Abstract
Recent data indicate that there are large disparities in the use of opioid analgesics to control breakthrough cancer pain (BTcP) in Europe and worldwide. While it is clear that affordability is a key factor, it is certainly not the only one, and other factors, such as cultural differences and overall awareness, are undoubtedly responsible. More work remains to be done to overcome barriers in the use of these medications when warranted. When prescribing a medication for BTcP, it must be considered that its time profile is different from chronic persistent pain. The best control of background pain can best be achieved with a low dose of an extended opioid, and managing BTcP with a rapid-onset opioid, providing a good combination of overall pain control and lower opioid exposure. Notwithstanding their efficacy, greater attention needs to be paid to inappropriate use of opioids. It is important to evaluate patients for potential opioid misuse, including assessment of risk factors, and aberrant drug-taking behaviours must be investigated. In our institution, several measures have been adopted in this patient population in order to prevent aberrant opioid-induced behaviours. The adoption of some or all of these principles, depending on the individual patient and treatment setting, can undoubtedly help to reduce the risk of developing an aberrant behaviour related to opioid use as rescue medication for BTcP.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
One of the most widely accepted definitions of cancer-related breakthrough pain (BTcP) is that of the Association for Palliative Medicine of Great Britain and Ireland (APM), namely ‘a transient exacerbation of pain that occurs either spontaneously, or in relation to a specific predictable or unpredictable trigger, despite relatively stable and adequately controlled background painʼ [1]. With that definition in mind, and considering that opioid analgesics are commonly used to treat pain, including BTcP, it is worthwhile examining recent statistics on the use of opioid analgesics in Europe and elsewhere. This highlights disparities in use of opioid analgesics, especially in Europe, in managing patients with cancer pain. Moreover, the experience on choice of rapid-onset opioids (ROOs) at Hospital General Universitario Gregorio Marañón in Madrid, Spain, will then be discussed, followed by an examination of practical measures regarding opioid treatment of patients with cancer pain, including BTcP, while minimising the risk of addictive behaviours.
Disparities in use of opioid analgesics
Very recent data calculating the defined daily doses for statistical purposes (S-DDD) per million inhabitants per day of opioid analgesics have indicated that there are wide disparities worldwide [2]. From 2010 to 2013, substantial increases in use were seen in North America, western and central Europe and Oceania, while no such increases were evident in other areas. Even among European countries, the so-called ‘pain divide’ is readily obvious (Table 1). Opioid analgesic use is highest in Germany and lowest in Bulgaria. While it is also clear that affordability is a key issue, it is certainly not the only one that is responsible for such disproportions, and other factors, such as cultural differences and overall awareness, are undoubtedly at the basis. This can be inferred from the intermediate consumption of opioid analgesics in other European countries such as France, UK and Italy. Considering barriers to opioid medicines, a review of national legislation and regulations of 11 central and eastern European countries concluded that stricter control measures might result in the prevention of misuse and diversion, but that legitimate medical use of opioids might be restricted [3]. Moreover, it was found that national legislations and regulations contain many potential barriers, such as disrespectful language that contributes to stigmatisation, as well as previously identified barriers such as absence of prescriber training, fear of dependence and criminal prosecution, problems sourcing or importing opioids, increased costs and difficulty in implementing control measures. In addition, diverse cultural attitudes were also considered to be a major source to access to opioid medicines. Thus, it is clear that more work needs to be done to overcome such barriers.
Access to opioid analgesics for BTcP in Spain and characteristics of BTcP
In March 2014, the Pharmacy Committee of Hospital General Universitario Gregorio Marañón in Madrid, Spain, (HGUGM) requested a formal recommendation from our palliative care unit regarding which of the six then licensed ROOs should be available in the hospital formulary [4]. The request was made to rationalize ROOs use, in spite of the low consumption rates of ROOs in hospitals due to widespread availability of parenteral opioids, and also in order to reduce costs associated with stocking. Our unit was selected as we are a national reference centre for palliative care, and the decisions of the Pharmacy Committee of the HGUGM are regarded as widely influential in Spain.
