Summary
Background
Despite a marked improvement in the overall prognosis of patients with type 1 diabetes mellitus (T1DM), cardiovascular morbidity/mortality is still increased. Since cellular and microvascular aberrations have been demonstrated already in children with T1DM, albeit a good glycemic control (CO), we hypothesized that early macrovascular changes can be detected by common carotid artery intima-media thickness (CCA-IMT).
Methods
We included 73 children/adolescents with T1DM (34 boys, 39 girls; mean age, 14.8 ± 2 years) and 243 sex- and age-matched healthy CO. In T1DM mean HbA1c was 7.9 ± 1.1 rel.%, and duration of disease 7.5 ± 3.1 years. High-resolution ultrasonography was used to assess CCA-IMT, defined as the mean of 24 measurements of the near and far wall on both right and left CCA.
Results
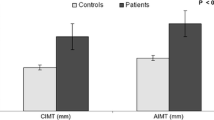
CCA-IMT was not different in the total of children and adolescents with T1DM compared with CO (0.302 ± 0.057 vs. 0.301 ± 0.054 mm; p = 0.88). Analysis according to gender, however, revealed higher CCA-IMT values in girls than in boys in the diabetic cohort (0.315 ± 0.055 vs. 0.288 ± 0.058 mm; p = 0.047), whereas CCA-IMT was higher in boys than in girls in the CO group (0.321 ± 0.057 vs. 0.284 ± 0.045 mm; p < 0.001). Multiple stepwise backward regression showed that in the T1DM group only HbA1c remained significantly associated with CCA-IMT (Beta = − 0.307, p = 0.008). In CO, gender (Beta = − 0.302, p < 0.001), body mass index (Beta = 0.226, p < 0.001) and systolic blood pressure (Beta = 0.213, p < 0.001) were predictive of CCA-IMT.
Conclusion
Our data suggest that in children/adolescents with T1DM the quality of metabolic CO (HbA1c) is the most important predictor of CCA-IMT and outweighs the effect of gender.
Zusammenfassung
Hintergrund
Trotz der besseren Allgemeinprognose von Patienten mit Diabetes Mellitus Typ 1 (T1DM) ist die kardiovaskuläre Morbidität/Mortalität noch hoch. Da bereits über zelluläre und mikrovaskuläre Veränderungen bei Kindern und Jugendlichen mit T1DM auch im Fall einer guten glykämischen Kontrolle berichtet wurde, haben wir angenommen, dass sehr frühe makrovaskuläre Veränderungen durch die Messung der Intima-Media-Dicke im Bereich der Arteria carotis communis (CCA-IMT) detektiert werden könnten.
Methoden
Eingeschlossen wurden 73 Kinder und Jugendliche mit T1DM (34 männlich, 39 weiblich; Durchschnittsalter 14,8 ± 2 Jahre) und 243 geschlechts- und altersgematchte gesunde Kontrollen (CO). Bei T1DM betrug der HbA1c-Mittelwert 7,9 ± 1,1 rel. % und die Krankheitsdauer 7,5 ± 3,1 Jahre. Die CCA-IMT wurde mittels Duplexsonographie ermittelt und als Mittelwert aus 24 Messungen im Bereich der anterioren und posterioren Wand der rechten und linken ACC definiert.
Ergebnisse
Wir fanden keinen signifikanten Unterschied in der CCA-IMT zwischen T1DM und CO Gruppe (0,302 ± 0,057 vs. 0,301 ± 0,054 mm; p = 0,88). In der geschlechtsbezogenen Subgruppenanalyse zeigte sich jedoch ein statistisch signifikanter Unterschied zwischen weiblichem und männlichem Kollektiv mit höheren IMT-Werten für Mädchen (0,315 ± 0,055 vs. 0,288 ± 0,058 mm; p = 0,047) in der T1DM Gruppe und höheren Werten für Jungen in der CO-Gruppe (0,321 ± 0,057 vs. 0,284 ± 0,045 mm; p < 0,001).
Nach multiplen rückwärts Regressionsanalysen zeigte in der T1DM Gruppe nur noch der HbA1c-Wert eine signifikante Assoziierung mit CCA-IMT (Beta = − 0,307, p = 0,008). In der CO Gruppe waren Geschlecht (Beta = − 0,302, p < 0,001), BMI (Beta = 0,226, p < 0,001) und systolischer Blutdruck (Beta = 0,213, p < 0,001) prädiktiv für CCA-IMT.
