Abstract
Purpose
Insomnia is highly prevalent in cancer patients. Efficacious treatments exist for this condition but, for these interventions to be offered, an effective screening needs to be carried out beforehand. The pan-Canadian practice guidelines on sleep disturbances provide recommendations on how to use the Edmonton Symptom Assessment System (ESAS) and the Canadian Problem Checklist (CPC) to screen for sleep difficulties in cancer. However, empirical evidence to support these recommendations is lacking. The goal of this study was to assess the capacity of the ESAS (drowsiness and “other” items) and the CPC (sleep item) to screen for clinical insomnia in cancer patients.
Methods
As part of routine care, 615 patients with various cancer types completed the ESAS, the CPC, and the Insomnia Severity Index, used as the standard for establishing the presence of clinical insomnia.
Results
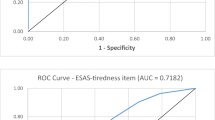
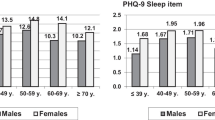
None of the criteria provided an effective screening when used alone. No patient used the ESAS-other item to report sleep difficulties. The sensitivity and specificity rates of the CPC-sleep item alone were 60.4 and 89.6 %, respectively. A score ≥2 on the ESAS-drowsiness item had a sensitivity of 61.5 % and a specificity of 75.4 %. When used in combination, the best option was scoring positively on the CPC-sleep item OR a score ≥2 on the ESAS-drowsiness item (sensitivity 84.2 %; specificity 69.7 %).
Conclusions
When used alone, the CPC-sleep and the ESAS-drowsiness items yielded insufficient sensitivity rates for a first screening, but when used in combination, they provided a good balance between sensitivity and specificity.
Similar content being viewed by others
References
Palesh OG, Roscoe JA, Mustian KM, Roth T, Savard J, Ancoli-Israel S, Heckler C, Purnell JQ, Janelsins MC, Morrow GR (2010) Prevalence, demographics, and psychological associations of sleep disruption in patients with cancer: University of Rochester cancer center-community clinical oncology program. J Clin Oncol 28:292–298
Savard J, Ivers H, Villa J, Caplette-Gingras A, Morin CM (2011) Natural course of insomnia comorbid with cancer: an 18-month longitudinal study. J Clin Oncol 29:3580–3586
Savard J, Villa J, Ivers H, Simard S, Morin CM (2009) Prevalence, natural course, and risk factors of insomnia comorbid with cancer over a 2-month period. J Clin Oncol 27:5233–5239
Ruel S, Savard J, Ivers H (2016) Insomnia, self-reported infections and infection-related consequences in cancer patients: an 18-month longitudinal study. Health Psychol
Daley M, Morin CM, LeBlanc M, Grégoire J-P, Savard J, Baillargeon L (2009) Insomnia and its relationship to health-care utilization, work absenteeism, productivity and accidents. Sleep Med 10:427–438
Fortier-Brochu É, Beaulieu-Bonneau S, Ivers H, Morin CM (2012) Insomnia and daytime cognitive performance: a meta-analysis. Sleep Med Rev 16:83–94
Chevalier H, Los F, Boichut D, Bianchi M, Nutt DJ, Hajak G, Hetta J, Hoffmann G, Crowe C (1999) Evaluation of severe insomnia in the general population: results of a European multinational survey. J Psychopharmacol (Oxf) 13:S21–S24
Léger D, Guilleminault C, Bader G, Levy E, Paillard M (2002) Medical and socio-professional impact of insomnia. Sleep 25:625–629
Neckelmann D, Mykletun A, Dahl AA (2007) Chronic insomnia as a risk factor for developing anxiety and depression. Sleep 30:873–880
Morphy H, Dunn KM, Lewis M, Boardman HF, Croft PR (2007) Epidemiology of insomnia: a longitudinal study in a UK population. Sleep 30:274–280
Jansson-Fröjmark M, Lindblom K (2008) A bidirectional relationship between anxiety and depression, and insomnia? A prospective study on the general population. J Psychosom Res 64:443–449
Sivertsen B, Lallukka T, Salo P, Pallesen S, Hysing M, Krokstad S, Simon O (2014) Insomnia as a risk factor for ill health: results from the large population-based prospective HUNT Study in Norway. J Sleep Res 23:124–132
