numeric rating scale was collected every 15 min during the procedure, and the perceived quality of life was determined at the end of each procedure using the EuroQol five-dimension questionnaire. The patients and medical staff members directly involved with the procedure were blinded to the medication used.
Results
The patients’ pain levels were mild in both analgesic groups. Meperidine appeared to be slightly more effective than fentanyl, although the differences in the average pain score and quality of life were not statistically significant.
Conclusion
Both meperidine and fentanyl in combination with benzodiazepine were effective in relieving pain and discomfort in patients undergoing brachytherapy.
Trial Registration
NCT02684942, ClinicalTrials.gov


Similar content being viewed by others
References
Torre LA, Bray F, Siegel RL, Ferlay J, Lortet-Tieulent J, Jemal A (2015) Global cancer statistics, 2012. CA Cancer J Clin 65:87–108
Global Burden of Disease Cancer C, Fitzmaurice C, Dicker D, Pain A, Hamavid H, Moradi-Lakeh M et al (2015) The global burden of cancer 2013. JAMA Oncol 1:505–527
Siegel RL, Miller KD, Jemal A (2016) Cancer statistics, 2016. CA Cancer J Clin 66:7–30
Sankaranarayanan R, Nene BM, Shastri SS, Jayant K, Muwonge R, Budukh AM et al (2009) HPV screening for cervical cancer in rural India. N Engl J Med 360:1385–1394
Lukka H, Hirte H, Fyles A, Thomas G, Elit L, Johnston M et al (2002) Concurrent cisplatin-based chemotherapy plus radiotherapy for cervical cancer—a meta-analysis. Clin Oncol (R Coll Radiol) 14:203–212
Morris M, Eifel PJ, Lu J, Grigsby PW, Levenback C, Stevens RE et al (1999) Pelvic radiation with concurrent chemotherapy compared with pelvic and para-aortic radiation for high-risk cervical cancer. N Engl J Med 340:1137–1143
Waggoner SE (2003) Cervical cancer. Lancet 361:2217–2225
Rose PG, Bundy BN, Watkins EB, Thigpen JT, Deppe G, Maiman MA et al (1999) Concurrent cisplatin-based radiotherapy and chemotherapy for locally advanced cervical cancer. N Engl J Med 340:1144–1153
Eifel PJ, Thoms WW Jr, Smith TL, Morris M, Oswald MJ (1994) The relationship between brachytherapy dose and outcome in patients with bulky endocervical tumors treated with radiation alone. Int J Radiat Oncol Biol Phys 28:113–118
Lanciano RM, Martz K, Coia LR, Hanks GE (1991) Tumor and treatment factors improving outcome in stage III-B cervix cancer. Int J Radiat Oncol Biol Phys 20:95–100
Kirchheiner K, Czajka-Pepl A, Ponocny-Seliger E, Scharbert G, Wetzel L, Nout RA et al (2014) Posttraumatic stress disorder after high-dose-rate brachytherapy for cervical cancer with 2 fractions in 1 application under spinal/epidural anesthesia: incidence and risk factors. Int J Radiat Oncol Biol Phys 89:260–267
Bhanabhai H, Samant R, E C, Grenier L, Lowry S (2013) Pain assessment during conscious sedation for cervical cancer high-dose-rate brachytherapy. Curr Oncol 20:e307–e310
Benrath J, Kozek-Langenecker S, Hupfl M, Lierz P, Gustorff B (2006) Anaesthesia for brachytherapy—51/2 yr of experience in 1622 procedures. Br J Anaesth 96:195–200
Smith MD, Todd JG, Symonds RP (2002) Analgesia for pelvic brachytherapy. Br J Anaesth 88:270–276
Chen HC, Leung SW, Wang CJ, Sun LM, Fang FM, Huang EY et al (1998) Local vaginal anesthesia during high-dose-rate intracavitary brachytherapy for cervical cancer. Int J Radiat Oncol Biol Phys 42:541–544
Nguyen TV, Petereit DG (1998) High-dose-rate brachytherapy for medically inoperable stage I endometrial cancer. Gynecol Oncol 71:196–203
Petereit DG, Sarkaria JN, Chappell RJ (1998) Perioperative morbidity and mortality of high-dose-rate gynecologic brachytherapy. Int J Radiat Oncol Biol Phys 42:1025–1031
Hjermstad MJ, Fayers PM, Haugen DF, Caraceni A, Hanks GW, Loge JH et al (2011) Studies comparing numerical rating scales, verbal rating scales, and visual analogue scales for assessment of pain intensity in adults: a systematic literature review. J Pain Symptom Manag 41:1073–1093
