Summary
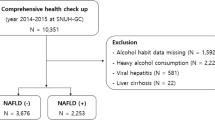
Nonalcoholic fatty liver disease (NAFLD) currently represents the most common hepatic disease worldwide and is closely linked to cardiovascular disease, obesity and diabetes mellitus. This study aimed to investigate NAFLD and its influence on different monocyte subpopulations to determine the presence of significant associations. A total of 3 monocyte subpopulations were investigated, i.e. classical (CD14++CD16−), intermediate (CD14++CD16+) and non-classical (CD14+CD16++). Of the participants 261 were included in this study (n = 53 with NAFLD, n = 208 controls). Ultrasonography was used to diagnose NAFLD and exclude other morphologic causes of liver diseases and other tests (including medical history inquiries and detection of hepatitis virus) were performed to exclude other causes of parenchymal liver disease. Classical inflammatory and metabolic-related NAFLD biomarkers were also determined. In contrast to the healthy control group, the intermediate monocyte fraction was increased in NAFLD patients (p = 0.032), while the classical monocyte fraction was decreased (p = 0.025). Intermediate monocyte fraction, body mass index (BMI) and tumor necrosis factor alpha (TNF-α) were independent risk factors for NAFLD. Classical, non-classical and intermediate monocytes fraction were strongly associated with age, triglyceride, and waist circumference. This study suggests that the intermediate monocyte fraction in peripheral blood is likely related to the aggravation of NAFLD.


Similar content being viewed by others
Abbreviations
- ALT:
-
Alanine transaminase
- AST:
-
Aspartate transaminase
- BMI:
-
Body mass index
- CM:
-
Classical monocyte
- ECG:
-
Electrocardiogram
- FPG:
-
Fasting plasma glucose
- GGT:
-
Gamma-glutamyl transferase
- HDL-C:
-
High-density lipoprotein cholesterol
- HOMA-IR:
-
Homeostasis model assessment-estimated insulin resistance
- IM:
-
Intermediate monocytes
- IR:
-
Insulin resistance
- LDL-C:
-
Low-density lipoprotein cholesterol
- LPS:
-
Lipopolysaccharide
- NAFLD:
-
Nonalcoholic fatty liver disease
- NASH:
-
Nonalcoholic steatohepatitis
- NCM:
-
Non-classical monocytes.
- NK:
-
Natural killer cells
- PBMC:
-
Peripheral blood monocytes
- TC:
-
Total cholesterol
- TG:
-
Triglyceride
- TNF-α:
-
Tumor necrosis factor alpha
References
Tuyama AC, Chang CY. Non-alcoholic fatty liver disease. J Diabetes. 2012;4:266–80.
Aygun C, Kocaman O, Sahin T, Uraz S, Eminler AT, Celebi A, Senturk O, Hulagu S. Evaluation of metabolic syndrome frequency and carotid artery intima-media thickness as risk factors for atherosclerosis in patients with nonalcoholic fatty liver disease. Dig Dis Sci. 2008;53:1352–7.
Shoelson SE, Herrero L, Naaz A. Obesity, inflammation, and insulin resistance. Gastroenterology. 2007;132:2169–80.
Sheth SG, Gordon FD, Chopra S. Nonalcoholic steatohepatitis. Ann Intern Med. 1997;126:137–45.
Shimada M, Hashimoto E, Taniai M. Hepatocellular carcinoma in patients with non-alcoholic steatohepatitis. J Hepatol. 2002;37:154–60.
Sugimoto K, Takei Y. Clinicopathological features of nonalcoholic fatty liver disease. Hepatol Res. 2011;41:911–20.
Baffy G. Kupffer cells in non-alcoholic fatty liver disease: the emerging view. J Hepatol. 2011;51:212–23.
Stansfield BK, Ingram DA. Clinical significance of monocyte heterogeneity. Clin Transl Med. 2015;4:4–5.
Gordon S, Taylor PR. Monocyte and macrophage heterogeneity. Nat Rev Immunol. 2005;5:953–64.
Wong KL, Tai JJ, Wong WC. Gene expression profiling reveals the defining features of the classical, intermediate, and nonclassical human monocyte subsets. Blood. 2011;118:e16–e31.
