Summary
Background
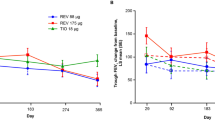
No specific (only subgroup) recommendations for the use of long-acting muscarinic antagonists in chronic obstructive pulmonary disease (COPD) exist. The aim of this exploratory hypothesis generating study was to assess whether different phenotypic/endotypic characteristics could be determinants of the short-term ineffectiveness of the initial tiotropium bromide monotherapy in treatment naïve moderate to severe COPD patients.
Methods
A total of 51 consecutively recruited COPD patients were followed for 3 months after the initial evaluation and prescribed initial treatment (tiotropium). Short-term treatment ineffectiveness was assessed as a composite measure comprising COPD exacerbations, need for additional treatment, and no improvement in functional parameters, e.g. 6‑min walking test (6MWT), body-mass index, airflow obstruction, dyspnea, and exercise (BODE) index and forced expiratory volume in 1 s (FEV1), and as single components.
Results
Treatment ineffectiveness was significantly associated with baseline hemoglobin level, COPD assessment test (CAT) score, modified Medical Research Council (mMRC) scale and BODE index (p = 0.002). Incident exacerbation during the follow-up was associated with baseline bronchoalveolar lavage fluid (BALF) alpha-amylase level and CAT score (p < 0.001), and change in treatment with leukocyte count, 6MWT desaturation and fatigue (p < 0.001). No improvement in 6MWT was associated with baseline CAT score, body mass index, mMRC, fatigue, 6MWT and BODE index (p = 0.002). No improvement in BODE index was associated with leukocyte count, serum interleukin 8 (IL-8) and BALF albumin levels (p < 0.001); and no improvement in FEV1 with CAT score, baseline vital capacity and BALF tumor necrosis factor alpha (TNF-alpha) level (p < 0.001).
Conclusion
Our results suggest that there is a possibility to identify predictors of short-term tiotropium ineffectiveness in patients with moderate to severe COPD.





Similar content being viewed by others
Abbreviations
- ACE:
-
Angiotensin-converting enzyme
- ALP:
-
Alkaline phosphatase
- AT1T:
-
Alpha1-antitrypsin
- ATS:
-
American Thoracic Society
- AUC:
-
Area under the curve
- BALF:
-
Bronchoalveolar lavage fluid
- BMI:
-
Body mass index
- BODE:
-
Body-mass index, airflow obstruction, dyspnea, and exercise
- CAT:
-
COPD assessment test
- CBC:
-
Complete blood cell
- CD:
-
Cluster of differentiation
- CI:
-
Confidence interval
- COPD:
-
Chronic obstructive pulmonary disease
- CRP:
-
C-reactive protein
- DLCO :
-
Diffusing capacity of the lungs for carbon monoxide
- ERS:
-
European Respiratory Society
- FAS:
-
Tilburg fatigue assessment scale
- FeNO:
-
Fraction of exhaled nitric oxide
- FEV1 :
-
Forced expiratory volume in 1 s
- FVC:
-
Forced vital capacity
- GCP:
-
Good clinical practice
- GOLD:
-
Global Initiative for Chronic Obstructive Lung Disease
- HRQoL:
-
Health related quality of life
- ICS:
-
Inhaled corticosteroids
- IL:
-
Interleukin
- LAMA:
-
Long-acting muscarinic antagonists
- LDH:
-
Lactate dehydrogenase
- mMRC:
-
Modified Medical Research Council
- NPV:
-
Negative predictive value
- OR:
-
Odds ratio
- PEF:
-
Peak expiratory flow
- pCO2:
-
Partial pressure of carbon dioxide
- pO2:
-
Partial pressure of oxygen
- PPV:
-
Positive predictive value
- RV:
-
Residual volume
- SD:
-
Standard deviation
- SpO2:
-
Arterial oxygen saturation
- 6MWT:
-
6 min walking test
- TGF-beta:
-
Transforming growth factor beta
- TLC:
-
Total lung capacity
- TNF-alpha:
-
Tumor necrosis factor alpha
References
Vestbo J, Hurd SS, Agustí AG, Jones PW, Vogelmeier C, Anzueto A, et al. Global strategy for the diagnosis, management and prevention of chronic obstructive pulmonary disease: GOLD executive summary. Am J Respir Crit Care Med. 2013;187:347–65.
