Abstract
Purpose
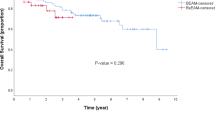
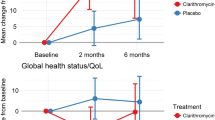
High-dose chemotherapy prior to autologous stem cell transplantation (ASCT) leads to adverse effects including mucositis, neutropenia and bacteremia. To reduce the toxicity, we treated myeloma and lymphoma patients with peroral bismuth as an adjuvant to chemotherapy to convey cytoprotection in non-malignant cells.
Methods
This trial was a prospective, randomised, double-blind, placebo-controlled pilot study of hematological inpatients (n = 50) receiving bismuth or placebo tablets, in order to identify any potential superiority of bismuth on toxicity from chemotherapy.
Results
We show for the first time that bismuth significantly reduces grade 2 stomatitis, febrile neutropenia and infections caused by melphalan in multiple myeloma, where adverse effects also were significantly linked to gender. In lymphoma patients, bismuth significantly reduces diarrhoea relative to placebo. Also, lymphoma patients’ adverse effects were linked to gender. For the first time, bismuth is demonstrated as a safe strategy against chemotherapy’s toxicity without interfering with intentional anti-cancer efficiency. Also, we show how gender significantly influences various adverse effects and response to treatment in both multiple myeloma and malignant lymphomas.
Conclusion
These results may impact clinical prevention of chemotherapy’s cytotoxicity in certain patient groups, and also, this study may direct further attention towards the impact of gender during the course and treatment outcome of malignant disorders.





Similar content being viewed by others
Change history
06 October 2020
This article has been retracted. Please see the retraction notice for more detail: https://doi.org/10.1007/s00520-020-05770-w.
References
Attal M, Harousseau JL, Stoppa AM et al (1996) A prospective, randomized trial of autologous bone marrow transplantation and chemotherapy in multiple myeloma. Intergroupe Français du Myélome. N Engl J Med 335:91–97
Child JA, Morgan GJ, Davies FE et al (2003) High-dose chemotherapy with hematopoietic stem-cell rescue for multiple myeloma. N Engl J Med 348:1875–1883
Fernandes LL, Torres SR, Garnica M et al (2014) Oral status of patients submitted to autologous hematopoietic stem cell transplantation. Support Care Cancer 22:15–21
Wardill HR, Bowen JM, Gibson RJ (2014) New pharmacotherapy options for chemotherapy-induced alimentary mucositis. Expert Opin Biol Ther 14:347–354
Waśko-Grabowska A, Rzepecki P, Oborska S et al (2011) Efficiency of supersaturated calcium phosphate mouth rinse treatment in patients receiving high-dose melphalan or BEAM prior to autologous blood stem cell transplantation: a single-center experience. Transplant Proc 43:3111–3113
Spielberger R, Stiff P, Bensinger W et al (2004) Palifermin for oral mucositis after intensive therapy for hematologic cancers. N Engl J Med 351:2590–2598
Herbers AH, van der Velden WJ, de Haan AF et al (2014) Impact of palifermin on intestinal mucositis of HSCT recipients after BEAM. Bone Marrow Transplant 49:8–10
Blijlevens N, de Château M, Krivan G et al (2013) In a high-dose melphalan setting, palifermin compared with placebo had no effect on oral mucositis or related patient’s burden. Bone Marrow Transplant 48:966–971
Briand GG, Burford N (1999) Bismuth compounds and preparations with biological or medicinal relevance. Chem Rev 99:2601–2658
Xia W, Li H, Sun H (2014) Functional disruption of HypB, a GTPase of Helicobacter pylori, by bismuth. Chem Commun (Camb) 50:1611–1614
Song M, Ang TL (2014) Second and third line treatment options for Helicobacter pylori eradication. World J Gastroenterol 20:1517–1528
Imura N, Naganuma A, Satoh M, Koyama Y (1987) Induction of renal metallothionein allows increasing dose of an extensively used antitumor drug, cis-diamminedichloroplatinum. Experientia Suppl 52:655–660
Morikawa T, Kawamura E, Komiyama T, Imura N (1990) Alleviation of cisplatin toxicity by high-dose bismuth subnitrate and pharmacokinetics of bismuth subnitrate and cisplatin. Nippon Gan Chiryo Gakkai Shi 25:1138–1145
Morikawa T, Kawamura E (1989) A method of cisplatin administration with the aid of high-dose bismuth subnitrate, and their pharmacokinetics. Gan To Kagaku Ryoho 16:1094–1098