Anbazhagan K, Duroux-Richard I, Jorgensen C, Apparailly F. Transcriptomic network support distinct roles of classical and non-classical monocytes in human. Int Rev Immunol. 2014;33:470–89.
Seidler S, Zimmermann HW, Weiskirchen R, Trautwein C, Tacke F. Elevated circulating soluble interleukin-2 receptor in patients with chronic liver diseases is associated with non-classical monocytes. BMC Gastroenterol. 2012;12:38.
Zawada AM, Rogacev KS, Rotter B, Winter P, Marell RR, Fliser D, Heine GH. Super SAGE evidence for CD14+CD16+monocytes as a third monocyte subset. Blood. 2011;118:50–61.
Fingerle G, Pforte A, Passlick B, Blumenstein M. The novel subset of CD14+/CD16+ blood monocytes is expanded in sepsis patients. Blood. 1993;82:3170–6.
Hepburn AL, Mason JC, Davies KA. Expression of Fcgamma and complement receptors on peripheral blood monocytes in systemic lupus erythematosus and rheumatoid arthritis. Rheumatology (Oxford). 2004;43:547–54.
Katayama K, Matsubara T, Fujiwara M. CD14+CD16+ monocyte subpopulation in Kawasaki disease. Clin Exp Immunol. 2000;121:566–70.
Okamoto H, Mizuno K, Horio T. Circulating CD14+ CD16+ monocytes are expanded in sarcoidosis patients. J Dermatol. 2003;30:503–9.
Schlitt A, Heine GH, Blankenberg S, Espinola-Klein C, Dopheide JF, Bickel C, Lackner KJ, Iz M, Meyer J, Darius H, Rupprecht HJ. CD14+CD16+ monocytes in coronary artery disease and their relationship to serum TNF-alpha levels. Thromb Haemost. 2004;92:419–24.
Zimmermann HW, Seidler S, Nattermann J. Functional contribution of elevated circulating and hepatic nonclassical CD14CD16 monocytes to inflammation and human liver fibrosis. PLoS ONE. 2010;5:e11049.
Kim HL, Chung GE, Park IY, Choi JM, Hwang SM, Lee JH, Kim D. Elevated peripheral blood monocyte fraction in nonalcoholic fatty liver disease. Tohoku J Exp Med. 2011;223:227–33.
Wang Y. A nonclassical monocyte phenotype in peripheral blood is associated with nonalcoholic fatty liver disease: a report from an EMIL subcohort. Horm Metab Res. 2016;48:54–61.
Farrell GC, Larter CZ. Nonalcoholic fatty liver disease: from steatosis to cirrhosis. Hepatology. 2006;43:S99–S112.
Nati M. The role of immune cells in metabolism-related liver inflammation and development of non-alcoholic steatohepatitis (NASH). Rev Endocr Metab Disord. 2016;17:29–39.
Stansfield BK, Ingram DA. Clinical significance of monocyte heterogeneity. Clin Transl Med. 2015;4:5.
Mukherjee R, Kanti Barman P, Kumar Thatoi P, Tripathy R, Kumar Das B, Ravindran B. Non-classical monocytes display inflammatory features: validation in sepsis and systemic lupus erythematous. Sci Rep. 2015;5:13886.
Yang J, Zhang L, Yu C, Yang XF, Wang H. Monocyte and macrophage differentiation: circulation inflammatory monocyte as biomarker for inflammatory diseases. Biomark Res. 2014;2:1.
Acknowledgements
This work was supported by grants from the National Natural Science Foundation of China (grant no. 81400828) and the Natural Science Foundation of Shandong Province (grant no. ZR2014HQ057).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
J. Zhang, W. Chen, L. Fang, Q. Li, X. Zhang, H. Zhang, Q. Guan, R. Zhao, C. Yang, and F. Jing declare that they have no competing interests.
Rights and permissions
About this article
Cite this article
Zhang, J., Chen, W., Fang, L. et al. Increased intermediate monocyte fraction in peripheral blood is associated with nonalcoholic fatty liver disease. Wien Klin Wochenschr 130, 390–397 (2018). https://doi.org/10.1007/s00508-018-1348-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00508-018-1348-6