BTcP has a time profile that is different from chronic persistent pain, and thus should be managed differently [5]. Indeed, as reported by Davies et al., the median time to peak intensity of BTcP is 10 min, even if the range is somewhat large (Fig. 1), with a median duration of 60 min (range < 1 to 360 min: Fig. 2) [6]. In the observational study of 1000 patients by Davies et al., the intensity of the BTcP was rated as ‘mildʼ in 36 cases, ‘moderateʼ in 337 cases and ‘severeʼ in 618 cases (with no specific information for nine patients) [6]. The median number of episodes of BTcP is 3 per day [7].
Time to peak intensity of untreated episodes of BTcP. Adapted with permission from [6]
Duration of untreated episodes of BTcP. Adapted with permission from [6]
Importantly, the pharmacological profile of oral morphine does not tend to mirror the temporal characteristics of most breakthrough pain episodes. Thus, the slow onset of action (analgesia: 20–30 min; peak analgesia: 60–90 min) results in delayed or ineffective analgesia, while the prolonged duration of effect (3–6 h) results in ongoing adverse effects (Fig. 3) [8]. In other words, oral morphine is not the optimal rescue medication for most breakthrough pain episodes, which have an average duration of 30 min. Moreover, these factors apply equally to the oral immediate-release formulations of similar opioid analgesics, e.g. oxycodone and hydromorphone.
Temporal relationship between breakthrough pain episodes and oral morphine treatment. Adapted from [8] with permission
Pain control with only an around-the-clock extended-release opioid medication will lead to a high level of opioid exposure and adverse neurological and gastrointestinal effects, and the profile of extended release opioid does not match that of BTcP [5] (Fig. 4). While using a lower dose of an extended-release opioid together with an immediate-release opioid would result in lower overall exposure compared to a high dose of an extended-release opioid, BTcP is still not well controlled because the characteristics of BTcP do not match that of an immediate-release opioid (i.e. onset of action about 30 min, duration of about 4 h) (Fig. 4). Thus, control of background pain with a low dose of an extended opioid and managing BTcP with a ROO provides a good combination of overall pain control and lower opioid exposure (by matching the temporal characteristics of BTcP) (Fig. 4). Indeed, rapid onset and short duration of action allow good control of analgesia, while the pharmacokinetic properties of ROOs may permit reduction of the total opioid burden and associated adverse effects. Moreover, the efficacy of ROOs has been most effectively demonstrated by a meta-analysis that concluded that it is superior to oral morphine, which in turn is superior to placebo in control of BTcP [9].
Time course of cancer pain (black line) with various treatment strategies. The grey shading indicates total opioid exposure. a ATC every 12 h ER opioid medication (thin grey line). b Lower dosage ATC ER opioid medication, with IR opioid medication for BTP. c Same dosage of ATC ER opioid as in panel b; BTP controlled with a ROO. ATC around the clock, BTP breakthrough pain, ER extended release, IR immediate release, ROO rapid-onset opioid. Adapted from [5] with permission
Thus, any decisions regarding the use a specific rescue medication, usually a ROO formulation, for treatment of BTcP should be based on a combination of four factors: (1) the characteristics of BTcP, including temporal characteristics like duration and time to peak intensity (median duration is 60 min and median time to peak intensity is 10 min [7]); (2) the drug’s characteristics, including pharmacokinetics, pharmacodynamics (short-acting opioids, such as immediate release oral morphine, are not the treatment of choice for BTcP because the onset of analgesia starts after 30–45 min with an analgesic duration of about 4 h, which does not match the temporal profile of BTcP episodes); (3) previous response to opioids (e.g. efficacy and tolerability); and (4) the patient’s preference for a specific route of administration (up to 65% of patients prefer an oral transmucosal route [7]) (Fig. 5). In this light, it is unlikely that any single ROO formulations will be suitable for all patients with BTcP.
