Abstract
Goals
Oral mucositis (OM), the painful inflammation of oropharyngeal tissues, is an economically costly chemotherapy toxicity. Several agents to prevent chemotherapy-induced OM are in development, with most studies conducted among transplantation subjects with a brief well-defined risk period. The potential value of these preventative agents among hematology-oncology populations receiving cyclic standard-dose therapy is unknown.
Patients and methods
Patients receiving standard-dose chemotherapy at an outpatient oncology center over a 2-week time-frame were invited to participate in an anonymous unprompted survey. The survey instrument consisted of six demographic questions and six questions regarding toxicities of chemotherapy.
Results
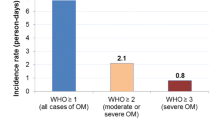
Of 514 patients providing completed surveys from among approximately 1625 patients (32% response rate), 167 (32%) reported experiencing OM. Factors associated with developing OM included number of chemotherapy cycles (P=0.001), hematologic malignancy (P=0.02), female gender (P=0.03), age (P=0.05), and treatment with anthracyclines (P=0.001), vinca alkaloids (P=0.001), cyclophosphamide (P=0.001), fludarabine (P=0.01), cis/carboplatin (P=0.05) and radiotherapy (P=0.005). Among patients experiencing OM, 69% considered OM to be an important toxicity with 7% rating their OM very severe, 18% severe, 36% moderate and 29% mild. Recurrent OM was reported by 87 patients (53%) and was judged similar in severity by 67%, milder by 27% and more severe by 6%. OM was considered the sixth most distressing complication behind (in descending order) fatigue, hair loss, nausea, numbness and diarrhea, and more important than anxiety and heartburn.
Conclusions
OM represents a common toxicity of standard-dose chemotherapy occurring in approximately one-third of patients. High-risk populations can be identified, permitting targeting of primary prophylaxis strategies whereby all patients possessing high-risk factors are treated to prevent OM. However, since OM was self-reported by only one-third of patients receiving standard-dose chemotherapy, but over half of those experiencing OM developed recurrent episodes, secondary prophylaxis strategies targeting recurrent OM episodes may be more appropriate.

Similar content being viewed by others
References
Bellm LA, Epstein JB, Rose-Ped A, Martin P, Fuchs HJ (2000) Patient reports of complications of bone marrow transplantation. Support Care Cancer 8:33–39
Dodd MJ, Dibble S, Miaskowski C, Paul S, Cho M, MacPhail L, Greenspan D, Shiba G (2001) A comparison of the affective state and quality of life of chemotherapy patients who do and do not develop chemotherapy-induced oral mucositis. J Pain Symptom Manage 21:498–505
Elting LS, Cooksley C, Chambers M, Cantor SB, Manzullo E, Rubenstein E (2003) The burdens of cancer therapy: clinical and economic outcomes of chemotherapy induced mucositis. Cancer 98:1531–1539
Epstein JB, Schubert MM (1999) Oral mucositis in myelosuppressive cancer therapy. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 88:273–276
Gralla R, Goldberg SL, Giles FJ (2003) Oral mucositis: emerging strategies for improving patient care. Oncology Special Edition, March 1–7
Heimdahl A, Mattsson T, Dahllof G, Lonnquist B, Ringden O (1989) The oral cavity as a port of entry for early infections in patients treated with bone marrow transplantation. Oral Surg Oral Med Oral Pathol 68:711–716
Manzullo E, Chambers M, Toth B, Rubenstein E, Elting L (1998) Outcomes and resource utilization in cancer patients with oral and gastrointestinal complications of chemotherapy. Proc Am Soc Clin Oncol 1605a
National Cancer Institute (2003) http://www.cancernet.nci.nih.gov
Rapoport AP, Miller Watelet LF, Linder T, Eberly S, Raubertas RF, Lipp J, Duerst R, Abboud CN, Constine L, Andrews J, Etter MA, Spear L, Powley E, Packman CH, Rowe JM, Schwertschlag U, Bedrosian C, Liesveld JL (1999) Analysis of factors that correlate with mucositis in recipients of autologous and allogeneic stem-cell transplants. J Clin Oncol 17:2446–2453
Ruescher TJ, Sodeifi A, Scrivani SJ, Kaban LB, Sonis ST (1998) The impact of mucositis on alphahemolytic streptococcal infection in patients undergoing autologous bone marrow transplantation for hematologic malignancies. Cancer 82:2275–2281
Sonis ST, Olser G, Fuchs H, Bellm L, Bradford W, Edlsberg J, Hayden V, Eilers J, Epstein J, LeVeque F, Miller C, Peterson D, Schubert MM, Spijkervet FK, Horowitz M (2001) Oral mucositis and the clinical and economic outcomes of hematopoietic stem cell transplantation. J Clin Oncol 19:2201–2205
Stiff P (2001) Mucositis associated with stem cell transplantation: current status and innovative approaches to management. Bone Marrow Transplant 27 [Suppl 2]:S3–S11
Worthington HV, Clarkson JE (2002) Prevention of oral mucositis and oral candidiasis for patients with cancer treated with chemotherapy: Cochrane Systematic Review. J Dent Educ 66:903–911
Worthington HV, Clarkson JE, Eden OB (2002) Interventions for treating oral mucositis for patients with cancer receiving treatment. Cochrane Database Systematic Review 1:CD001973.16
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Goldberg, S.L., Chiang, L., Selina, N. et al. Patient perceptions about chemotherapy-induced oral mucositis: implications for primary/secondary prophylaxis strategies. Support Care Cancer 12, 526–530 (2004). https://doi.org/10.1007/s00520-004-0640-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00520-004-0640-3