Summary
Objective
To assess the association of indoor environmental risk factors with respiratory function among adults in an acid rain-plagued city in China where coal use is frequent.
Methods
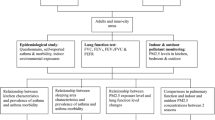
The subjects were randomly selected in the winter season. Information on selected home environmental factors was collected through administered questionnaires. Additionally, pulmonary function tests, including Forced Vital Capacity (FVC), Forced Expiratory Volume in 1 s (FEV1), FEV1/FVC and Peak Expiratory Flow Rate (PEFR) were also performed in participants.
Results
This study showed that, among a variety of risk factors, coal fuel use, cooking oil fumes and active and passive smoking exposure together with asthma in childhood were important factors for deterioration of pulmonary function among adults in the winter season (p < 0.05). Additionally, subjects whose kitchen was located in the living room or bedroom, who opened their windows only occasionally or never, who noted the presence of cooking oil fumes and pests, whose bedroom was shared by 3 or more residents and who kept pets tended to exhibit lower values of FVC, FEV1 and PEFR values compared with non-exposed counterparts (p < 0.05).
Conclusions
This study demonstrated impaired pulmonary function among adults who were exposed to indoor risk factors, such as coal fires and cigarette smoking compared to non-users in the winter season and emphasizes the need for public health efforts to decrease exposure to indoor air pollution.
Similar content being viewed by others
References
WHO Fuel for life. In: Household Energy and Health. New York: WHO; 2006.
Hersoug LG, Husemoen LL, Sigsgaard T, Madsen F, Linneberg A. Indoor exposure to environmental cigarette smoke, but not other inhaled particulates associates with respiratory symptoms and diminished lung function in adults. Respirology. 2010;15:993–1000.
Jie Y, Houjin H, Xun M, Kebin L, Xuesong Y, Jie X. Relationship of pulmonary function among adult residents to indoor air pollution from coal combustion in inner-city area of Southwest China. Braz J Med Biol Res. 2014;47(11):982–9.
Dottorini ML, Bruni B, Peccini F, Bottini P, Pini L, Donato F, Casucci G, Tantucci C. Skin prick-test reactivity to aeroallergens and allergic symptoms in an urban population of central Italy: a longitudinal study. Clin Exp Allergy. 2007;37(2):188–96.
Yu Jie IZM, Jie X, Ismai NH. Asthma and asthma-related symptoms among adults of an acid rain-plagued city in Southwest China: prevalence and risk factors. Pol J Environ Stud. 2013;22(3):717–26.
Yu J, Noor HI, Xu J, Zaleha MI. Do indoor environments influence asthma and asthma-related symptoms among adults in homes? A review of the literature. J Formos Med Assoc. 2011;110(9):555–63.
Ma Y, Chen R, Pan G, Xu X, Song W, Chen B, Kan H. Fine particulate air pollution and daily mortality in Shenyang, China. Sci Total Environ. 2011;409(13):2473–7.
Leitte AM, Schlink U, Herbarth O, Wiedensohler A, Pan XC, Hu M, Richter M, Wehner B, Tuch T, Wu Z, Yang M, Liu L, Breitner S, Cyrys J, Peters A, Wichmann HE, Franck U. Size-segregated particle number concentrations and respiratory emergency room visits in Beijing, China. Environ Health Perspect. 2011;119(4):508–13.
Jie Y, Houjin H, Xun M, Kebin L, Xuesong Y, Jie X. Relationship between pulmonary function and indoor air pollution from coal combustion among adult residents in an inner-city area of southwest China. Braz J Med Biol Res. 2014;47(11):982–9.
Lan Q, Mumford JL, Shen M, Demarini DM, Bonner MR, He X, Yeager M, Welch R, Chanock S, Tian L, Chapman RS, Zheng T, Keohavong P, Caporaso N, Rothman N. Oxidative damage-related genes AKR1C3 and OGG1 modulate risks for lung cancer due to exposure to PAH-rich coal combustion emissions. Carcinogenesis. 2004;25(11):2177–81.