Sakthong P, Sonsa-Ardjit N, Sukarnjanaset P, Munpan W (2015) Psychometric properties of the EQ-5D-5L in Thai patients with chronic diseases. Qual Life Res 24:3015–3022
Lim KH, Lu JJ, Wynne CJ, Back MF, Mukherjee R, Razvi K et al (2004) A study of complications arising from different methods of anesthesia used in high-dose-rate brachytherapy for cervical cancer. Am J Clin Oncol 27:449–451
Watanabe Nemoto M, Nozaki-Taguchi N, Togasaki G, Kanazawa A, Kurokawa M, Harada R et al (2015) New approach to relieving pain and distress during high-dose-rate intracavitary irradiation for cervical cancer. Brachytherapy 14:642–647
Soysal S, Karcioglu O, Demircan A, Topacoglu H, Serinken M, Ozucelik N et al (2004) Comparison of meperidine plus midazolam and fentanyl plus midazolam in procedural sedation: a double-blind, randomized controlled trial. Adv Ther 21:312–321
Ali S, Davidson DL, Gremse DA (2004) Comparison of fentanyl versus meperidine for analgesia in pediatric gastrointestinal endoscopy. Dig Dis Sci 49:888–891
Robertson DJ, Jacobs DP, Mackenzie TA, Oringer JA, Rothstein RI (2009) Clinical trial: a randomized, study comparing meperidine (pethidine) and fentanyl in adult gastrointestinal endoscopy. Aliment Pharmacol Ther 29:817–823
Dzeletovic I, Harrison ME, Crowell MD, Ramirez FC, Yows CR, Harris LA et al (2013) Impact of fentanyl in lieu of meperidine on endoscopy unit efficiency: a prospective comparative study in patients undergoing EGD. Gastrointest Endosc 77:883–887
Rollison B, Strang P (1995) Pain, nausea and anxiety during intra-uterine brachytherapy of cervical carcinomas. Support Care Cancer 3:205–207
Isoyama-Shirakawa Y, Nakamura K, Abe M, Kunitake N, Matsumoto K, Ohga S et al (2015) Caudal epidural anesthesia during intracavitary brachytherapy for cervical cancer. J Radiat Res 56:583–587
Agostoni M, Fanti L, Arcidiacono PG, Gemma M, Strini G, Torri G et al (2007) Midazolam and pethidine versus propofol and fentanyl patient controlled sedation/analgesia for upper gastrointestinal tract ultrasound endoscopy: a prospective randomized controlled trial. Dig Liver Dis 39:1024–1029
Ferrandina G, Mantegna G, Petrillo M, Fuoco G, Venditti L, Terzano S et al (2012) Quality of life and emotional distress in early stage and locally advanced cervical cancer patients: a prospective, longitudinal study. Gynecol Oncol 124:389–394
Jensen PT, Groenvold M, Klee MC, Thranov I, Petersen MA, Machin D (2003) Longitudinal study of sexual function and vaginal changes after radiotherapy for cervical cancer. Int J Radiat Oncol Biol Phys 56:937–949
Mirabeau-Beale KL, Viswanathan AN (2014) Quality of life (QOL) in women treated for gynecologic malignancies with radiation therapy: a literature review of patient-reported outcomes. Gynecol Oncol 134:403–409
Korfage IJ, Essink-Bot ML, Mols F, van de Poll-Franse L, Kruitwagen R, van Ballegooijen M (2009) Health-related quality of life in cervical cancer survivors: a population-based survey. Int J Radiat Oncol Biol Phys 73:1501–1509
Le Borgne G, Mercier M, Woronoff AS, Guizard AV, Abeilard E, Caravati-Jouvenceaux A et al (2013) Quality of life in long-term cervical cancer survivors: a population-based study. Gynecol Oncol 129:222–228
Acknowledgements
This study was supported by Chulabhorn Hospital.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
The study was approved by the Committee on Human Rights Related to Research Involving Human Subjects Chulabhorn Research Institute, number 20/2553. Written informed consent was obtained from all the patients.
Conflict of interest
The authors declare that they have no conflicts of interest.
Rights and permissions
About this article
Cite this article
Thanthong, S., Rojthamarat, S., Worasawate, W. et al. Comparison of efficacy of meperidine and fentanyl in terms of pain management and quality of life in patients with cervical cancer receiving intracavitary brachytherapy: a double-blind, randomized controlled trial. Support Care Cancer 25, 2531–2537 (2017). https://doi.org/10.1007/s00520-017-3662-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00520-017-3662-3