Summary
Background
The purpose is to present the Austrian data of an observational, cross-sectional, multicentre study conducted in 13 European countries. This study was undertaken to assess human papillomavirus (HPV) type distribution in high-grade cervical lesions.
Methods
Two hundred and ninety cases of high-grade cervical intraepithelial neoplasia (CIN2, CIN3) or adenocarcinoma in situ of the cervix from 2004 to 2007 were analysed by histopathological review and polymerase chain reaction for HPV.
Results
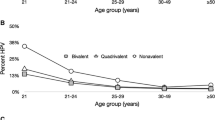
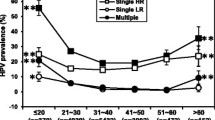
Two hundred and nine cases were “histologically eligible” and of those 206 were HPV+. Median age was 34 years (19–76 years). CIN3 was the most frequent diagnosis (64.6 %), followed by CIN2/3 (19.4 %) and CIN2 (13.6 %). Adenocarcinoma in situ was only detected together with a squamous lesion in 2.4 % cases. Majority of women (75.2 %) were infected with a single HPV type, 98.1 % of them with high-risk HPV types: HPV 16 (56.1 %), HPV 33 (12.3 %), HPV 31 (11.0 %), HPV 18 (3.9 %), HPV 35 (3.9 %), HPV 51 (3.2 %) and HPV 52 (2.6 %), HPV 58 (1.9 %) and HPV 45 (0.6 %). The low-risk HPV 6 was found in 1.3 % cases. Forty-six lesions (22.3 %) contained multiple infections, 71.1 % of those were HPV 16 or 18 and 91.1 % were HPV 16, 18, 31, 33 or 45 positive.
Conclusions
These Austrian data clearly demonstrate that HPV 16 is the predominant type in high-grade CIN, the immediate precursor lesions of cervical cancer. More than 60 % of the lesions were associated with HPV 16 and 18 and more than 85 % with HPV 16, 18, 31, 33 or 45. The prevalence of adenocarcinoma in situ is underestimated, since its detection is difficult with the current cytology screening.
Zusammenfassung
Grundlagen
Ziel dieser multizentrischen, in 13 europäischen Ländern durchgeführten Beobachtungsstudie ist die Erfassung der Typenverteilung von Humanen Papilloma Viren (HPV) in hochgradigen zervikalen Läsionen. Es werden die österreichischen Ergebnisse präsentiert.
Methodik
290 Fälle von hochgradigen zervikalen intraepithelialen Neoplasien (CIN2, CIN3) oder Adenocarcinoma in situ der Zervix wurden analysiert. Es wurden retrospektiv (von 2007–2004) zervikale Biopsiepräparate mit hochgradigen zervikalen Neoplasien sequentiell aus dem Archiv enthoben. Nach neuerlicher histopathologischer Prüfung erfolgte eine Testung auf HPV Desoxyribonucleinsäure mittels Polymerase Kettenreaktion.
Ergebnisse
209 Frauen bildeten die „histologisch auswertbare“ Kohorte, 206 waren HPV positiv. Das mittlere Alter war 34 Jahre (19–76). CIN3 war die häufigste histologische Diagnose (64,6 %), gefolgt von CIN2/3 (19,4 %) und CIN2 (13,6 %). Ein Adenocarcinoma in situ der Zervix wurde immer nur in Kombination mit einer hochgradigen Dysplasie diagnostiziert (2,4 %).
Die meisten Frauen waren mit einem HPV Typ infiziert (75,2 %), 98,1 % von diesen mit einem Hochrisiko-Typ: HPV 16 (56,1 %), HPV 33 (12,3 %), HPV 31 (11,0 %), HPV 18 (3,9 %), HPV 35 (3,9 %), HPV 51 (3,2 %) und HPV 52 (2,6 %), HPV 58 (1,9 %) und HPV 45 in 0,6 %. 46 Biopsate wiesen mehrere HPV Typen auf (22,3 %), 71,1 % davon HPV 16 oder 18 und 91,1 % HPV 16, 18, 31, 33 oder 45.
