Summary
Background
The incidence of metabolic heart diseases has increased significantly in Middle Eastern countries such as Iran. The present study aimed to investigate the association between monocyte percentage to high-density cholesterol ratio (MHR), lymphocyte percentage to high-density cholesterol ratio (LHR), and lymphocyte to monocyte percentage ratio (LMR) and cardiometabolic diseases in a Kurdish population in the west of Iran.
Methods
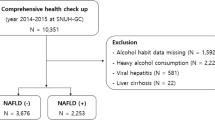
This study recruited 9803 individuals, 4728 (48.2%) were male and 5084 (51.8%) were female from Ravansar, Iran. All biomarkers were analyzed by the standard methods.
Results
The prevalence of cardiometabolic diseases was higher in overweight/obese participants and increased with age. MHR and LHR increased significantly in cardiometabolic individuals compared with healthy controls. Individuals in the fourth quartiles of LHR and MHR had higher odds ratio (ORs) for metabolic syndrome (MetS) and diabetes mellitus (DM) than the first quartiles. The LMR had a statistical association with non-alcoholic fatty liver disease (NAFLD) ORs and FLI. Besides, all these associations were stronger for females, and increased physical activity decreased inflammatory biomarkers.
Conclusion
The present study showed MHR and LHR had significant associations with ORs of MetS and DM. Also, MHR and LHR had a significant positive correlation with cardiometabolic risk factors. The LMR only had a statistical association with NAFLD and fatty liver index (FLI). Besides, the strong correlation between inflammatory biomarkers and cardiometabolic risk factors in females might be relevant to higher fat accumulation and metabolic inflammation background, and lower physical activity.

Similar content being viewed by others
References
Sattar N, Gill JM, Alazawi W. Improving prevention strategies for cardiometabolic disease. Nat Med. 2020;263:320–5.
Cai J, Zhang X-J, Ji Y-X, Zhang P, She Z-G, Li H. Nonalcoholic fatty liver disease pandemic fuels the upsurge in cardiovascular diseases. Circulation research. 2020;1265:679–704.https://doi.org/10.1161/CIRCRESAHA.119.316337.
Faasse S, Braun H, Vos M. The role of NAFLD in cardiometabolic disease: an update. F1000Res. 2018. https://doi.org/10.12688/f1000research.12028.1.
Ndisang JF, Rastogi S. Cardiometabolic diseases and related complications: current status and future perspective. Hindawi. 2013. https://doi.org/10.1155/2013/467682.
Nichols GA, Horberg M, Koebnick C, et al. Cardiometabolic risk factors among 1.3 million adults with overweight or obesity, but not diabetes, in 10 geographically diverse regions of the United States, 2012–2013. Prev Chronic Dis. 2017;14:E22.
Aksentijevich M, Lateef SS, Anzenberg P, et al. Chronic inflammation, cardiometabolic diseases and effects of treatment: psoriasis as a human model. Trends Cardiovasc Med. 2020;308:472–8.
Donath MY, Meier DT, Böni-Schnetzler M. Inflammation in the pathophysiology and therapy of cardiometabolic disease. Endocr Rev. 2019;404:1080–91.
Kantari C, Pederzoli-Ribeil M, Witko-Sarsat V. The role of neutrophils and monocytes in innate immunity. Trends Innate Immun. 2008;15:118–46.
Chapman CM, Beilby JP, McQuillan BM, et al. Monocyte count, but not C‑reactive protein or interleukin‑6, is an independent risk marker for subclinical carotid atherosclerosis. Stroke. 2004;357:1619–24.
Moro-García MA, Mayo JC, Sainz RM, et al. Influence of inflammation in the process of T lymphocyte differentiation: proliferative, metabolic, and oxidative changes. Front Immunol. 2018;9:339.
Ely BR, Clayton ZS, McCurdy CE, et al. Meta-inflammation and cardiometabolic disease in obesity: can heat therapy help? Temperature. 2018;51:9–21.
Berg A, Scherer P. The Online version of this article, along with updated information and services, is located on the World Wide Web. JAHA. 2005;96:939–49.
Osmond JM, Mintz JD, Dalton B, et al. Obesity increases blood pressure, cerebral vascular remodeling, and severity of stroke in the Zucker rat. Hypertension. 2009;532:381–6.
