Summary
Background
Disease and aging-related factors may predispose chronic obstructive pulmonary disease (COPD) patients to impaired balance, although the underlying determinants of impaired balance in COPD patients are still unknown. The purpose of this study was to identify the determinants of impaired balance in COPD patients. Also, we aimed to determine which balance measures (clinical or laboratory tests) are more indicative in determining balance impairment in these patients.
Methods
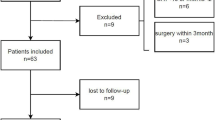
This cross-sectional study recruited 24 patients with moderate to severe COPD and 24 age-matched healthy subjects. Participants were evaluated regarding demographic and clinical data, previous falls history, lower limb muscle strength, exercise capacity, physical activity and balance level.
Results
COPD patients exhibited significantly a longer test duration on timed up and go test, a higher sway index on the postural stability and lower directional control score on the limit of stability of Biodex balance system (all, p < 0.001) compared to healthy controls, whereas there was no difference in Berg balance scale score between groups (p > 0.05). Balance impairment of the patient group was significantly associated with nonpulmonary conditions, such as physical activity level, exercise capacity, lower limb muscle strength, and with fall history. Also, COPD patients represented significantly lower physical activity level and exercise capacity, weaker lower limb muscle strength than healthy controls (all, p < 0.001).
Conclusions
Patients with moderate to severe COPD exhibit apparently important reductions in balance control that is directly associated with nonpulmonary consequences and fall history. These results may be extremely important to fall prevention and to guide the development of interventions for this population.
Similar content being viewed by others
References
Han MK, Agusti A, Calverley PM, Celli BR, Criner G, Curtis JL, et al. Chronic obstructive pulmonary disease phenotypes: the future of COPD. Am J Respir Crit Care Med. 2010;182:598–604.
Park JK, Deutz NEP, Cruthirds CL, Kirschner SK, Park H, Madigan ML, et al. Risk factors for postural and functional balance impairment in patients with chronic obstructive pulmonary disease. J Clin Med. 2020;9(2):609.
Loughran KJ, Atkinson G, Beauchamp MK, Dixon J, Martin D, Rahim S, et al. Balance impairment in individuals with COPD: a systematic review with meta-analysis. Thorax. 2020;75:539–46.
Ozalevli S, Ilgin D, Narin S, Akkoclu A. Association between disease-related factors and balance and falls among the elderly with COPD: a cross-sectional study. Aging Clin Exp Res. 2011;23:372–7.
de Castro LA, Ribeiro LR, Mesquita R, de Carvalho DR, Felcar JM, Merli MF, et al. Static and functional balance in individuals with COPD: comparison with healthy controls and differences according to sex and disease severity. Respir Care. 2016;61:1488–96.
Chuatrakoon B, Ngai SPC, Sungkarat S, Uthaikhup S. Balance impairment and effectiveness of exercise intervention in chronic obstructive pulmonary disease—a systematic review. Arch Phys Med Rehabil. 2020;101:1590–602.
Beauchamp MK, Sibley KM, Lakhani B, Romano J, Mathur S, Goldstein RS, et al. Impairments in systems underlying control of balance in COPD. Chest. 2012;141:1496–503.
Oliveira CC, Lee AL, McGinley J, Anderson GP, Clark RA, Thompson M, et al. Balance and falls in acute exacerbation of chronic obstructive pulmonary disease: a prospective study. COPD. 2017;14:518–25.
Roig M, Eng JJ, Road JD, Reid WD. Falls in patients with chronic obstructive pulmonary disease: a call for further research. Respir Med. 2009;103:1257–69.
Porto EF, Castro AA, Schmidt VG, Rabelo HM, Kumpel C, Nascimento OA, et al. Postural control in chronic obstructive pulmonary disease: a systematic review. Int J Chron Obstruct Pulmon Dis. 2015;10:1233–9.
Oliveira CC, Lee A, Granger CL, Miller KJ, Irving LB, Denehy L. Postural control and fear of falling assessment in people with chronic obstructive pulmonary disease: a systematic review of instruments, international classification of functioning, disability and health linkage, and measurement properties. Arch Phys Med Rehabil. 2013;94:1784–1799.e7.
Mirza S, Clay RD, Koslow MA, Scanlon PD. COPD guidelines: a review of the 2018 GOLD report. Mayo Clin Proc. 2018;93:1488–502.
Crisan AF, Oancea C, Timar B, Fira-Mladinescu O, Tudorache V. Balance impairment in patients with COPD. PLoS ONE. 2015;10:e120573.
Wanger J, Clausen JL, Coates A, Pedersen OF, Brusasco V, Burgos F, et al. Standardisation of the measurement of lung volumes. Eur Respir J. 2005;26:511–22.
Cachupe WJ, Shifflett B, Kahanov L, Wughalter EH. Reliability of biodex balance system measures. Meas Phys Educ Exerc Sci. 2001;5:97–108.
Mkacher W, Tabka Z, Trabelsi Y. Minimal detectable change for balance measurements in patients with COPD. J Cardiopulm Rehabil Prev. 2017;37:223–8.
Hauer K, Lamb SE, Jorstad EC, Todd C, Becker C. Systematic review of definitions and methods of measuring falls in randomised controlled fall prevention trials. Age Ageing. 2006;35:5–10.