Cohen S, Doyle WJ, Alper CM, Janicki-Deverts D, Turner RB (2009) Sleep habits and susceptibility to the common cold. Arch Intern Med 169:62–67
Davidson JR, Feldman-Stewart D, Brennenstuhl S, Ram S (2007) How to provide insomnia interventions to people with cancer: insights from patients. Psychooncology 16:1028–1038
Savard J, Savard MH (2013) Insomnia and cancer: prevalence, nature, and nonpharmacologic treatment. Sleep Med Clin 8:373–387
Blais MC, St-Hilaire A, Fillion L, De Serres M, Tremblay A (2014) What to do with screening for distress scores? Integrating descriptive data into clinical practice. Palliat Support Care 12:25–38
Jacobsen PB, Donovan KA, Trask PC, Fleishman SB, Zabora J, Baker F, Holland JC (2005) Screening for psychologic distress in ambulatory cancer patients. Cancer 103:1494–1502
Roth AJ, Kornblith AB, Batel-Copel L, Peabody E, Scher HI, Holland JC (1998) Rapid screening for psychologic distress in men with prostate carcinoma: a pilot study. Cancer 82:1904–1908
Bruera E, Kuehn N, Miller MJ, Selmser P, Macmillan K (1991) The Edmonton Symptom Assessment System (ESAS): a simple method for the assessment of palliative care patients. J Palliat Care 7:6–9
Ashbury FD, Findlay H, Reynolds B, McKerracher K (1998) A Canadian survey of cancer patients’ experiences: are their needs being met? J Pain Symptom Manag 16:298–306
Fitch MI, Porter HB, Page BD (2008) Supportive care framework: a foundation for person-centered care Pappin communications Pembroke, ON
Howell D, Oliver TK, Keller-Olaman S, Davidson J, Garland S, Samuels C, Savard J, Harris C, Aubin M, Olson K, Sussman J, Macfarlane J, Taylor C (2012) A pan-Canadian practice guideline: prevention, screening, assessment, and treatment of sleep disturbances in adults with cancer. Support Care Cancer
Chang VT, Hwang SS, Feuerman M (2000) Validation of the Edmonton symptom assessment scale. Cancer 88:2164–2171
Feldstain A, Tomei C, Belanger M, Lebel S (2014) Screening for distress in patients with cancer: methodologic considerations. Curr Oncol 21:e330–e333
Nekolaichuk C, Watanabe S, Beaumont C (2008) The Edmonton symptom assessment system: a 15-year retrospective review of validation studies (1991--2006). Palliat Med 22:111–122
Bastien CH, Vallières A, Morin CM (2001) Validation of the insomnia severity index as an outcome measure for insomnia research. Sleep Med 2:297–307
Blais FC, Gendron L, Mimeault V, Morin CM (1997) Évaluation de l’insomnie: validation de trois questionnaires. L’Encéphale 23:447–453
Savard MH, Savard J, Simard S, Ivers H (2005) Empirical validation of the insomnia severity index in cancer patients. Psychooncology 14:429–441
Rosenberg RP (2015) Recommended treatment strategies for patients with excessive daytime sleepiness. J Clin Psychiatry 76:e1330
Hannon B, Dyck M, Pope A, Swami N, Banerjee S, Mak E, Bryson J, Rodin G, Ridley J, Lo C, Le LW, Zimmermann C (2015) Modified Edmonton symptom assessment system including constipation and sleep: validation in outpatients with cancer. J Pain Symptom Manag 49:945–952
Kwon JH, Nam SH, Koh S, Hong YS, Lee KH, Shin SW, Hui D, Park KW, Yoon SY, Won JY, Chisholm G, Bruera E (2013) Validation of the Edmonton symptom assessment system in Korean patients with cancer. J Pain Symptom Manag 46:947–956
Delgado-Guay M, Yennurajalingam S, Parsons H, Palmer JL, Bruera E (2011) Association between self-reported sleep disturbance and other symptoms in patients with advanced cancer. J Pain Symptom Manag 41:819–827
American Psychiatric Association (2013) Diagnostic and statistical manual of mental disorders. American Psychiatric Publishing, Arlington
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no competing interests.
Rights and permissions
About this article
Cite this article
Savard, J., Ivers, H. & Savard, MH. Capacity of the Edmonton Symptom Assessment System and the Canadian Problem Checklist to screen clinical insomnia in cancer patients. Support Care Cancer 24, 4339–4344 (2016). https://doi.org/10.1007/s00520-016-3273-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00520-016-3273-4