Ouchi N, Kihara S, Funahashi T, et al. Obesity, adiponectin and vascular inflammatory disease. Curr Opin Lipidol. 2003;146:561–6.
Shulman GI. Ectopic fat in insulin resistance, dyslipidemia, and cardiometabolic disease. N Engl J Med. 2014;371(12):1131–41.
Zhu X, Parks JS. New roles of HDL in inflammation and hematopoiesis. Annu Rev Nutr. 2012;32:161–82.
Mousa H, Islam N, Ganji V, et al. Serum 25-hydroxyvitamin D is inversely associated with monocyte percentage to HDL cholesterol ratio among young healthy adults in qatar. Nutrients. 2021;131:127.
Chen H, Xiong C, Shao X, et al. Lymphocyte to high-density lipoprotein ratio as a new indicator of inflammation and metabolic syndrome. Diabetes Metab Syndr Obes. 2019;12:2117.
Kizilgül M, Çalişkan M, Uçan B, et al. Monocyte to HDL cholesterol ratio and its association with cardio-metabolic risk factors in primary hyperparathyroidism. Medeniyet Med J. 2018;332:94–9.
Cekici Y, Yılmaz M, Seçen Ö. New inflammatory indicators: association of high eosinophil-to-lymphocyte ratio and low lymphocyte-to-monocyte ratio with smoking. J Int Med Res. 2019;479:4292–303.
Demirbaş A, Elmas ÖF, Atasoy M, et al. Can monocyte to HDL cholesterol ratio and monocyte to lymphocyte ratio be markers for inflammation and oxidative stress in patients with vitiligo? A preliminary study. Arch Dermatol Res. 2020. https://doi.org/10.1007/s00403-020-02129-3.
Sirin MC, Korkmaz S, Erturan I, et al. Evaluation of monocyte to HDL cholesterol ratio and other inflammatory markers in patients with psoriasis. An Bras Dermatol. 2020;95:575–82.
Yakar HI, Kanbay A, Ceylan E. Could monocyte/HDL cholesterol ratio predict cardiovascular events in patients with chronic obstructive pulmonary disease? Eur Respiratory Soc. 2017. https://doi.org/10.1183/1393003.congress-2017.PA1007.
Acikgoz N, Kurtoğlu E, Yagmur J, et al. Elevated monocyte to high-density lipoprotein cholesterol ratio and endothelial dysfunction in Behçet disease. Angiology. 2018;691:65–70.
X‑b WCF, J‑l H, et al. Novel risk biomarker for infective endocarditis patients with normal left ventricular ejection fraction—monocyte to high-density lipoprotein cholesterol ratio. Circ J. 2017;821:283–8.
Oh SW, Yi HJ, Lee DH, et al. Prognostic significance of various inflammation-based scores in patients with mechanical thrombectomy for acute ischemic stroke. World Neurosurg. 2020;141:e710–e7.
Asgari S, Moosaie F, Khalili D, et al. External validation of the European risk assessment tool for chronic cardio-metabolic disorders in a Middle Eastern population. J Transl Med. 2020;181:1–12.
Pasdar Y, Najafi F, Moradinazar M, et al. Cohort profile: ravansar non-communicable disease cohort study: the first cohort study in a Kurdish population. Int J Epidemiol. 2019;483:682–3f.
Ryan H, Trosclair A, Gfroerer J. Adult current smoking: differences in definitions and prevalence estimates—NHIS and NSDUH, 2008. J Environ Public Health. 2012. https://doi.org/10.1155/2012/918368.
Aadahl M, Jørgensen T. Validation of a new self-report instrument for measuring physical activity. Med Sci Sports Exerc. 2003;357:1196–202.
Rajati F, Hamzeh B, Pasdar Y, et al. Prevalence, awareness, treatment, and control of hypertension and their determinants: results from the first cohort of non-communicable diseases in a Kurdish settlement. Sci Rep. 2019;91:1–10.
Alberti K, Eckel RH, Grundy SM, et al. Harmonizing the metabolic syndrome: a joint interim statement of the international diabetes federation task force on epidemiology and prevention; national heart, lung, and blood institute; American heart association; world heart federation; international atherosclerosis society; and international association for the study of obesity. Circulation. 2009;120(16):1640–5.