Global Initiative for Chronic Obstructive Lung Disease (GOLD). 2016. http://www.goldcopd.org/. Accessed 22 May 2016.
Bestal JC, Paule A, Garrod R, Garnham R, Jones PW, Wedzicha JA. Usefulness of the research council (MRC) dyspnea scale as a measure of disability in patients with chronic obstructive pulmonary disease. Thorax. 1999;54:581–6.
Jones PW, Harding G, Berry P, Wiklund I, Chen WH, Kline Leidy N. Development and validation of the COPD assessment test. Eur Respir J. 2009;34:648–54.
Hogg JC. Pathophysiology of airflow limitation in chronic obstructive pulmonary disease. Lancet. 2004;364:709–21.
Stockley RA. Neutrophils and the pathogenesis of COPD. Chest. 2002;121(5 suppl):151S–5S.
Barnes PJ. Macrophages as orchestrators of COPD. COPD. 2004;1:59–70.
Hogg JC, Chu F, Utokaparch S, Woods R, Elliot WM, Buzatu L, et al. The nature of small-airway obstruction in chronic obstructive pulmonary disease. N Eng J Med. 2004;350:2645–53.
Bathoorne E, Liesker JJ, Postma DS, Koëter GH, van der Toorn M, van der Heide S, et al. Change in inflammation in out-patient COPD patients from stable to a subsequent exacerbation. Int J Chron Obstruct Pulmon Dis. 2009;4:101–9.
Barnes PJ. Mediators of chronic obstructive pulmonary disease. Pharmacol Rev. 2004;56:515–48.
Rachman I. Oxidative stress in pathogenesis of chronic obstructive pulmonary disease: cellular and molecular mechanisms. Cell Biochem Biophys. 2005;43:167–88.
Faganello MM, Tanni SE, Sanchez FF, Pelegrino NR, Luchet PA, Godoy I. BODE index and GOLD staging as predictors of 1‑year exacerbation risk in chronic obstructive pulmonary disease. Am J Med Sci. 2010;339:10–4.
Stockley RA, Mannino D, Barnes PJ. Burden and pathogenesis of chronic obstructive pulmonary disease. Proc Am Thorac Soc. 2009;6:524–6.
Keam SJ, Keating GM. Tiotropium bromide. A review of its use as maintenance therapy in patients with COPD. Treat Respir Med. 2004;3:247–68.
Canadian Thoracic Society/Canadian Respiratory Clinical Research Consortium, Aaron SD, Vandemheen KL, Fergusson D, Maltais F, Bourbeau J, Goldstein R, et al. Tiotropium in combination with placebo, salmeterol, or fluticasone-salmeterol for treatment of chronic obstructive pulmonary disease: a randomized trial. Ann Intern Med. 2007;146:545–55.
Disse B, Speck GA, Rominger KL, Witek TJ, Hammer R Jr.. Tiotropium (Spiriva): mechanistical considerations and clinical profile in obstructive pulmonary disease. Life Sci. 1999;64:457–64.
Tashkin D, Celli B, Kesten S, Lystic T, Decramer M. Effect of tiotropium in men and women with COPD: results of the 4‑year UPLIFT trial. Respir Med. 2010;104:1495–504.
Mamary Aj, Criner GJ. Tiotropium bromide for chronic obstructive pulmonary disease. Expert Rev Respir Med. 2009;3:211–20.
Zeiger RS, Szefler SJ, Phillips BR, Schatz M, Martinez FD, Chinchilli VM, et al. Childhood Asthma Research and Education Network of the National Heart, Lung, and Blood Institute. Response profiles to fluticasone and montelukast in mild-to-moderate persistent childhood asthma. J Allergy Clin Immunol. 2006;117:45–52.