Responses to questions about potential use of different routes of administration (‘would you consider using such a product?ʼ). Adapted from [7] with permission
Our final recommendation to the Pharmacy Committee in our institution to introduce ROOs in our hospital formulary was also supported by two recent pharmacoeconomic studies performed in Spain. In the first study, all ROOs were cost-effective in terms of willingness to pay per years gained with good quality of life [10]. In the second study, a 4-year model of the budget impact of ROOs was developed for the period 2012–2015 for patients with BTcP from the perspective of the public Spanish National Health System, which tightly regulates the cost of ROOs in the country [11]. The model determined the annual treatment costs of BTcP per patient associated with each fentanyl product to estimate the overall budget impact based on the total treatment population and the percentage of drug utilization associated with each product (buccal, sublingual or nasal transmucosal). The analysis found that although the economic impact of treatment of BTcP was expected to increase over 4 years due to population growth, the increased use of fentanyl buccal tablet decreased the average annual costs per patient by an average of €29 over 4 years. Thus, according to this model, an increase in use of an oral ROO would lead to significant overall savings in the budget impact for the Spanish National Health System.
It is important to emphasize that there are no specific restrictions in place in Spain in order to prescribe ROOs. Nevertheless, in our final report to our Pharmacy Committee, we suggested that the 2007 FDA safety warning should be followed when prescribing ROOs, namely:
-
Do not use in opioid-naïve patients
-
Do not use in acute pain
-
Do not convert patients on a microgram per microgram basis from one ROO to another—ROOs are not interchangeable and have very specific dosing strategies
-
Do not substitute one product for another when dispensing
-
Risk of misuse [12].
Addressing the problem of aberrant opioid-induced behaviour
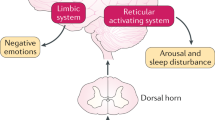
A recent publication has stressed that opioid therapy is effective for use in cancer pain, although there are due concerns about its inappropriate use [13]. In this regard, patients on opioid therapy should be evaluated for potential opioid misuse, including assessment of risk factors, and aberrant drug-taking behaviours must be investigated. Outcomes of cancer pain management should also be addressed using the ‘4As’ developed by Passik and Weinreb [14].
The 4As are as follows:
-
Analgesia
-
Activities of daily living
-
Adverse events
-
Aberrant opioid-induced behaviours (AB)
Thus in this light, adequate pain relief, psychosocial function, side effects and addiction-related outcomes are all important in managing pain. In order to properly address these aspects, it is crucial that physicians have precise definitions for the different terms used. These have been defined by several authors (Table 2) [13, 16, 17].
Concerning the incidence of aberrant behaviour with opioid use, a range of values have been reported in both cancer and non-cancer populations. An observational post-authorisation safety surveillance study in a cohort of 551 patients was conducted in UK from 2009 to 2011, with the overall aim to examine the use of a ROO in relation to safety as prescribed in primary care. The study reported that the frequency of AB observed during treatment was 8% [18]. Also, during a 12-week open-label extension period of a study involving 130 patients with non-cancer pain taking chronic opioid therapy, AB was identified in 18% of patients taking a ROO and in 20% of patients taking traditional short-acting oral opioid for BTP [16].
In patients being treated for BTcP in Spain, the proportion of patients with AB ranges from about 9–19%, with both ROOs and short-acting oral opioids being equally responsible [19, 20]. This highlights the need to take adequate measures to prevent opioid-induced AB when treating patients with cancer pain in our own clinical setting, and so, our team has been involved in research in this topic for some time now [21, 22].
Therefore, in our Palliative Care Unit (PCU), the following measures have been adopted in this patient population in order to prevent aberrant opioid-induced behaviors:
-
Increased awareness for early detection of risk factors:
-
prior addictive personality (drugs, alcohol, gambling etc.)
