Abstract
Purpose
Bevacizumab may potentiate the risk of venous thromboembolisms (VTEs) in cancer patients, who are already predisposed to pro-thrombotic states. We aimed to characterize the incidence of VTEs in a population-based cohort of metastatic colorectal cancer (mCRC) patients treated with bevacizumab, describe patient and treatment factors associated with VTEs, and examine how VTEs are managed.
Methods
Patients diagnosed with mCRC from 2006 to 2009 and offered bevacizumab were included. Descriptive statistics were used to describe VTE occurrences and management. Univariate and multivariate regression models were constructed to explore associations between clinical factors and VTEs.
Results
We identified 541 mCRC patients: 27 never started bevacizumab and 15 were lost to follow-up. Of the 499 evaluable patients, median age was 61, 59.3 % were men, 88.1 % had ECOG 0/1, and 5.2 % reported previous VTEs. Mean number of bevacizumab doses was 13.3 cycles. After receiving bevacizumab, 81 patients developed 93 cases of VTEs, with 9 patients experiencing >1 event. Individuals who experienced VTEs were more likely to have had pre-existing cardiovascular disease (OR 2.259, p = 0.0245), resection of primary cancer (OR 3.262, p = 0.0269), pre-chemotherapy platelet count ≥350,000/μL (OR 2.295, p = 0.0293), and received >12 bevacizumab cycles (OR 2.172, p = 0.0158). Use of bevacizumab varied after occurrence of VTE where it was discontinued in 34.4 %, continued in 34.4 %, and temporarily held in 1.1 %.
Conclusions
VTE risk can be high, especially in patients with specific pre-treatment risk factors as well as in those who received more bevacizumab, suggesting a potential dose-related effect. Management of bevacizumab-related VTEs was variable.
Similar content being viewed by others
References
Canadian Cancer Society’s Advisory Committee on Cancer Statistics (2013) Canadian Cancer Statistics 2013. http://www.cancer.ca/~/media/cancer.ca/CW/cancer%20information/cancer%20101/Canadian%20cancer%20statistics/canadian-cancer-statistics-2013-EN.pdf. Accessed 10 Sept 2013
National Cancer Institute (2011) SEER Stat Fact Sheets: Colon and Rectum Cancer. http://seer.cancer.gov/statfacts/html/colorect.html. Accessed 12 Aug 2014
Kopetz S, Chang GJ, Overman MJ, Eng C, Sargent DJ, Larson DW, Grothey A, Vauthey JN, Nagorney DM, McWilliams RR (2009) Improved survival in metastatic colorectal cancer is associated with adoption of hepatic resection and improved chemotherapy. J Clin Oncol 27(22):3677–83
Hurwitz H, Fehrenbacher L, Novotny W, Cartwright T, Hainsworth J, Heim W, Berlin J, Baron A, Griffing S, Holmgren E, Ferrara N, Fyfe G, Rogers B, Ross R, Kabbinavar F (2004) Bevacizumab plus irinotecan, fluorouracil, and leucovorin for metastatic colorectal cancer. N Engl J Med 350(23):2335–42
Hurwitz HI, Tebbutt NC, Kabbinavar F, Giantonio BJ, Guan ZZ, Mitchell L, Waterkamp D, Tabernero J (2013) Efficacy and safety of bevacizumab in metastatic colorectal cancer: pooled analysis from seven randomized controlled trials. Oncologist 18(9):1004–12
Welch S, Spithoff K, Rumble RB, Maroun J, Gastronintestinal Cancer Disease Site Group (2010) Bevacizumab combined with chemotherapy for patients with advanced colorectal cancer: a systematic review. Ann Oncol 21(6):1152–62
Nipp RD, Ryan DP (2015) Should FOLFOXIRI plus bevacizumab be the standard first-line therapy in metastatic colorectal cancer? Oncologist 20(3):236–8
Dranitsaris G, Edwards S, Edwards J, Leblanc M, Abbott R (2010) Bevacizumab in combination with FOLFIRI chemotherapy in patients with metastatic colorectal cancer: an assessment of safety and efficacy in the province of Newfoundland and Labrador. Curr Oncol 17(5):12–16
Renouf DJ, Lim HJ, Speers C, Villa D, Gill S, Blanke CD, O’Reilly SE, Kennecke H (2011) Survival for metastatic colorectal cancer in the bevacizumab era: a population-based analysis. Clin Colorectal Cancer 10(2):97–101
Kamba T, McDonald DM (2007) Mechanisms of adverse effects of anti-VEGF therapy for cancer. Br J Cancer 96(12):1788–95
Schutz FA, Je Y, Azzi GR, Nguyen PL, Choueiri TK (2011) Bevacizumab increases the risk of arterial ischemia: a large study in cancer patients with a focus on different subgroup outcomes. Ann Oncol 22(6):1404–12