Jones PW, Harding G, Berry P, Wiklund I, Chen WH, Kline Leidy N. Development and first validation of the COPD Assessment Test. Eur Respir J. 2009;34:648–54.
Michielsen HJ, de Vries J, van Heck GL. Psychometric qualities of a brief self-rated fatigue measure: the Fatigue Assessment Scale. J Psychosom Res. 2003;54:345–52.
Miller MR, Hankinson J, Brusasco V, Burgos F, Casaburi R, Coates A, et al. ATS/ERS Task Force. Standardisation of spirometry. Eur Respir J. 2005;26:319–38.
Quanjer PH, Tammeling GJ, Cotes JE, Pedersen OF, Peslin R, Yernault JC. Lung volumes and forced ventilatory flows. Report Working Party Standardization of Lung Function Tests, European Community for Steel and Coal. Official Statement of the European Respiratory Society. Eur Respir J. 1993;6(Suppl 16):5–40.
Macintyre N, Crapo RO, Viegi G, Johnson DC, van der Grinten CP, Brusasco V, et al. Standardization of the single-breath determination of carbon monoxide uptake in the lung. Eur Respir J. 2005;26:720–35.
American Thoracic Society, European Respiratory Society. ATS/ERS Recommendations for standardized procedures for online and offline measurement of exhaled lower respiratory and nasal nitric oxide. Am J Respir Crit Care Med. 2005;171:912–30.
ATS Committee on Proficiency Standards for Clinical Pulmonary Function Laboratories. ATS statement: guidelines for the six-minute walk test. Am J Respir Crit Care Med. 2002;166:111–7.
Haslam PL, Baughman RP. Report or ERS task force: guidelines for measurement of a cellular components and standardization of BAL. Eur Respir J. 1999;14:245–8.
Goossens LM, Leimer I, Metzdorf N, Becker K, Rutten-van Mölken MP. Does the 2013 GOLD classification improve the ability to predict lung function decline, exacerbations and mortality: a post-hoc analysis of the 4‑year UPLIFT trial. BMC Pulm Med. 2014;14:163.
Miravitlles M, García-Sidro P, Fernández-Nistal A, Buendía MJ, de los Monteros MJE, Esquinas C, et al. The chronic obstructive pulmonary disease assessment test improves the predictive value of previous exacerbations for poor outcomes in COPD. Int J Chron Obstruct Pulmon Dis. 2015;10:2571–9.
García-Sidro P, Naval E, Martinez Rivera C, Bonnin-Vilaplana M, Garcia-Rivero JL, Herrejón A, et al. The CAT (COPD Assessment Test) questionnaire as a predictor of the evolution of severe COPD exacerbations. Respir Med. 2015;109:1546–52.
Karloh M, Fleig Mayer A, Maurici R, Pizzichini MM, Jones PW, Pizzichini E. The COPD assessment test: what do we know so far?: a systematic review and meta-analysis about clinical outcomes prediction and classification of patients into GOLD stages. Chest. 2016;149:413–25.
Kim S, Oh J, Kim Y‑I, Ban H‑J, Kwon Y‑S, Oh I‑J, et al. Differences in classification of COPD group using COPD assessment test (CAT) or modified Medical Research Council (mMRC) dyspnea scores: a cross-sectional analyses. BMC Pulm Med. 2013;13:35.
Calverley PM, Celli B, Coxson HO, Edwards LD, Lomas DA, et al. Characterisation of COPB heterogeneity in the ECLIPSE cohort. Respir Res. 2010;11:122.
Andrianopoulos V, Wouters EFM, Pinto-Plata VM, Vanfleteren LEGW, Bakke PS, Franssen FME, et al. Prognostic value of variables derived from the six-minute walk test in patients with COPD: Results from the ECLIPSE study. Respir Med. 2015;109:1138–46.
Dal Negro RW, Tognella S, Bonadiman L, Turco P. Changes in blood hemoglobin and blood gases PaO2 and PaCO2 in severe COPD over a three-year telemonitored program of long-term oxygen treatment. Multidiscip Respir Med. 2012;7:15.