-
psychiatric illness
-
-
Selection of appropriate rescue drug for BTcP when risk factor detected:
-
Extended release formulations for basal cancer pain
-
Avoid rescue doses with opioids if at all possible
-
-
Monitor regularly
-
Recruit relatives to oversee patient at home
-
Do not prescribe ROOs off-license, e.g. for benign pain
Also in our PCU, the following measures are adopted once a patient is diagnosed with an aberrant opioid-induced behaviour:
-
Only one knowledgeable prescriber should be responsible for all opioids needed by the patient, while simultaneously coordinating the involvement of the rest of the multidisciplinary team
-
Adopt an empathic approach, avoiding stigmatisation
-
Verbal treatment agreement
-
Monitor closely; the patient will probably need follow-up until death or total opioid discontinuation
-
Ambulatory opioid rotation to buprenorphine TTS or/and inpatient opioid rotation to oral methadone [20]
Finally, our group has recently submitted for publication a clinical audit performed in our Early Palliative Care Outpatient Clinic that evaluated the quality of our management of aberrant opioid-induced behaviour. Our data support the emerging relevance of AB in chronic cancer pain and the BTcP population, and also seem to validate our standing protocol. Based on our clinical experience, it seems that good clinical practice performed by highly qualified professionals has been key to our success in controlling AB. In our experience, urine drug screens and screening questionnaires, as suggested in the literature, are not helpful. On the other hand, clinical expertise in the detection of AB and in performing complex opioid rotations to buprenorphine and/or methadone have been key to analgesic success and in controlling AB [23].
Conclusion
The unquestionable emergence of AB seems to be, up to a certain extent, a relatively unavoidable side effect of adequate medical opioid consumption for the relief of cancer pain. Our data support our conviction that the problem is manageable with good clinical practice. Therefore, we believe the answer to the problem is not to increase restrictions on cancer patients to access opioids (including ROOs) in order to avoid an expansion of AB, but to increase efforts to prevent these behaviours, and once detected to organize adequate specialized care.
References
Davies AN, Dickman A, Reid C, Stevens AM, Zeppetella G, Science Committee of the Association for Palliative Medicine of Great B et al (2009) The management of cancer-related breakthrough pain: recommendations of a task group of the science Committee of the Association for palliative medicine of great Britain and Ireland. Eur J Pain 13:331–338
Berterame S, Erthal J, Thomas J, Fellner S, Vosse B, Clare P et al (2016) Use of and barriers to access to opioid analgesics: a worldwide, regional, and national study. Lancet 387:1644–1656
Vranken MJ, Lisman JA, Mantel-Teeuwisse AK, Junger S, Scholten W, Radbruch L et al (2016) Barriers to access to opioid medicines: a review of national legislation and regulations of 11 central and eastern European countries. Lancet Oncol 17:e13–e22
Núñez Olarte JM (2014) Breakthrough cancer pain management in Spain. Meet the experts session. 8th World Research Congress of the European Association for Palliative Care (EAPC), Lleida (Spain), pp 5–7
Simon SM, Schwartzberg LS (2014) A review of rapid-onset opioids for breakthrough pain in patients with cancer. J Opioid Manag 10:207–215
Davies A, Buchanan A, Zeppetella G, Porta-Sales J, Likar R, Weismayr W et al (2013) Breakthrough cancer pain: an observational study of 1000 European oncology patients. J Pain Symptom Manag 46:619–628
Davies A, Zeppetella G, Andersen S, Damkier A, Vejlgaard T, Nauck F et al (2011) Multi-Centre European study of breakthrough cancer pain: pain characteristics and patient perceptions of current and potential management strategies. Eur J Pain 15:756–763
Davies AN (2011) The management of breakthrough cancer pain. Br J Nurs 20:803–804
