Summary
Background
Body temperature control is a frequently used screening test for infectious diseases, such as Covid-19 (Sars-CoV-2). We used this procedure to test the body temperature of staff members in a hospital in Tyrol (Austria), where the Covid-19 disease occurred in March 2020. The hospital is located in a mountain area at 995 m above sea level with low outdoor temperatures during early spring season. Under these conditions, we analyzed whether forehead temperature control offers a sufficient screening tool for infectious diseases.
Methods
Forehead temperature of 101 healthy male and female employees was measured with an infrared thermometer directly after entering the hospital (0 min), followed by further controls after 1 min, 3 min, 5 min and 60 min. We also tracked the outside temperature and the temperature at the entrance hall of the hospital.
Results
Complete data of body temperature were available for 46 female and 46 male study participants. The average forehead temperature measured directly after entrance to the hospital was the lowest (0 min) 33.17 ± 1.45 °C, and increased constantly to 34.90 ± 1.49 °C after 1 min, 35.77 ± 1.10 °C after 3 min, 36.08 ± 0.79 °C after 5 min, and 36.6 ± 0.24 °C after 60 min. The outside temperature ranged between −5.5 °C and 0 °C, the indoor temperature had a constant value of 20.5 °C.
Conclusion
Our results indicate that forehead infrared temperature control is not an appropriate tool to screen for infectious disease directly at the entrance of a building, at least during early spring season with cold outdoor temperatures.
Similar content being viewed by others
Introduction
Covid-19 (Sars-CoV-2) is a dangerous infectious disease with the risk of life-threatening pulmonary complications [1, 2]. Since the number of infected people and the mortality rates increase worldwide, many countries decided for a nationwide lockdown [3]. Further strategies focus on early diagnosis of Sars-CoV‑2 infection, which is known to result in flu-like symptoms, such as fever, sore throat and dry cough [1, 4, 5]. Social contact with infected people is considered as a high-risk situation and, therefore, several institutions, including hospitals, implemented screening areas including temperature controls at the entrance [3, 6, 7].
The pandemic of Sars-CoV‑2 reached Tyrol in March 2020. The hospital Hochzirl (Hochzirl 1, 6170 Zirl, Austria), a geriatric and neurological institution situated in a mountain area at 995 m above sea level, started with temperature screening for all staff members immediately after the onset of the pandemic. The hospital operator decided to deny access for the clinical personal if the body temperature was above 37.4 °C. Beside this, information about the need of social distancing, hygiene standards and the use of the personal protective equipment was provided.
Because of the low outdoor temperatures at this season, especially in the morning, a debate started whether routinely performed temperature controls of staff members might be a sufficient tool to detect possibly infected people. To the best of our knowledge, only few published data are available about the relationship between forehead temperature measurements and the outdoor climate situation. Therefore, we performed temperature controls directly at the entrance of the hospital Hochzirl, followed by further measurements up to 1h, which was considered as a steady state body temperature.
Methods
Study participants
A total of 101 members of the hospital staff (women 52, men 49) gave their consent to participate in the study (54 physicians and medical students, 16 nurses, 19 physiotherapists and 12 office workers). Since 9 of the study participants were not available after 1h (e.g. due to meetings), we were able to rely on a final sample of 92 persons where full information on body temperature was available.
At the entrance to the hospital, all study participants wore winter clothing, but no headgear (e.g., hat or headband). There are three different ways for study participants to reach the hospital’s entrance with the screening area: (1) by car followed by a walk of approximately 160 m from the parking place (2 min), (2) by train with a 1.2 km walk (13 min and +80 m altitude) and (3) a steep 500 m path from the train station through the forest (+80 m altitude 7 min). The corresponding distances, times and altitudes were taken from Guru maps pro v4.4.9 (6841).
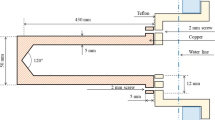
Temperature control
Temperature control was performed at the entrance to the hospital between 7 and 8 a.m. All measurements were taken by Trimedika TR 1 infrared Thermometer for clinical use (TriMedika, Belfast, Northern Ireland, Great Britain). The lens of the TriMedika thermometer focuses the infrared energy to a detector, which converts the energy to an electrical signal that can be displayed in °C after being compensated for ambient temperature variation. This configuration facilitates temperature measurement from a distance without contact to the skin [8]. The device was equilibrated for 15–20 min at room temperature. Body temperature was taken at the forehead, two fingers widths from the skin at an exposed area, free from hair [8].
Temperature was displayed within a range of 32–42 °C. Below and above these limits, temperatures at the thermometer were reported as “low” and “high”.
