Abstract
Purpose
Informal caregivers (ICs) provide care and improve the quality of life of patients with malignant brain tumor. We analyze the impact of their involvement on themselves from a triple perspective.
Methods
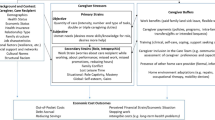
Home-dwelling patients with primary malignant brain tumor underwent a medical examination. ICs burden was evaluated by a self-administered postal questionnaire. Objective burden (Informal Care Time, ICT), subjective burden (Zarit Burden Inventory, ZBI), and financial burden (valuation of lost earnings using the Replacement and Opportunity Cost Methods, RCM, OCM) were evaluated.
Results
ICs (N = 84) were principally women (87 %) and spouses (64 %), of mean age 55 years, who assisted patients of mean age 53 years and with a mean KPS score of 61 (range = 30–90, med = 60). Subjective burden was moderate (mean ZBI = 30). Objective burden was high (mean ICT = 11.7 h/day), mostly consisting of supervision time. Higher subjective and objective burden were associated with poorer functional status (KPS) but not with a higher level of cognitive disorders in multivariate analyses. Other independent associated factors were bladder dysfunction and co-residency for objective burden and working and a poor social network for subjective burden. The 56 working ICs made work arrangements (75 %) that impacted their wages (36 %) and careers (30 %). Financial burden due to uncompensated caregiving hours for Activities of Daily Living had a mean monetary value from Є677(RCM) to Є1683(OCM) per month (i.e., ranging from Є8124 to Є20196 per year).
Conclusions
IC burden is multidimensional. Greater provision of formal care, more IC support programs, and economic interventions targeting IC employment and finances are needed.


Similar content being viewed by others
References
Louis DN, Ohgaki H, Wiestler OD, et al. (2007) The 2007 WHO classification of tumours of the central nervous system. Acta Neuropathol 114:97–109
Institut National de la Statistique et des Etudes Economiques. Enquête Handicap Santé-Aidants Informels (HS-HSA-HSM) (2008) http://www.insee.fr/fr/methodes/default.asp?page =sources/ope-enq-handicap-sante-menages-hsm.htm
Lageman SK, Brown PD, Anderson SK, et al. (2015) Exploring primary brain tumor patient and caregiver needs and preferences in brief educational and support opportunities. Support Care Cancer 23(3):851
Sherwood PR, Cwiklik M, Donovan HS (2016) Neuro-oncology family caregiving: review and directions for future research. CNS Oncol 5:41–48
Whisenant M (2011) Informal caregiving in patients with brain tumors. Oncol Nurs Forum 38:E373–E381
Sherwood PR, Given BA, Given CW, et al. (2006) Predictors of distress in caregivers of persons with a primary malignant brain tumor. Res Nurs Health 29:105–120
Keir ST, Guill AB, Carter KE, Friedman HS (2006) Stress and intervention preferences of patients with brain tumors. Support Care Cancer 14:1213–1219
Madsen K, Poulsen HS (2010) Needs for everyday life support for brain tumour patients’ relatives: systematic literature review. Eur J Cancer Care (Engl) 20:33–43
Sherwood PR, Donovan HS, Given CW, et al. (2008) Predictors of employment and lost hours from work in cancer caregivers. Psychooncology 17:598–605
Ford E, Catt S, Chalmers A, Fallowfield L (2012) Systematic review of supportive care needs in patients with primary malignant brain tumors. Neuro-Oncology 14:392–404
Deeken JF, Taylor KL, Mangan P, Yabroff KR, Ingham JM (2003) Care for the caregivers: a review of self-report instruments developed to measure the burden, needs, and quality of life of informal caregivers. J Pain Symptom Manag 26:922–953
Harvey K, Catty J, Langman A, et al. (2008) A review of instruments developed to measure outcomes for carers of people with mental health problems. Acta Psychiatr Scand 117:164–176
Kinsella G, Cooper B, Picton C, Murtagh D (1998) A review of the measurement of caregiver and family burden in palliative care. J Palliat Care 14:37–45
Sterckx W, Coolbrandt A, Clement P, et al. (2015) Living with a high-grade glioma: a qualitative study of patients’ experiences and care needs. Eur J Oncol Nurs 19:383–390