Padhy PK, Padhi BK. Effects of biomass combustion smoke on hemato-logical and antioxidant profile among children (8–13 years) in India. Inhal Toxicol. 2009;21(8):705–11.
Saha A, Rao NM, Kulkarni PK, Majumdar PK, Saiyed HN. Pulmonary function and fuel use: a population survey. Respir Res. 2005;6:127.
Qian Z, He Q, Kong L, Xu F, Wei F, Chapman RS, Chen W, Edwards RD, Bascom R. Respiratory responses to diverse indoor combustion air pollution sources. Indoor Air. 2007;17(2):135–42.
Barry AC, Mannino DM, Hopenhayn C, Bush H. Exposure to indoor biomass fuel pollutants and asthma prevalence in Southeastern Kentucky: results from the Burden of Lung Disease (BOLD) study. J Asthma. 2010;47(7):735–41.
Shimada Y, Matsuoka Y. Analysis of indoor PM2.5 exposure in Asian countries using time use survey. Sci Total Environ. 2011;409(24):5243–52.
Diette GB, Accinelli RA, Balmes JR, Buist AS, Checkley W, Garbe P, Hansel NN, Kapil V, Gordon S, Lagat DK, Yip F, Mortimer K, Perez-Padilla R, Roth C, Schwaninger JM, Punturieri A, Kiley J. Obstructive lung disease and exposure to burning biomass fuel in the indoor environment. Glob Heart. 2012;7(3):265–70.
Mejza F, Nastałek P, Skucha W, Harat R, Niżankowska-Mogilnicka E. Effects of biomass combustion and occupational exposures on lung function in random population sample of Malopolska inhabitants. Pneumonol Alergol Pol. 2012;80(6):507–15.
Shen M, Chapman RS, Vermeulen R, Tian L, Zheng T, Chen BE, Engels EA, He X, Blair A, Lan Q. Coal use, stove improvement, and adult pneumonia mortality in Xuanwei, China: a retrospective cohort study. Environ Health Perspect. 2009;117(2):261–6.
Barone-Adesi F, Chapman RS, Silverman DT, He X, Hu W, Vermeulen R, Ning B, Fraumeni JF Jr, Rothman N, Lan Q. Risk of lung cancer associated with domestic use of coal in Xuanwei, China: retrospective cohort study. BMJ. 2012;345:e5414.
Constant C, Sampaio I, Negreiro F, Aguiar P, Silva A, Salgueiro M, Bandeira T. Environmental tobacco smoke (ETS) exposure and respiratory morbidity in school age children. Rev Port Pneumol. 2011;17(1):20–6.
Skogstad M, Kjaerheim K, Fladseth G, Gjølstad M, Daae HL, Olsen R, Molander P, Ellingsen DG. Cross shift changes in lung function among bar and restaurant workers before and after implementation of a smoking ban. Occup Environ Med. 2006;63(7):482–7.
Eisner MD, Wang Y, Haight TJ, Balmes J, Hammond SK, Tager IB. Secondhand smoke exposure, pulmonary function, and cardiovascular mortality. Ann Epidemiol. 2007;17(5):364–73.
Kunzli N, Schwartz J, Stutz EZ, Ackermann-Liebrich U, Leuenberger P. Association of environmental tobacco smoke at work and forced expiratory lung function among never smoking asthmatics and non-asthmatics. The SAPALDIA-Team. Swiss Study on Air Pollution and Lung Disease in Adults. Soz Praventivmed. 2000;45(5):208–17.
Janson C, Chinn S, Jarvis D, Zock JP, Toren K, Burney P. Effect of passive smoking on respiratory symptoms, bronchial responsiveness, lung function, and total serum IgE in the European Community Respiratory Health Survey: a cross-sectional study. Lancet. 2001;358(9299):2103–9.