Schlussfolgerungen
HPV 16 ist der vorherrschende HPV Typ in hochgradigen zervikalen Neoplasien, der unmittelbaren Vorstufe des invasiven Zervixkarzinoms. Mehr als 60 % der Läsionen war mit HPV 16 und 18 assoziiert, mehr als 85 % mit HPV 16, 18, 31, 33 oder 45. Die Prävalenz des Adenocarcinoma in situ wird unterschätzt, da es mit den gängigen Screening Methoden schwer zu diagnostizieren ist.
Similar content being viewed by others
References
Schiffman M, Castle PE, Jeronimo J, Rodriguez AC, Wacholder S. Human papillomavirus and cervical cancer. Lancet. 2007;370:890–907.
Baseman JG, Koutsky LA. The epidemiology of human papillomavirus infections. J Clin Virol. 2005;32(Suppl 1):S16–24.
Parkin DM, Bray F, Ferlay J, Pisani P. Global cancer statistics, 2002. CA Cancer J Clin. 2005; 55:74–108.
Regauer S, Reich O. CK17 and p16 expression patterns distinguish (atypical) immature squamous metaplasia from high-grade cervical intraepithelial neoplasia (CIN III). Histopathology. 2007;50(5):629–35.
Reich O, Pickel H, Regauer S. Why does HPV infection induce sharply demarcated lesions of the cervix? J Low Genit Tract Dis. 2008;12:8–10.
Reich O, Pickel H. Multifocal stromal invasion in microinvasive squamous cell carcinoma of the cervix: how to measure and stage these lesions. Int J Gynecol Pathol. 2002;21:416–7.
Reich O, Pickel H, Tamussino K, Winter R. Microcarcinoma of the cervix: first focus of invasion. Obstet Gynecol. 2001;97:890–2.
McCredie MR, Sharples KJ, Paul C, et al. Natural history of cervical neoplasia and risk of invasive cancer in women with cervical intraepithelial neoplasia 3: a retrospective cohort study. Lancet Oncol. 2008;9(5):425–34.
Smith JS, Lindsay L, Hoots B, et al. Human papillomavirus type distribution in invasive cervical cancer and high-grade cervical lesions: a meta-analysis update. Int J Cancer. 2007;121:621–32.
Tjalma WA, Fiander A, Reich O, et al.; HERACLES/SCALE Study Group. Differences in human papillomavirus type distribution in high-grade cervical intraepithelial neoplasia and invasive cervical cancer in Europe. Int J Cancer. 2013;132(4):854–67.
Newcombe RG. Two-sided confidence intervals for the single proportion: comparison of seven methods. Stat Med. 1998;17(8):857–72.
Zechmeister I. Ökonomische Evaluation der Impfung gegen humane Papillomaviren (HPV- Impfung) in Österreich. Endbericht des Ludwig Boltzmann Instituts für Health Technology Assessment (LBI-HTA) 2007;26.
Leitner B. Statistik Austria, Jahrbuch der Gesundheitsstatistik 2010. Vienna: Statistik Austria; 2011.
Kyrgiou M, Koliopoulos G, Martin-Hirsch P, Arbyn M, Prendiville W, Paraskevaidis E. Obstetric outcomes after conservative treatment for intraepithelial or early invasive cervical lesions: systematic review and meta-analysis. Lancet. 2006;367(9509):489–98.
Arbyn M, Kyrgiou M, Simoens C, et al. Perinatal mortality and other severe adverse pregnancy outcomes associated with treatment of cervical intraepithelial neoplasia: meta-analysis. BMJ. 2008;337:a1284.
Van Hentenryck M, Noel JC, Simon P. Obstetric and neonatal outcome after surgical treatment of cervical dysplasia. Eur J Obstet Gynecol Reprod Biol. 2012;162(1):16–20.
Ortoft G, Henriksen T, Hansen E, Petersen L. After conisation of the cervix, the perinatal mortality as a result of preterm delivery increases in subsequent pregnancy. BJOG. 2010;117(3):258–67.