Hogg JC, Timens W. The pathology of chronic obstructive pulmonary disease. Annu Rev Pathol. 2009;4:435–59.
Grutters JC, Wuyts WA, Willems S, Demedts MG. Clinical use of biomarkers of survival in pulmonary fibrosis. Respir Res. 2010;11:89.
Dickens J, Miller B, Edwards L, Silverman E, Lomas D, Tal-Singer R. COPD association and repeatability of blood biomarkers in the ECLIPSE cohort. Respir Res. 2011;12:146.
Larsson K. Inflammatory markers in COPD. Clin Respir J. 2008;2(Suppl 1):84–7.
van Noord JA, Bantje TA, Eland ME, Korducki L, Cornelissen PJ. A randomised controlled comparison of tiotropium nd ipratropium in the treatment of chronic obstructive pulmonary disease. The Dutch Tiotropium Study Group. Thorax. 2000;55:289–94.
Donohue JF, Fogarty C, Lötvall J, Mahler DA, Worth H, Yorgancioglu A, et al. Once-daily bronchodilators for chronic obstructive pulmonary disease: indacaterol versus tiotropium. Am J Respir Crit Care Med. 2010;182:155–62.
Hohlfeld JM, Sharma A, van Noord JA, Cornelissen PJ, Derom E, Towse L, et al. Pharmacokinetics and pharmacodynamics of tiotropium solution and tiotropium powder in chronic obstructive pulmonary disease. J Clin Pharmacol. 2014;54(4):405–14.
Funding
No grant, equipment or drugs were received for this study.
Author contributions
V. Fijačko conceived the idea for the study, together with M. Labor, S. Škrinjarić-Cincar, S. Labor, T. Bačun, A. Včev and M. Fijačko collected data. D. Plavec and S. Popović-Grle were responsible together with V. Fijačko for the design of the research and for data analysis. I. Dumbović Dubravčić contributed by literature research, writing and editing the data. All authors contributed by editing and approving the final version of the manuscript. All authors have read and approved the final version of the manuscript.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
V. Fijačko has received honoraria for lectures from Novartis, Sandoz, AstraZeneca, Berlin Chemie, Pliva, and Boehringer Ingelheim. S. Škrinjarić-Cincar has received honoraria for lectures from Novartis, Sandoz, AstraZeneca, Berlin Chemie, Pliva, and Boehringer Ingelheim. S. Labor has received honoraria for lectures from Novartis, and Boehringer Ingelheim. T. Bačun has received honoraria for lectures from Novo Nordisk, Eli Lilly, Novartis, Sandoz, AstraZeneca, Berlin Chemie, Pliva, and Boehringer Ingelheim. S. Popović-Grle has received honoraria for advisory boards and/or lectures from Boehringer Ingelheim, Novartis, AstraZeneca, Pliva-Teva, Takeda, GlaxoSmithKline, Meda Pharma, Sanofi Aventis, Krka farma, Berlin Chemie Menarini Hrvatska, and Sandoz Hrvatska. D. Plavec has received research grants from GlaxoSmithKline, honoraria for advisory boards and/or lectures and/or clinical trials from GlaxoSmithKline, Menarini, Pliva, Boehringer Ingelheim, Belupo, AbbVie, MSD, and Chiesi. M. Labor, I. Dumbović Dubravčić, M. Fijačko and A. Včev declare that they have no competing interests.
Ethical standards
All studies on humans described in the present manuscript were carried out with the approval of the responsible ethics committee (Institutional Review Board and Medical Faculty Ethics Committee) and in accordance with national law and the Helsinki Declaration of 1975 (in its current, revised form). Informed consent was obtained from all patients included in the study.
Rights and permissions
About this article
Cite this article
Fijačko, V., Labor, M., Fijačko, M. et al. Predictors of short-term LAMA ineffectiveness in treatment naïve patients with moderate to severe COPD. Wien Klin Wochenschr 130, 247–258 (2018). https://doi.org/10.1007/s00508-017-1307-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00508-017-1307-7