Downs SH, Brändli O, Zellweger JP, Schindler C, Künzli N, Gerbase MW, Burdet L, Bettschart R, Zemp E, Frey M, Keller R, Tschopp JM, Leuenberger P, Ackermann-Liebrich U. Accelerated decline in lung function in smoking women with airway obstruction: SAPALDIA 2 cohort study. Respir Res. 2005;26(6):45.
Apostol GG, Jacobs DR, Tsai AW, Crow RS, Williams OD, Townsend MC, Beckett WS. Early life factors contribute to the decrease in lung function between ages 18 and 40: the Coronary Artery Risk Development in Young Adults study. Am J Respir Crit Care Med. 2002;166(2):166–72.
Thomson NC, Chaudhuri R. Asthma in smokers: challenges and opportunities. Curr Opin Pulm Med. 2009;15(1):39–45.
Svedahl S, Svendsen K, Qvenild T, Sjaastad AK, Hilt B. Short termexposure to cooking fumes and pulmonary function. J Occup Med Toxicol. 2009;4(4):9.
Adewole O, Desalu O, Nwogu K, Adewole T, Erhabor G. Respiratory symptoms and lung function patterns in workers exposed to wood smoke and cooking oil fumes (mai suya) in Nigeria. Ann Med Health Sci Res. 2013;3(1):38–42.
Naydenov K, Popov T, Mustakov T, Melikov A, Bornehag CG, Sundell J. The association of pet keeping at home with symptoms in airways, nose and skin among Bulgarian children. Pediatr Allergy Immunol. 2008;19(8):702–8.
Sunyer J, Soriano J, Antó JM, Burgos F, Pereira A, Payo F, Martínez-Moratalla J, Ramos J. Sensitization to individual allergens as risk factors for lower FEV1 in young adults. Int J Epidemiol. 2000;29(1):125–30.
Acknowledgements
This work was supported by the foundation of the National Natural Science Foundation of China (NO:2013-81360419), (NO:2015-81560527); Advanced Programs of Overseas Students Science and Technology Activities, Ministry of Human Resources and Social Security of the People’s Republic of China [2016] (176); the Key Technologies R&D Programme of the Department of Science and Technology of Guizhou Province, China (SY[2012]3126) and (SY[2013]3027).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
J. Yu, L. Zhang, Y. Luo, Y. Tang, F. Tuo, J. Yang and J. Xu declare that they have no competing interests.
Ethical standards
All studies on humans described in this manuscript were carried out with the approval of the responsible ethics committee and in accordance with national law and the Helsinki Declaration from 1964 (in its current revised form). Informed consent was obtained from all participants included in the study.
Additional information
Concern over the part of indoor air pollution in the damaging of human health has recently increased. Indoor environmental factors associated with pulmonary function is correlated with public health, hence we chose the “Wiener klinische Wochenschrift” for publication of the manuscript.
This study eventually concludes showing the impaired pulmonary function both in adult males and females who exposed to indoor risk factors such as coal and ETS use compared to non-users. Our study suggests that the deterioration of pulmonary function may be an important component of the public health burden of indoor air pollution. Issues of energy and IAP should therefore be considered in the formulation of policies and interventions aimed at reducing the respiratory disease burden in Zinyi City of China where domestic environmental risk exposure is common.
In the present study we performed for the first time a simultaneous evaluation of pulmonary function changes and magnitude of exposure in an adult population exposed to indoor environmental risk factors an acid rain-plagued city in China. There is few recent research published or presented at events on the same theme of the manuscript.
Yu Jie contributed to manuscript writing and investigation, Yang jiaqi, Luo Ya and Tang Yin contributed to epidemiological investigations, Zhang Longju, Tuo Fangxu contributed to language revision, Xu Jie contributed to study design.
Rights and permissions
About this article
Cite this article
Yu, J., Zhang, L., Luo, Y. et al. Indoor environmental factors associated with pulmonary function among adults in an acid rain-plagued city in Southwest China. Wien Klin Wochenschr 129, 259–268 (2017). https://doi.org/10.1007/s00508-016-1156-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00508-016-1156-9