Schlussfolgerung
Unsere Ergebnisse suggerieren, dass in Kindern/Jugendlichen mit T1DM die Qualität der metabolischen Kontrolle (HbA1c) der wichtigste Prädiktor für CCA-IMT ist und auch die geschlechtsbezogenen Unterschiede aufheben kann.


Similar content being viewed by others
References
Nathan DM, Cleary PA, Backlund JY, et al. Diabetes Control and Complications Trial/Epidemiology of Diabetes Interventions and Complications (DCCT/EDIC) Study Research Group Intensive diabetes treatment and cardiovascular disease in patients with type 1 diabetes. N Engl J Med. 2005;353:2643–53.
Pambianco G, Costacou T, Ellis D, et al. The 30-year natural history of type 1 diabetes complications: the Pittsburgh Epidemiology of Diabetes Complications Study experience. Diabetes. 2006;55:1463–9.
Soedamah-Muthu SS, Fuller JH, Mulnier HE, et al. All-cause mortality rates in patients with type 1 diabetes mellitus compared with a non-diabetic population from the UK general practice research database, 1992–1999. Diabetologia. 2006;49:660–6.
Waernbaum I, Blohmé G, Ostman J, et al. Excess mortality in incident cases of diabetes mellitus aged 15–34 years at diagnosis: a population-based study (DISS) in Sweden. Diabetologia. 2006;49:653–9.
Secrest AM, Becker DJ, Kelsey SF, et al. All-cause mortality trends in a large population-based cohort with long-standing childhood-onset type 1 diabetes: the Allegheny County type 1 diabetes registry. Diabetes Care. 2010;33:2573–9.
Groop PH, Thomas MC, Moran JL, et al. FinnDiane Study Group. The presence and severity of chronic kidney disease predicts all-cause mortality in type 1 diabetes. Diabetes. 2009;58:1651–8.
Dogra G, Rich L, Stanton K, Watts GF. Endothelium-dependent and independent vasodilation studies at normoglycaemia in type I diabetes mellitus with and without microalbuminuria. Diabetologia. 2001;44:593–01.
Devaraj S, Cheung AT, Jialal I, et al. Evidence of increased inflammation and microcirculatory abnormalities in patients with type 1 diabetes and their role in microvascular complications. Diabetes. 2007;56:2790–6.
Lopes-Virella MF, Carter RE, Gilbert GE, et al. Diabetes Control and Complications Trial/Epidemiology of Diabetes Intervention and Complications Cohort Study Group. Risk factors related to inflammation and endothelial dysfunction in the DCCT/EDIC cohort and their relationship with nephropathy and macrovascular complications. Diabetes Care. 2008;31:2006–12.
Lin J, Glynn RJ, Rifai N, et al. Inflammation and progressive nephropathy in type 1 diabetes in the diabetes control and complications trial. Diabetes Care. 2008;31:2338–43.
Hörtenhuber T, Rami-Mehar B, Satler M, et al. Endothelial progenitor cells are related to glycemic control in children with type 1 diabetes mellitus over time. Diabetes Care. 2013;36:1647–53.
Schlager O, Hammer A, Willfort-Ehringer A, et al. Microvascular autoregulation in children and adolescents with type 1 diabetes mellitus. Diabetologia. 2012;55:1633–40.
Berger E, Sochett EB, Peirone A, et al. Cardiac and vascular function in adolescents and young adults with type 1 diabetes. Diabetes Technol Ther. 2004;6:129–35.
Lande MB, Carson NL, Roy J, et al. Effects of childhood primary hypertension on carotid intima media thickness: a matched controlled study. Hypertension. 2006;48:40–4.
Pauciullo P, Iannuzzi A, Sartorio R, et al. Increased intima-media thickness of the common carotid artery in hypercholesterolemic children. Arterioscler Thromb. 1994;14:1075–9.
Reinher T, Kiess W, de Sousa G, et al. Intima media thickness in childhood obesity: relations to inflammatory marker, glucose metabolism, and blood pressure. Metabolism. 2006;55:113–8.