Moore G, Collins A, Brand C, et al. (2013) Palliative and supportive care needs of patients with high-grade glioma and their carers: a systematic review of qualitative literature. Patient Educ Couns 91:141–153
Heese O, Vogeler E, Martens T, et al. (2013) End-of-life caregivers’ perception of medical and psychological support during the final weeks of glioma patients: a questionnaire-based survey. Neuro-Oncology 15:1251–1256
Finocchiaro CY, Petruzzi A, Lamperti E, et al. (2012) The burden of brain tumor: a single-institution study on psychological patterns in caregivers. J Neuro-Oncol 107:175–181
Janda M, Steginga S, Langbecker D, Dunn J, Walker D, Eakin E (2007) Quality of life among patients with a brain tumor and their carers. J Psychosom Res 63:617–623
Halkett GK, Lobb EA, Oldham L, Nowak AK (2010) The information and support needs of patients diagnosed with high grade glioma. Patient Educ Couns 79:112–119
Janda M, Eakin EG, Bailey L, Walker D, Troy K (2006) Supportive care needs of people with brain tumours and their carers. Support Care Cancer 14:1094–1103
Parvataneni R, Polley MY, Freeman T, et al. (2011) Identifying the needs of brain tumor patients and their caregivers. J Neuro-Oncol 104:737–744
Schubart JR, Kinzie MB, Farace E (2008) Caring for the brain tumor patient: family caregiver burden and unmet needs. Neuro-Oncology 10:61–72
Zarit SH, Todd PA, Zarit JM (1986) Subjective burden of husbands and wives as caregivers: a longitudinal study. Gerontologist 26:260–266
Braithwaite V (1992) Caregiving burden: making the concept scientifically useful and policy relevant. Res Aging 14:3–27
Koopmanschap M, Van Exel J, Van den Berg B, Brouwer W (2008) An overview of methods and application to value informal Care in Economic Evaluations of healthcare. PharmacoEconomics 26:269–280
Brouwer WB, van Exel NJ, Koopmanschap MA, Rutten FF (1999) The valuation of informal care in economic appraisal. A consideration of individual choice and societal costs of time. Int J Technol Assess Health Care 15:147–160
Vecchio N, Cybinski P, Stevens S (2008) The effect of disability on the needs of caregivers. Int J of Social Economics. 782.
Schag CC, Heinrich RL, Ganz PA (1984) Karnofsky performance status revisited: reliability, validity, and guidelines. J Clin Oncol 2:187–193
Mahoney FI, Barthel DW (1965) Functional evaluation: the Barthel index. Md State Med J 14:61–65
Vanier M, Mazaux JM, Lambert J, Dassa C, Levin HS (2000) Assessment of neuropsychologic impairments after head injury: interrater reliability and factorial and criterion validity of the neurobehavioral rating scale-revised. Arch Phys Med Rehabil 81:796–806
Ware J Jr, Kosinski M, Keller SD (1996) A 12-item short-form health survey: construction of scales and preliminary tests of reliability and validity. Med Care 34:220–233
Dalgard OS (2009) Social support - Occurrence. In: EUPHIX E, ed. EUPHIX, EUphact Bilthoven: RIVM, <http://wwweuphixorg > EUphact\ Determinants of health\ Environment\ Social support
Zarit SH, Reever KE, Bach-Peterson J (1980) Relatives of the impaired elderly: correlates of feelings of burden. Gerontologist 20:649–655
Rankin ED, Haut MW, Keefover RW, Franzen MD (1994) The establishment of clinical cutoffs in measuring caregiver burden in dementia. Gerontologist 34:828–832
Wimo A, Winblad B (2003) Ressource utilization in dementia: RUD lite. Brain Aging 3:47–58
Décret relatif à la prestation de compensation à domicile pour les personnes handicapées (2005) Décret n° 2005–1591 du 19 décembre 2005 relatif à la prestation de compensation à domicile pour les personnes handicapées. Journal Officiel de la République Française.
McDaid D (2001) Estimating the costs of informal care for people with Alzheimer’s disease: methological and practical challenges. Int J Geriatr Psychiatry 16:400–405
Décret n (2013)° 2013–1190 du 19 décembre 2013 portant relèvement du salaire minimum de croissance Journal Officiel de la République Française du 20 décembre 2013 ;0295(Texte n°43):20809.
Ananian S, Demailly D, Pons Y (2014) Allègements et autres dispositifs dérogatoires portant sur les cotisations sociales patronales: une analyse empirique dans les entreprises de 10 salariés ou plus du secteur privé en 2010. Document d’études DARES. n°186.