Chobanian AV. National heart, lung, and blood institute joint national committee on prevention, detection, evaluation, and treatment of high blood pressure; national high blood pressure education program coordinating committee: the seventh report of the joint national committee on prevention, detection, evaluation, and treatment of high blood pressure: the JNC 7 report. JAMA. 2003;289:2560–72.
Huang X, Xu M, Chen Y, et al. Validation of the fatty liver index for nonalcoholic fatty liver disease in middle-aged and elderly Chinese. Medicine. 2015;94(40):e1682.
Foster M, Samman S. Zinc and regulation of inflammatory cytokines: implications for cardiometabolic disease. Nutrients. 2012;47:676–94.
Marseglia L, Manti S, D’Angelo G, et al. Oxidative stress in obesity: a critical component in human diseases. IJMS. 2015;161:378–400.
Yu S, Guo X, Li G, et al. Lymphocyte to high-density lipoprotein ratio but not platelet to lymphocyte ratio effectively predicts metabolic syndrome among subjects from rural China. Front Cardiovasc Med. 2021;8:107.
Yamamoto S, Narita I, Kotani K. The macrophage and its related cholesterol efflux as a HDL function index in atherosclerosis. Clin Chimica Acta. 2016;457:117–22.
Hu Y, Zhang H, Li J, et al. Gut-derived lymphocyte recruitment to liver and induce liver injury in non-alcoholic fatty liver disease mouse model. J Gastroenterol Hepatol. 2016;313:676–84.
Zhang J, Chen W, Fang L, et al. Increased intermediate monocyte fraction in peripheral blood is associated with nonalcoholic fatty liver disease. Wien Klin Wochenschr. 2018;130(11-12):390–7.
Monteiro R, Teixeira D, Calhau C. Estrogen signaling in metabolic inflammation. Mediators Inflamm. 2014. https://doi.org/10.1155/2014/615917.
Onat A, Karadeniz Y, Tusun E, et al. Advances in understanding gender difference in cardiometabolic disease risk. Expert Rev Cardiovasc Ther. 2016;144:513–23.
Acknowledgements
The authors are deeply grateful to the investigators of PERSIAN for their valuable support for designing the methods and developing the questionnaire. We also appreciate our interviewers, RaNCD staff, and Ravansar population for their significant cooperation in data collection.
Funding
This study was supported by the Ministry of Health and Medical Education of Iran and Kermanshah University of Medical Science (Grant No: 92472). The funder had no role in the design of the study, collection, analysis, and interpretation of the data, or writing and approval of manuscript.
Author information
Authors and Affiliations
Contributions
Maryam Kohsari conceived this study. Mehdi Moradinazar and Maryam Kohsari analyzed the data. All authors, including Maryam Kohsari, Mehdi Moradinazar, Zohreh Rahimi, Farid Najafi, Yahya Pasdar, and Ebrahim Shakiba, produced the first draft. All authors contributed to the multiple revisions and approved the final submission.
Corresponding author
Ethics declarations
Conflict of interest
M. Kohsari, M. Moradinazar, Z. Rahimi, F. Najafi, Y. Pasdar and E. Shakiba declare that they have no competing interests.
Ethical standards
All procedures performed in studies involving human participants or on human tissue were in accordance with the ethical standards of the institutional and/or national research committee and with the 1975 Helsinki declaration and its later amendments or comparable ethical standards. The study was approved by the ethics committees of Kermanshah University of Medical Sciences (KUMS.REC.1394.315), Kermanshah, Iran. All participants entered the study after they were fully informed of the process and signed a written consent.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Data availability
The datasets used and analyzed during the current study are available on reasonable request from the corresponding author
Rights and permissions
About this article
Cite this article
Kohsari, M., Moradinazar, M., Rahimi, Z. et al. New inflammatory biomarkers (lymphocyte and monocyte percentage to high-density lipoprotein cholesterol ratio and lymphocyte to monocyte percentage ratio) and their association with some cardiometabolic diseases. Wien Klin Wochenschr 134, 626–635 (2022). https://doi.org/10.1007/s00508-022-02029-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00508-022-02029-8