Values below 32 °C were frequently observed in our sample, values above 42 °C were not observed (Table 1). To carry out the statistical analysis, we fixed these body temperatures at 32 °C. To check the sensitivity of our results, we used alternative values of 31 °C and 30 °C, but it turned out that in qualitative terms our findings were robust against this change.
Measurement and data collection
Between 30 March 2020 and 3 April 2020 the forehead temperature of 101 participants was taken according to the manual [8]. Measurements were performed directly after entering the hospital at 0 min, followed by controls after 1 min, 3 min and 5 min (time period between 07:20 am and 08:00 am). For these measurements, participants were seated in the entrance area without change of clothing and without eating or drinking. A final temperature measurement performed after 1 h at the working place of the participants was considered as a steady state situation.
The outside temperature was determined by use of 3 different car thermometers and calculation of the average value, ranging from −5.5 to 0 °C. The temperature in the entrance hall was taken from built in thermostats (20.5 °C).
Statistical analysis
The sample size was determined for connected samples and constant target values with a significance level (alpha) of 0.05, 80% statistical power and a Cohen’s d of 0.3. This obtains a sample size of N = 89 [9]. Due to possible missing values, a size of 101 was chosen. Missing values were excluded (N = 9), the final sample size was N = 92 (46 males and 46 females).
Body temperature was taken for 0 min, 1 min, 3 min, 5 min and 60 min, respectively. For each measurement, we calculated the mean, median and standard deviation of body temperature. To carry out a pairwise comparison of mean temperatures, we applied a one-way ANOVA for repeated samples and unequal variances [10]. Apart from the timing of measurement, we were interested if the participants’ body temperature was affected by their gender and the outside as well as inside temperatures. For this purpose, we used a standard regression framework [10]. All the calculations are carried out with Stata (version 16, StataCorp, College Station, TX, USA).
Results
The temperature measured directly after entrance to the hospital was low (33.17 ± 1.45 °C) in all participants and increased thereafter, reaching a steady state after 1 h (Table 1). The average forehead temperature was 34.90 ± 1.49 °C after 1 min, 35.77 ± 1.10 °C after 3 min, 36.08 ± 0.79 °C after 5 min and 36.60 ± 0.24 °C after 1 h.
Our empirical findings suggest that the timing of measurement was important (Table 2). On average, the body temperature increased by about 0.8 °C within the observational time span. The effect of gender was insignificant, and the outside temperature had an impact of around 0.08. Accordingly, a 1 °C higher outside temperature was associated, on average, with a higher body temperature of 0.08 °C. Note that inside temperature was constant over the study period and is, therefore, captured in the constant.
Fig. 1 shows the time pattern of the observed body temperature along with the 5% and the 0.01% CI. It suggests significant differences over all measurements. More systematically, the ANOVA of pairwise comparisons between mean temperatures revealed a highly significant difference for forehead temperature across all measurements (Table 2).
Finally, we observed a difference between the measurement at the entrance and 1h later of around 3.4 °C (Table 3). This difference was significantly negative, suggesting that taking the forehead measurement at the entrance of the hospital systematically underestimates a person’s body temperature. This difference remains substantial when comparing the entrance measurement with shorter follow-up measurements. It should be noticed that the differences reported in Table 2 represent conservative estimates as we fixed the body temperature at 32 °C when the thermometer displayed a value of “low” (setting this value arbitrarily to 31 °C and 30 °C, this mean difference between 0 min and 60 min increased to −3.9 °C and −4.4 °C, respectively, which are both significant with a p-value far below 0.001).
Discussion
The main advantage of control of forehead temperature measurement is seen as the possibility for a quick and cost-effective decisions about permitting access to a hospital directly at an entrance. According to the results of our study there exist several limitations that should be considered with this procedure. We could observe that body temperature is underestimated by forehead measurements, when the controls are taken at the entrance of a building, especially during winter and early spring season with cold outdoor temperatures. These data are in accordance with the results of previously published studies on how physical activity [11, 12] and sun exposure [13] affect skin temperature. Although the screening procedure of temperature measurements may be seen as a psychological signal, emphasizing the importance to be conscious about infectious disease, the limitations of this method have to be considered.
Because thermal imaging cameras are described as an alternative tool to screen for people with increased body temperature, we have performed a literature search about the relevance of this procedure [15, 16]. Published literature describe that also imaging cameras should only be used in a standardized environment, especially free from secondary infrared sources, such as incandescent lamps or direct sunlight. In order to ensure the quality of the measurements [15, 16]. Moreover the results should be correlated with e.g. epitympanic measurement [16], but also epitympanic measurements are influenced by ambient and low temperatures [14].
