Abstract
Objective
The present study aimed to examine the effectiveness of intravenous administration of paracetamol added to morphine in the control of cancer pain and its possible contribution as reduction of opioid consumption and opioid-related side effects.
Materials and methods
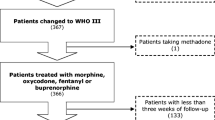
A total of 43 patients with chronic cancer pain without neuropathic origin aged between 18 and 76 years and receiving step 2 treatment according to the World Health Organization analgesic ladder were included. Patients were randomized to receive intravenous administration of saline (control) or 1 g of paracetamol on top of morphine. Visual analog scale (VAS), patient rating index (PRI), Eastern Cooperative Oncology Group (ECOG) status, patient satisfaction, and safety were evaluated.
Main results
Both treatments resulted in improved VAS and PRI scores compared to baseline. However, groups did not differ in terms of VAS and PRI scores, morphine consumption, side-effect frequencies, laboratory values, ECOG status, and patient satisfaction.
Conclusions
Although safe and there are signals for a true analgesic efficacy, our results failed to confirm any benefits of add-on treatment with intravenous administration of paracetamol. However, the study was underpowered, and future studies in this important area need to be wary of background noise and the risk of a type II error.

Similar content being viewed by others
References
Axelsson B, Stellborn P, Ström G (2008) Analgesic effect of paracetamol on cancer related pain in concurrent strong opioid therapy. A prospective clinical study. Acta Oncol 47:891–895
Blayney MR, Ryan JD, Malins AF (2003) Propofol target-controlled infusions for sedation—a safe technique for the non-anaesthetist? Br Dent J 194:450–452
Botting R, Ayoub SS (2005) COX 3 and the mechanism of action of paracetamol/acetaminophen. Prostaglandins, Leukotrienes and Essential Fatty Acids 72:85–87
Botting RM (2000) Mechanism of action of acetaminophen: is there a cyclooxygenase 3? Clin Infect Dis 31(Suppl 5):S202–210
Brune K, Zeilhofer HU (2003) Antipyretic analgesics. In: Melzack R, Wall PD (eds) Handbook of pain management. Churchill Livingstone, Edinburg, pp 1139–1153
Cherny N (2003) The management of cancer pain. In: Melzack R, Wall PD (eds) Handbook of pain management. Churchill Livingstone, Edinburg, pp 641–666
Delbos A, Boccard E (1995) The morphine sparing effect of propacetamol in orthopedic postoperative pain. J Pain Symptom Manage 10:279–286
Fitzgibbon DR, Chapman CR (2001) Cancer pain: assessment and diagnosis. In: Loeser JD (ed) Bonica's management of pain, IIIth edn. Lipponcott Williams & Wilkins, Philadelphia, pp 623–658
Graham GG, Scott KF, Day RO (2005) Tolerability of paracetamol. Drug Safety 28:227–240
Graham GG, Scott KF (2005) Mechanism of action of paracetamol. Am J Ther 12:46–55
Hardy J, Reymond E, Charles M (2005) Acetaminophen in cancer pain. J Clin Oncol 23:1586
Hernandez-Palazon J, Tortosa JA, Martinez-Lage JF, Perez-Flores D (2001) Intravenous administration of propacetamol reduces morphine consumption after spinal fusion surgery. Anesth Analg 92:1473–1476
New South Wales Therapeutic Advisory Group (2005) IV paracetamol-where does it sit in hospital practice? Current Opinion October 1-8.
Peduto VA, Ballabio M, Stefanini S (1998) Efficacy of propacetamol in the treatment of postoperative pain. Morphine-sparing effect in orthopedic surgery. Italian Collaborative Group on Propacetamol. Acta Anaesthesiol Scand 42:293–298
Pelissier T, Allou A, Caussade F, Dubray C, Cloarec A, Lavarenne J, Eschalier A (1996) Paracetamol exerts a spinal antinociceptive effect involving an indirect interaction with 5-hydroxytryptamine-3 receptors: in vivo and in vitro evidence. J Pharmacol Exp Ther 278:8–14
Pettersson PH, Jakobsson J, Öwall A (2005) Intravenous acetaminophen reduced the use of opioids compared with oral administration after coronary artery bypass grafting. J Cardiothorac Vasc Anesth 19:306–309
Prescott LF (2000) Therapeutic misadventure with paracetamol: fact or fiction. Am J Ther 7:99–114
Rodrigez MJ, Contreras D, Galvez R, Castro A, Camba MA, Busqueta C, Herrera J (2003) Double-blind evaluation of short-term analgesic efficacy of orally administered dexketoprofen trometamol and ketorolac in bone cancer pain. Pain 104:103–110
Schug SA (2005) Clinical pharmacology of non-opioid and opioid analgesics. In: Justins DM (ed) PAIN 2005-An Updated Review. IASP Press, Seattle, pp 31–38
Sinatra RS, Jahr JS, Reynolds LW, Viscusi ER, Groudine SB, Payen-Champenois C (2005) Efficacy and safety of single and repeated administration of 1 gram intravenous acetaminophen injection (paracetamol) for pain management after major orthopedic surgery. Anesthesiology 102:822–831
Stockler M, Vardy J, Pillai A, Warr D (2004) Acetaminophen (paracetamol) improves pain and well-being in people with advanced cancer already receiving a strong opioid regimen: A randomized, double-blind, placebo-controlled cross-over trial. J Clin Oncol 22:3389–3394
World Health Organization (1998) Cancer pain relief and palliative care in children. WHO, Geneva
World Health Organization (1996) Cancer pain relief, with a guide to opioid availability, 2nd edn. World Health Organization, Geneva
Zernikow B, Smale H, Michel E, Hasan C, Jorch N, Andler C (2006) Paediatric cancer pain management using the WHO analgesic ladder—results of a prospective analysis from 2265 treatment days during a guality improvement study. Eur J Pain 10:587–595
Dworkin RH, Turk DC, Farrar JT, Haythornthwaite JA, Jensen MP, Katz NP, Kerns RD et al (2005) Core outcome measures for chronic pain clinical trials: IMMPACT recommendations. Pain 113:9–19
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Tasmacioglu, B., Aydinli, I., Keskinbora, K. et al. Effect of intravenous administration of paracetamol on morphine consumption in cancer pain control. Support Care Cancer 17, 1475–1481 (2009). https://doi.org/10.1007/s00520-009-0612-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00520-009-0612-8