Alcalay A, Wun T, Khatri V, Chew HK, Harvey D, Zhou H, White RH (2006) Venous thromboembolism in patients with colorectal cancer: incidence and effect on survival. J Clin Oncol 24(7):1112–8
BC Cancer Agency (2006) Management guidelines for bevacizumab-related side effects in patients with colorectal cancer. BC Cancer Agency Cancer Management Guidelines. http://www.bccancer.bc.ca/NR/rdonlyres/6D39414F-EC1A-4BE2-9ACB-6DE017C9B4C4/19258/Managementforbevacizumabsideeffects_1Dec06.pdf. Accessed 14 April 2015
Khorana AA, Kuderer NM, Culakova E, Lyman GH, Francis CW (2008) Development and validation of a predictive model for chemotherapy-associated thrombosis. Blood 111(10):4902–7
Chong G (2010) Using bevacizumab with different chemotherapeutic regimens in metastatic colorectal cancer: balancing utility with low toxicity. Ther Adv Med Oncol 2(5):309–317
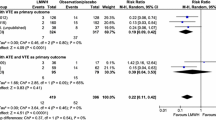
Nalluri SR, Chu D, Keresztes R, Zhu X, Wu S (2008) Risk of venous thromboembolism with the angiogenesis inhibitor bevacizumab in cancer patients: a meta-analysis. JAMA 300(19):2277–85
Mayer RJ (2001) Oral versus intravenous fluoropyrimidines for advanced colorectal cancer: by either route, it’s all the same. J Clin Oncol 19(21):4093–4096
Hurwitz HI, Saltz LB, Van Cutsem E, Cassidy J, Wiedemann J, Sirzén F, Lyman GH, Rohr UP (2011) Venous thromboembolic events with chemotherapy plus bevacizumab: a pooled analysis of patients in randomized phase II and III studies. J Clin Oncol 29(13):1757
Kalata P, Martus P, Zettl H, Rodel C, Hohenberger W, Raab R, Becker H, Leirsch T, Wittekind C, Sauer R, Fietkau R, German Rectal Cancer Study Group (2009) Differences between clinical trial participants and patients in a population-based registry: the German Rectal Cancer Study vs. the Rostock Cancer Registry. Dis Colon Rectum 52(3):425–37
Tsai AW, Cushman M, Rosamond WD, Heckbert SR, Polak JF, Folsom AR (2002) Cardiovascular risk factors and venous thromboembolism incidence: the longitudinal investigation of thromboembolism etiology. Arch Intern Med 162(10):1182
Anderson FA Jr, Wheeler HB, Goldberg RJ, Hosmer DW, Patwardhan NA, Jovanovic B, Forcier A, Dalen JE (1991) A population-based perspective of the hospital incidence and case-fatality rates of deep vein thrombosis and pulmonary embolism. The Worcester DVT Study. Arch Intern Med 151(5):933
Aldington S, Pritchard A, Perrin K, James K, Wijesinghe M, Beasley R (2008) Prolonged seated immobility at work is a common risk factor for venous thromboembolism leading to hospital admission. Intern Med J 38(2):133–5
Holst AG, Jensen G, Prescott E (2010) Risk factors for venous thromboembolism: results from the Copenhagen City Heart Study. Circulation 121(17):1896
Anderson FA Jr, Zayaruzyn M, Heit JA, Fidan D, Cohen AT (2007) Estimated annual numbers of US acute-care hospital patients at risk for venous thromboembolism. Am J Hematol 82(9):777–82
Ageno W, Becattini C, Brighton T, Selby R, Kamphuisen PW (2008) Cardiovascular risk factors and venous thromboembolism: a meta-analysis. Circulation 117(1):93
Sørensen HT, Horvath-Puho E, Søgaard KK, Christensen S, Johnsen SP, Thomsen RW, Prandoni P, Baron JA (2009) Arterial cardiovascular events, statins, low-dose aspirin and subsequent risk of venous thromboembolism: a population-based case–control study. J Thromb Haemost 7(4):521
Prandoni P, Bilora F, Marchiori A, Bernardi E, Petrobelli F, Lensing AW, Prins MH, Girolami A (2003) An association between atherosclerosis and venous thrombosis. N Engl J Med 348(15):1435
Lip GY, Gibbs CR (1999) Does heart failure confer a hypercoagulable state? Virchow’s triad revisited. J Am Coll Cardiol 33(5):1424
Acknowledgments
Authors would like to gratefully acknowledge the British Columbia Cancer Foundation and the Canadian Cancer Society Research Institute for their support in making this research possible.
Funding
This study was funded by the British Columbia Cancer Foundation and the Canadian Cancer Society Research Institute.
Conflicts of interest
The authors of the paper declare that they have no conflicts of interest.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Yu, I., Chen, L., Ruan, J.Y. et al. Risk and management of venous thromboembolisms in bevacizumab-treated metastatic colorectal cancer patients. Support Care Cancer 24, 1199–1208 (2016). https://doi.org/10.1007/s00520-015-2899-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00520-015-2899-y