Keir ST, Guill AB, Carter KE, Boole LC, Gonzales L, Friedman HS (2006) Differential levels of stress in caregivers of brain tumor patients-observations from a pilot study. Support Care Cancer 14:1258–1261
Adelbratt S, Strang P (2000) Death anxiety in brain tumour patients and their spouses. Palliat Med 14:499–507
Janda M, Steginga S, Dunn J, Langbecker D, Walker D, Eakin E (2008) Unmet supportive care needs and interest in services among patients with a brain tumour and their carers. Patient Educ Couns 71:251–258
Jackson D, Turner-Stokes L, Murray J, Leese M, McPherson KM (2009) Acquired brain injury and dementia: a comparison of carer experiences. Brain Inj 23:433–444
Li C, Zeliadt SB, Hall IJ, et al. (2013) Burden among partner caregivers of patients diagnosed with localized prostate cancer within 1 year after diagnosis: an economic perspective. Support Care Cancer 21:3461–3469
Ll Wood R, Alderman N, Williams C (2008) Assessment of neurobehavioural disability: a review of existing measures and recommendations for a comprehensive assessment tool. Brain Inj 22:905–918
Peters KB, West MJ, Hornsby WE, et al. (2014) Impact of health-related quality of life and fatigue on survival of recurrent high-grade glioma patients. J Neuro-Oncol 120:499–506
Blondel F, Delzescaux S, Fermon B (2009) Mesure de la qualité et qualité de la mesure de l’aide au domicile - Construction des points de vue sur la qualité de l’aide à domicile. Rapport post Appel à projet MIRe-DREES-CNSA
Sherwood PR, Given BA, Doorenbos AZ, Given CW (2004) Forgotten voices: lessons from bereaved caregivers of persons with a brain tumour. Int J Palliat Nurs 10:67–75 discussion 75
Newberry A, Kuo J, Donovan H, et al. (2012) Identifying family members who are likely to perceive benefits from providing care to a person with a primary malignant brain tumor. Oncol Nurs Forum 39:E226–E232
Sizoo EM, Braam L, Postma TJ, et al. (2010) Symptoms and problems in the end-of-life phase of high-grade glioma patients. Neuro-Oncology 12:1162–1166
Bayen E, Jourdan C, Ghout I, et al. (2014) Objective and subjective burden of informal caregivers 4 years after a severe traumatic brain injury: results from the PariS-TBI study. J Head Trauma Rehabil
Bayen E, Papeix C, Pradat-Diehl P, Lubetzki C, Joël ME (2015) Patterns of objective and subjective burden of informal caregivers of patients with multiple sclerosis Behav Neurol. May 20. 2015
Gustavsson A, Svensson M, Jacobi F, et al. (2011) Cost of disorders of the brain in Europe 2010. Eur Neuropsychopharmacol 21:718–779
Bradley SE, Sherwood PR, Kuo J, et al. (2009) Perceptions of economic hardship and emotional health in a pilot sample of family caregivers. J Neuro-Oncol 93:333–342
NICE (2006) Improving outcome for people with brain and other CNS tumours. London: National Institute of Health and Clinical Excellence. http://www.nice.org.uk/csgbraincns.
Cashman R, Bernstein LJ, Bilodeau D, et al. (2007) Evaluation of an educational program for the caregivers of persons diagnosed with a malignant glioma. Can Oncol Nurs J 17:6–15
Boele FW, Hoeben W, Hilverda K, et al. (2013) Enhancing quality of life and mastery of informal caregivers of high-grade glioma patients: a randomized controlled trial. J Neuro-Oncol 111:303–311
Acknowledgments
The authors thank the Association pour la Recherche sur les Tumeurs Cérébrales (ARTC) and Bérengère Davin for their support during the study. The first author received research grants from the French Society of Physical Medicine and Rehabilitation (SOFMER, 2012), the Fondation des “Gueules Cassées” (2012), the Caisse Nationale de Solidarité pour l’Autonomie (CNSA, 2013), and the Fondation de France (2014) for the project “Informal care and Neurodisability.” These funding sources were not involved in the study design, the collection, analysis, or interpretation of data, or in the writing of the article.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
All procedures performed in the present study involving human participants were in accordance with the ethical standards of the national research committee and with the 1964 Helsinki declaration and its later amendments.
Conflict of interest
The authors declare that there is no conflict of interest.
Rights and permissions
About this article
Cite this article
Bayen, E., Laigle-Donadey, F., Prouté, M. et al. The multidimensional burden of informal caregivers in primary malignant brain tumor. Support Care Cancer 25, 245–253 (2017). https://doi.org/10.1007/s00520-016-3397-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00520-016-3397-6