Bonora E, Tessari R, Micciolo R, et al. Intimal-medial thickness of the carotid artery in nondiabetic and NIDDM patients. Relationship with insulin resistance. Diabetes Care. 1997;20:627–31.
Gunczler P, Lanes R, Lopez E, et al. Cardiac mass and function, carotid artery intima-media thickness and lipoprotein (a) levels in children and adolescents with type 1 diabetes mellitus of short duration. J Pediatr Endocrinol Metab. 2002;15:181–6.
Parikh A, Sochett EB, McCrindle BW, et al. Carotid artery distensibility and cardiac function in adolescents with type 1 diabetes. J Pediatr. 2000;137:465–9.
Järvisalo MJ, Putto-Laurila A, Jartti L, et al. Carotid artery intima-media thickness in children with type 1 diabetes. Diabetes. 2002;51:493–8.
World Medical Association Declaration of Helsinki. Recommendations guiding physicians in biomedical research involving human subjects. Helsinki, Finland, 1964; amended in Tokyo, Japan, 1975; Venice, Italy, 1983; Hong Kong 1989; Somerset West, South Africa, 1996; Edinburgh, Scotland, 2000; Washington, USA, 2002; Tokyo, Japan 2004; Seoul, Korea, 2008. http://www.wma.net/en/30publications/10policies/b3/ . http://ethikkommission.meduniwien.ac.at/fileadmin/ethik/media/dokumente/rechtsgrundlagen/Declaration_of_Helsinki_October_2008.pdf
American Academy of Pediatrics. American Academy of Pediatrics. Committee on Nutrition. Cholesterol in childhood. Pediatrics. 1998;101:141–7.
Neuhauser HK, Thamm M, Ellert U, et al. Blood pressure percentiles by age and height from nonoverweight children and adolescents in Germany. Pediatrics. 2011;127:978–88.
Kromeyer-Hauschild K, Wabitsch M, Kunze D, et al. Perzentile für den Body-mass-Index für das Kindes- und Jugendalter unter Heranziehung verschiedener deutscher Stichproben. Monatsschr Kinderheilkd. 2001;149:807–18.
Roman MJ, Naqvi TZ, Gardin JM, et al. American Society of Echocardiography; Society of Vascular Medicine and Biology. Clinical application of noninvasive vascular ultrasound in cardiovascular risk stratification: a report from the American Society of Echocardiography and the Society of Vascular Medicine and Biology. J Am Soc Echocardiogr. 2006;19:943–54.
Babar GS, Zidan H, Widlansky ME, et al. Impaired endothelial function in preadolescent children with type 1 diabetes. Diabetes Care. 2011;34:681–5.
Singh TP, Groehn H, Kazmers A. Vascular function and carotid intimal-medial thickness in children with insulin-dependent diabetes mellitus. J Am Coll Cardiol. 2003;41:661–5.
Peppa-Patrikiou M, Scordili M, Antoniou A, et al. Carotid atherosclerosis in adolescents and young adults with IDDM. Relation to urinary endothelin, albumin, free cortisol, and other factors. Diabetes Care. 1998;21:1004–7.
Schwab KO, Doerfer J, Krebs A, et al. Early atherosclerosis in childhood type 1 diabetes: role of raised systolic blood pressure in the absence of dyslipidaemia. Eur J Pediatr. 2007;166:541–8.
Krebs A, Schmidt-Trucksäss A, Doerfer J, et al. Cardiovascular risk in pediatric type 1 diabetes: sex-specific intima-media thickening verified by automatic contour identification and analyzing systems. Pediatr Diabetes. 2012;13:251–8.
Valerio G, Spagnuolo MI, Lombardi F, et al. Physical activity and sports participation in children and adolescents with type 1 diabetes mellitus. Nutr Metab Cardiovasc Dis. 2007;5:376–82.
Bryden KS, Neil A, Mayou RA, et al. Eating habits, body weight, and insulin misuse. A longitudinal study of teenagers and young adults with type 1 diabetes. Diabetes Care. 1999;12:1956–60.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Giurgea, GA., Nagl, K., Gschwandtner, M. et al. Gender, metabolic control and carotid intima-media-thickness in children and adolescents with type 1 diabetes mellitus. Wien Klin Wochenschr 127, 116–123 (2015). https://doi.org/10.1007/s00508-014-0640-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00508-014-0640-3