Naganuma A, Satoh M, Imura N (1988) Specific reduction of toxic side effects of adriamycin by induction of metallothionein in mice. Jpn J Cancer Res 79:406–411
Kondo Y, Satoh M, Imura N, Akimoto M (1992) Tissue-specific induction of metallothionein by bismuth as a promising protocol for chemotherapy with repeated administration of cis-diamminedichloroplatinum (II) against bladder tumor. Anticancer Res 12:2303–2307
Kondo Y, Satoh M, Imura N, Akimoto M (1991) Effect of bismuth nitrate given in combination with cis-diamminedichloroplatinum(II) on the antitumor activity and renal toxicity of the latter in nude mice inoculated with human bladder tumor. Cancer Chemother Pharmacol 29:19–23
Satoh M, Kondo Y, Mita M et al (1993) Prevention of carcinogenicity of anticancer drugs by metallothionein induction. Cancer Res 53:4767–4768
Kondo Y, Rusnak JM, Hoyt DG et al (1997) Enhanced apoptosis in metallothionein null cells. Mol Pharmacol 52:195–201
Pedersen MØ, Larsen A, Stoltenberg M, Penkowa M (2009) The role of metallothioneinin oncogenesis and cancer prognosis. Prog Histochem Cytochem 44:29–64
Raudenska M, Gumulec J, Podlaha O et al (2014) Metallothionein polymorphisms in pathological processes. Metallomics 6:55–68
Ruttkay-Nedecky B, Nejdl L, Gumulec J et al (2013) The role of metallothionein in oxidative stress. Int J Mol Sci 14:6044–6066
Naganuma A, Imura N (1994) Role of metallothionein in cancer chemotherapy. Gan To Kagaku Ryoho 21:301–306
Satoh M, Naganuma A, Imura N (2000) Modulation of adriamycin toxicity by tissue-specific induction of metallothionein synthesis in mice. Life Sci 67:627–634
Finch PW, Rubin JS (2006) Keratinocyte growth factor expression and activity in cancer: implications for use in patients with solid tumors. J Natl Cancer Inst 98:812–824
Finch PW, Mark Cross LJ, McAuley DF, Farrell CL (2013) Palifermin for the protection and regeneration of epithelial tissues following injury: new findings in basic research and pre-clinical models. J Cell Mol Med 17:1065–1087
Ishino R, Minami K, Tanaka S et al (2013) FGF7 supports hematopoietic stem and progenitor cells and niche-dependent myeloblastoma cells via autocrine action on bone marrow stromal cells in vitro. Biochem Biophys Res Commun 440:125–131
Vokurka S, Bystricka E, Koza V et al (2005) The comparative effects of povidone–iodine and normal saline mouthwashes on oral mucositis in patients after high-dose chemotherapy and APBSCT—results of a randomized multicentre study. Support Care Cancer 13:554–558
Vokurka S, Bystrická E, Koza V et al (2006) Higher incidence of chemotherapy induced oral mucositis in females: a supplement of multivariate analysis to a randomized multicentre study. Support Care Cancer 14:974–976
Sakellari I, Angelopoulou M, Tsopra O et al (2015) A prospective study of incidence, clinical and quality of life consequences of oral mucositis post palifermin prophylaxis in patients undergoing high-dose chemotherapy and autologous hematopoietic cell transplantation. Ann Hematol 94:1733–1740
Pfreundschuh M, Müller C, Zeynalova S et al (2014) Suboptimal dosing of rituximab in male and female patients with DLBCL. Blood 123:640–646
Acknowledgements
We wish to acknowledge the clinical research unit and the nurses of the Department of Hematology for their assistance.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
The study was approved by relevant boards including the ethics committee and the Danish National Board of Health. This study is registered with EudraCT number 2007-007652-34.
Conflict of interest
The authors declare that they have no conflict of interest.
Funding
The study was funded by means of our institutions at the time of investigation (the Department of Hematology and the University of Copenhagen) and by grants from Herlev Hospital (PBH), Lægeforeningens Forskningsfond (MP) and Mimi og Viktor Larsens Fond (MP).
About this article
Cite this article
Hansen, P.B., Penkowa, M. RETRACTED ARTICLE: Bismuth adjuvant ameliorates adverse effects of high-dose chemotherapy in patients with multiple myeloma and malignant lymphoma undergoing autologous stem cell transplantation: a randomised, double-blind, prospective pilot study. Support Care Cancer 25, 1279–1289 (2017). https://doi.org/10.1007/s00520-016-3522-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00520-016-3522-6