Abstract
Purpose
To evaluate the efficacy of multifaceted interventions in reducing complications of peripherally inserted central venous catheter (PICC) in adult oncology patients.
Methods
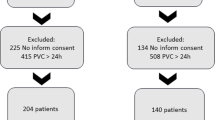
Multifaceted interventions were implemented in our department in December 2006. These interventions include: (1) A mandatory nurse reeducation was developed by a multidisciplinary task force; (2) Modification of peripherally inserted central catheter insertion: take a chest X-ray before removal of the guidewire and cutting of the catheter. The guidewire in the catheter facilitates the accurate location of the tip of PICC on chest X-ray and make the malposition correction (withdrawing, reinsertion, even reinsertion following withdrawal) easily; (3) Using a 2% chlorhexidine preparation, replace 10% povidone iodine for skin antisepsis; (4) Maintenance of maximum sterile barrier precautions during PICC insertion and aftercare; (5) Designing of a PICC archive form and establishing a PICC archive for each patient. The PICC complication rates of groups before and after interventions were evaluated and compared.
Results
Sixty-nine PICC lines were inserted before these interventions, and 165 were inserted after implementation of these interventions. Compared with preintervention group, the postintervention group was associated with a 62.14% decrease in the overall complication rate (11.52% vs 30.43% [P = 0.0004]; incidence density, 1.82 vs 4.62 per 1,000 PICC days) with a 67.48% decrease in the infective complications rate (4.24% vs 13.04% [P = 0.015]) with a 58.19% decrease in the noninfective complications rate (7.27% vs 17.39% [P = 0.0199]).
Conclusions
The results suggest that these interventions implemented in this study may be help in reducing complications of PICC in adult oncology patients.

Similar content being viewed by others
References
Abedin S, Kapoor G (2008) Peripherally inserted central venous catheters are a good option for prolonged venous access in children with cancer. Pediatr Blood Cancer 51(2):251–255. doi:10.1002/pbc.21344
Walshe LJ, Malak SF, Eagan J et al (2002) Complication rates among cancer patients with peripherally inserted central catheters. J Clin Oncol 20(15):3276–3281. doi:10.1200/JCO.2002.11.135
Cheong K, Perry D, Karapetis C et al (2004) High rate of complications associated with peripherally inserted central venous catheters in patients with solid tumours. Intern Med J 34(5):234–238. doi:10.1111/j.1444-0903.2004.00447.x
Trerotola SO, Thompson S, Chittams J et al (2007) Analysis of tip malposition and correction in peripherally inserted central catheters placed at bedside by a dedicated nursing team. J Vasc Interv Radiol 18(4):513–518. doi:10.1016/j.jvir.2007.01.020
Yap YS, Karapetis C, Lerose S et al (2006) Reducing the risk of peripherally inserted central catheter line complications in the oncology setting. Eur J Cancer Care 15(4):342–347. doi:10.1111/j.1365-2354.2006.00664.x
Pearson ML (1996) Guideline for prevention of intravascular device-related infections. Hospital Infection Control Practices Advisory Committee. Infect Control Hosp Epidemiol 17(7):438–473
Pittiruti M, Scoppettuolo G, La GA et al (2008) The EKG method for positioning the tip of PICCs: results from two preliminary studies. J Assoc Vasc Access 13(4):179–186. doi:10.2309/java.13-4-3
Hoffer EK, Borsa J, Santulli P et al (1999) Prospective randomized comparison of valved versus nonvalved peripherally inserted central vein catheters. AJR Am J Roentgenol 173(5):1393–1398
Michelle EH, Thanh HN, Allen JC (2004) Optimizing the patient positioning for PICC line tip determination. Emerg Radiol 10(4):186–189. doi:10.1007/s10140-003-0310-7
Mermel LA, Farr BM, Sherertz RJ et al (2001) Guidelines for the management of intravascular catheter related infections. Clin Infect Dis 32(9):1249–1272. doi:10.1086/320001
Racadio JM, Doellman DA, Johnson ND et al (2001) Pediatric peripherally inserted central catheters: complication rates related to catheter tip location. Pediatrics 107:E28
Infusion Nurses Society (2006) Infusion nursing standards of practice. J Infus Nurs 29(1 Suppl):S1–S92
Frey AM (1995) Pediatric peripherally inserted central catheter program report: a summary of 4,536 catheter days. J Intraven Nurs 18(6):280–291
Maki DG, Ringer M, Alvarado CJ (1991) Prospective randomized trial of povidone-iodine, alcohol, and chlorhexidine for prevention of infection associated with central venous and arterial catheters. Lancet 338(8763):339–343. doi:10.1016/0140-6736(91)90479-9
Ryder MA (1993) Peripherally inserted central venous catheters. Nurs Clin North Am 28(4):937–971
Hogan MJ (1999) Neonatal vascular catheters and their complications. Radiol Clin North Am 37(6):1109–1125
James L, Bledsoe L, Hadaway LC (1993) A retrospective look at tip location and complications of peripherally inserted central catheter lines. J Intraven Nurs 16(2):104–109
Kearns PJ, Coleman S, Wehner JH (1996) Complications of long arm-catheters: a randomized trial of central vs, peripheral tip location. JPEN J Parenter Enteral Nutr 20(1):20–24
Smith JR, Friedell ML, Cheatham ML et al (1998) Peripherally inserted central catheters revisited. Am J Surg 176:208–211. doi:10.1016/S0002-9610(98)00121-4
Naylor CL (2007) Reduction of malposition in peripherally inserted central catheters with tip location system. J Assoc Vasc Access 12(1):29–31
O’Grady NP, Alexander M, Dellinger EP et al (2002) Guidelines for the prevention of intravascular catheter-related infections. Am J Infect Control 30(8):476–489. doi:10.1067/mic.2002.129427
Pronovost P, Needham D, Berenholtz S et al (2006) An intervention to decrease catheter-related bloodstream infections in the ICU. N Engl J Med 355(26):2725–2732
Lawson T (1998) Infusion of IV medication and fluids via PICC and midline catheters: influences of tip position on the success of infusion. J Vasc Access Devices 3:11–17
Acknowledgement
This study was supported in part by a grant from the Science and Technology Grants for Medicine and Health Research from the Shenzhen Bureau of Science, Technology and Information. Grant Number: 200703272.
Conflict of interest statement
All authors declare no conflict of interests.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Tian, G., Zhu, Y., Qi, L. et al. Efficacy of multifaceted interventions in reducing complications of peripherally inserted central catheter in adult oncology patients. Support Care Cancer 18, 1293–1298 (2010). https://doi.org/10.1007/s00520-009-0747-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00520-009-0747-7