Wang C‑Y, Olson SL, Protas EJ. Test-retest strength reliability: hand-held dynamometry in community-dwelling elderly fallers. Arch Phys Med Rehabil. 2002;83:811–5.
ATS Committee on Proficiency Standards for Clinical Pulmonary Function Laboratories. ATS statement: guidelines for the six-minute walk test. Am J Respir Crit Care Med. 2002;166:111–7.
Saglam M, Arikan H, Savci S, Inal Ince D, Boşnak Güçlü M, Karabulut E, et al. International physical activity questionnaire: reliability and validity of the Turkish version. Percept Mot Skills. 2010;111:278–84.
Munari AB, Gulart AA, Dos Santos K, Venâncio RS, Karloh M, Mayer AF. Modified medical research council dyspnea scale in GOLD classification better reflects physical activities of daily living. Respir Care. 2018;63:77–85.
Smith MD, Chang AT, Seale HE, Walsh JR, Hodges PW. Balance is impaired in people with chronic obstructive pulmonary disease. Gait Posture. 2010;31:456–60.
Beauchamp MK, O’Hoski S, Goldstein RS, Brooks D. Effect of pulmonary rehabilitation on balance in persons with chronic obstructive pulmonary disease. Arch Phys Med Rehabil. 2010;91:1460–5.
Bennie S, Bruner K, Dizon A, Fritz H, Goodman B, Peterson S. Measurements of balance: comparison of the timed “up and go” test and functional reach test with the Berg balance scale. J Phys Ther Sci. 2003;15:93–7.
Butcher SJ, Meshke JM, Sheppard MS. Reductions in functional balance, coordination, and mobility measures among patients with stable chronic obstructive pulmonary disease. J Cardiopulm Rehabil. 2004;24:274–80.
Beauchamp MK, Hill K, Goldstein RS, Janaudis-Ferreira T, Brooks D. Impairments in balance discriminate fallers from non-fallers in COPD. Respir Med. 2009;103:1885–91.
Bradley JM, Lasserson T, Elborn S, Macmahon J, O’Neill B. A systematic review of randomized controlled trials examining the short-term benefit of ambulatory oxygen in COPD. Chest. 2007;131:278–85.
Ribeiro F, Oliveira J. Aging effects on joint proprioception: the role of physical activity in proprioception preservation. Eur Rev Aging Phys Act. 2007;4:71.
Katajisto M, Kupiainen H, Rantanen P, Lindqvist A, Kilpelainen M, Tikkanen H, et al. Physical inactivity in COPD and increased patient perception of dyspnea. Int J Chron Obstruct Pulmon Dis. 2012;7:743–55.
Janssens L, Brumagne S, McConnell AK, Claeys K, Pijnenburg M, Burtin C, et al. Proprioceptive changes impair balance control in individuals with chronic obstructive pulmonary disease. PLoS One. 2013;8:e57949.
Evans RA, Kaplovitch E, Beauchamp MK, Dolmage TE, Goldstein RS, Gillies CL, et al. Is quadriceps endurance reduced in COPD?: A systematic review. Chest. 2015;147:673–84.
Hodges PW, Gurfinkel VS, Brumagne S, Smith TC, Cordo PC. Coexistence of stability and mobility in postural control: evidence from postural compensation for respiration. Exp Brain Res. 2002;144:293–302.
Schmid M, Conforto S, Bibbo D, D’Alessio T. Respiration and postural sway: detection of phase synchronizations and interactions. Hum Mov Sci. 2004;23:105–19.
Pedrozo MD, de Silveira AF. Balance assessment in people with chronic obstructive pulmonary disease. Fisioter Mov. 2015;28:149–56.
Smith MD, Chang AT, Hodges PW. Balance recovery is compromised and trunk muscle activity is increased in chronic obstructive pulmonary disease. Gait Posture. 2016;43:101–7.
Ku PX, Abu Osman NA, Wan Abas WAB. The limits of stability and muscle activity in middle-aged adults during static and dynamic stance. J Biomech. 2016;49:3943–8.
Beauchamp MK. Balance assessment in people with COPD: an evidence-based guide. Chron Respir Dis. 2019;16:1479973118820311.
Nguyen US, Kiel DP, Li W, Galica AM, Kang HG, Casey VA, et al. Correlations of clinical and laboratory measures of balance in older men and women. Arthritis Care Res (Hoboken). 2012;64:1895–902.
Acknowledgements
We appreciate all the people who cooperated in this research.
Author information
Authors and Affiliations
Contributions
M. Eymir and H. Yakut designed and performed the research, and analyzed the data. M. Eymir, H. Yakut and S. Özalevli drafted the manuscript. S. Özalevli and A. Ö. Alpaydın reviewed and modified the manuscript. All authors have read and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of interest
M. Eymir, H. Yakut, S. Özalevli and A. Ö. Alpaydın declare that they have no competing interests.
Ethical standards
This study was conducted in accordance with the Declaration of Helsinki and approved by the Medical Ethics Committee of Dokuz Eylul University. Informed consent was obtained from all individual participants included in the study.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Eymir, M., Yakut, H., Özalevli, S. et al. Static and dynamic balance impairment and relationship with disease-related factors in patients with chronic obstructive pulmonary disease. Wien Klin Wochenschr 133, 1186–1194 (2021). https://doi.org/10.1007/s00508-021-01918-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00508-021-01918-8