Zeppetella G, Davies A, Eijgelshoven I, Jansen JP (2014) A network meta-analysis of the efficacy of opioid analgesics for the management of breakthrough cancer pain episodes. J Pain Symptom Manag 47:772–785 e775
Blanco B, García Ruiz AJ, García-Agua SN (2013) Resultados en salud y eficiencia del fentanilo intranasal en pectina en el dolor irruptivo en la práctica clínica habitual. Rev Soc Esp Dolor 20:221–229
Darba J, Kaskens L, Sánchez-de la Rosa R (2013) Budget impact analyisis of the fentanyl buccal tablet for treatment of breakthrough cancer pain. Clinicoecon Outcomes Res 6:1–9
Twycross R, Prommer EE, Mihalyo M, Wilcock A (2012) Fentanyl (transmucosal). J Pain Symptom Manag 44:131–149
Pergolizzi JV, Zampogna G, Taylor R, Gonima E, Posada J, Raffa RB (2016) A guide for pain Management in Low and Middle Income Communities. Managing the risk of opioid abuse in patients with cancer pain. Front Pharmacol 7:42
Passik SD, Weinreb HJ (2000) Managing chronic nonmalignant pain: overcoming obstacles to the use of opioids. Adv Ther 17:70–83
Passik SD, Messina J, Golsorkhi A, Xie F (2011) Aberrant drug-related behavior observed during clinical studies involving patients taking chronic opioid therapy for persistent pain and fentanyl buccal tablet for breakthrough pain. J Pain Symptom Manag 41:116–125
Passik SD, Narayana A, Yang R (2014) Aberrant drug-related behavior observed during a 12-week open-label extension period of a study involving patients taking chronic opioid therapy for persistent pain and fentanyl buccal tablet or traditional short-acting opioid for breakthrough pain. Pain Med 15:1365–1372
Wu SM, Compton P, Bolus R, Schieffer B, Pham Q, Baria A et al (2006) The addiction behaviors checklist: validation of a new clinician-based measure of inappropriate opioid use in chronic pain. J Pain Symptom Manag 32:342–351
Layton D, Osborne V, Al-Shukri M, Shakir SA (2014) Indicators of drug-seeking aberrant behaviours: the feasibility of use in observational post-marketing cohort studies for risk management. Drug Saf 37:639–650
Martin ZM (2016) Registro del abuso/mal uso de opioides: experiencia de un centro. Symposium TEVA. XI Congreso Internacional de Cuidados Paliativos de la Sociedad Española de Cuidados Paliativos (SECPAL), Sevilla, Spain, pp 12–14
Núñez Olarte JM (2016) Abordaje práctico del paciente con abuso/mal uso de opioides de acción rápida. Symposium TEVA. XI Congreso Internacional de Cuidados Paliativos de la Sociedad Española de Cuidados Paliativos (SECPAL), Sevilla, Spain, pp 12–14
Nunez-Olarte JM, Alvarez-Jimenez P (2011) Emerging opioid abuse in terminal cancer patients taking oral transmucosal fentanyl citrate for breakthrough pain. J Pain Symptom Manag 42:e6–e8
Álvarez Jiménez P, Quiñones Pérez A, Núñez Olarte JM (2013) onductas aberrantes asociadas al empleo de fentanilos rápidos en pacientes oncológicos terminales: a propósito de un caso. Medicina Paliativa 20:26–31
Núñez Olarte JM, Francisco López MC. Management of aberrant opioid-induced behaviour in an "early palliative care" outpatient clinic. Medicina Palliativa 2016
Acknowledgements
None.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Funding
None.
Conflict of interest
The author has received monetary support from Angelini (research grant), Archimedes (educational activities), Ferrer (scientific board, educational activities), Mundipharma (educational activities), Prostrakan (educational activities), Takeda (scientific board, educational activities) and Teva (research grant, educational activities).
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution-NonCommercial 4.0 International License (http://creativecommons.org/licenses/by-nc/4.0/), which permits any noncommercial use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made.
About this article
Cite this article
Olarte, J.M.N. Breakthrough cancer pain and rational drug use. Support Care Cancer 25 (Suppl 1), 11–17 (2017). https://doi.org/10.1007/s00520-017-3636-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00520-017-3636-5