The results of our study show that forehead temperature measurement is not an appropriate tool for screening for infectious disease during cold outdoor temperatures.
The relevance of temperature measurements in the course of screening for infectious diseases should therefore be critically discussed.
Key points
-
Forehead temperature measurement is not an appropriate tool for screening for infectious diseases during cold outdoor temperatures.
-
Body temperature is systematically underestimated when taken at the forehead and at the entrance of a building, especially during the winter and cold outdoor temperatures.
References
Guan W, Ni Z, Hu Y, Liang W, Ou C, He J, et al. Clinical Characteristics of Coronavirus Disease 2019 in China. N Engl J Med. 2020. https://doi.org/10.1056/nejmoa2002032.
Li Q, Guan X, Wu P, Wang X, Zhou L, Tong Y, et al. Early transmission dynamics in Wuhan, China, of novel Coronavirus-infected pneumonia. N Engl J Med. 2020;382(13):1199–207.
Klompas M, Morris CA, Sinclair J, PAearson M, Shenoy ES. Universal masking in hospitals in the Covid-19 era. N Engl J Med. 2020; https://doi.org/10.1056/NEJMp2006372?articleTools=true.
Singhal T. A review of Coronavirus disease-2019 (COVID-19). Indian J Pediatr. 2020;87(4):281–6.
Chen N, Zhou M, Dong X, Qu J, Gong F, Han Y, et al. Epidemiological and clinical characteristics of 99 cases of 2019 novel coronavirus pneumonia in Wuhan, China: a descriptive study. Lancet. 2020;395(10223):507–13. https://doi.org/10.1016/S0140-6736(20)30211-7.
Bitar D, Goubar A, Desenclos JC. International travels and fever screening during epidemics: a literature review on the effectiveness and potential use of non-contact infrared thermometers. Euro Surveill. 2009;14:1–5.
Gostic KM, Gomez ACR, Mummah RO, Kucharski AJ, Lloyd-Smith JO. Estimated effectiveness of symptom and risk screening to prevent the spread of COVID-19. Elife. 2020;9:1–18.
Manual TriTemp Non-contact-thermometer Part No CWC017 Revision 0619. 2020.
Fallzahlschätzung für verbundene Stichproben und stetige Zielgrößen. http://jumbo.uni-muenster.de/fileadmin/jumbo/applets/falla.html. Last access: 25.03.2020.
Casella G, Berger RL. Statistical Inference. 2nd ed. Duxbury: Pacific-Grove; 2002.
Bagley RJ, Judelson AD, Spiering AB, Beam CW, Bartolini JA, Washburn VB, et al. Validity of field expedient devices to assess core temperature during exercise in the cold. Aviat Space Environ Med. 2011;82(12):1098–103.
Casa DJ, Becker SM, Ganio MS, Brown CM, Yeargin SW, Roti MW, et al. Validity of devices that assess body temperature during outdoor exercise in the heat. J Athl Train. 2007;42(3):333–42.
Petersen B, Philipsen PA, Wulf HC. Skin temperature during sunbathing—relevance for skin cancer. Photochem Photobiol Sci. 2014;13(8):1123–5. https://doi.org/10.1039/C4PP00066H.
Strapazzon G, Procter E, Putzer G, Avancini G, Dal Cappello T, Überbacher N, et al. Influence of low ambient temperature on epitympanic temperature measurement: a prospective randomized clinical study. Scand J Trauma Resusc Emerg Med. 2015;23(1):1–6. https://doi.org/10.1186/s13049-015-0172-5.
Lahiri BB, Bagavathiappan S, Jayakumar T, Philip J. Medical applications of infrared thermography: A review. Infrared Phys Technol. 2012;55(4):221–35. https://doi.org/10.1016/j.infrared.2012.03.007.
Ng EY, Kaw GJ, Chang WM. Analysis of IR thermal imager for mass blind fever screening. Microvasc Res. 2004;68(2):104–9. https://doi.org/10.1016/j.mvr.2004.05.003.
Funding
This research received no specific grant from any funding agency in the commercial, public, or not-for-profit sectors.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
C. Dzien, W. Halder, H. Winner, and M. Lechleitner declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Dzien, C., Halder, W., Winner, H. et al. Covid-19 screening: are forehead temperature measurements during cold outdoor temperatures really helpful?. Wien Klin Wochenschr 133, 331–335 (2021). https://doi.org/10.1007/s00508-020-01754-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00508-020-01754-2