Six L, Leodolter S, Sings HL, Barr E, Haupt R, Joura EA. Prevalence of Human Papillomavirus Types 6, 11, 16, and 18 in young Austrian Women- the baseline data of a Phase III Vaccine Trial. Wien Klin Wochenschr. 2008;120(21–22):666–71.
Herzog TJ, Monk BJ. Reducing the burden of glandular carcinomas of the uterine cervix. Am J Obstet Gynecol. 2007;197(6):566–71.
Bray F, Carstensen B, Møller H, et al. Incidence trends of adenocarcinoma of the cervix in 13 European countries. Cancer Epidemiol Biomarkers Prev. 2005;14(9):2191–9.
Zielonke N. Krebsinzidenz und Krebsmortalität in Österreich 2012. Vienna: Statistik Austria; 2012.
Ault KA, Joura EA, Kjaer SK, et al.; FUTURE I and II Study Group. Adenocarcinoma in situ and associated human papillomavirus type distribution observed in two clinical trials of a quadrivalent human papillomavirus vaccine. Int J Cancer. 2011;128(6):1344–53.
Stoler MH, Vichnin MD, Ferenczy A, et al.; FUTURE I, II and III Investigators. The accuracy of colposcopic biopsy: analyses from the placebo arm of the Gardasil clinical trials. Int J Cancer. 2011;128(6):1354–62.
van Doorn LJ, Molijn A, Kleter B, Quint W, Colau B. Highly effective detection of human papillomavirus 16 and 18 DNA by a testing algorithm combining broad-spectrum and type-specific PCR. J Clin Microbiol. 2006;44:3292–8.
van Doorn LJ, Quint W, Kleter B, et al. Genotyping of human papillomavirus in liquid cytology cervical specimens by the PGMY line blot assay and the SPF(10) line probe assay. J Clin Microbiol. 2002;40:979–83.
Paavonen J, Naud P, Salmerón J, et al.; HPV PATRICIA Study Group. Efficacy of human papillomavirus (HPV)-16/18 AS04-adjuvanted vaccine against cervical infection and precancer caused by oncogenic HPV types (PATRICIA): final analysis of a double-blind, randomised study in young women. Lancet. 2009;374(9686):301–14.
Lehtinen M, Paavonen J, Wheeler CM, et al.; HPV PATRICIA Study Group. Overall efficacy of HPV-16/18 AS04-adjuvanted vaccine against grade 3 or greater cervical intraepithelial neoplasia: 4-year end-of-study analysis of the randomised, double-blind PATRICIA trial. Lancet Oncol. 2012;13(1):89–99.
FUTURE II Study Group. Quadrivalent vaccine against human papillomavirus to prevent high-grade cervical lesions. N Engl J Med. 2007;356:1915–27.
Joura EA, Leodolter S, Hernandez-Avila M, et al. Efficacy of a quadrivalent prophylactic human papillomavirus (types 6, 11, 16 and 18) L1 virus-like-particle vaccine against high-grade vulval and vaginal lesions: a combined analysis of three clinical trials. Lancet. 2007;369:1693–702.
Joura EA, Garland SM, Paavonen J, et al.; FUTURE I and II Study Group. Effect of the human papillomavirus (HPV) quadrivalent vaccine in a subgroup of women with cervical and vulvar disease: retrospective pooled analysis of trial data. BMJ. 2012;27(344):e1401.
Brown DR, Kjaer SK, Sigurdsson K, et al. The impact of quadrivalent human papillomavirus (HPV; types 6, 11, 16, and 18) L1 virus-like particle vaccine on infection and disease due to oncogenic nonvaccine HPV types in generally HPV-naive women aged 16–26 years. J Infect Dis. 2009;199(7):926–35.
Wheeler CM, Castellsagué X, Garland SM, et al. HPV PATRICIA Study Group. Cross-protective efficacy of HPV-16/18 AS04-adjuvanted vaccine against cervical infection and precancer caused by non-vaccine oncogenic HPV types: 4-year end-of-study analysis of the randomised, double-blind PATRICIA trial. Lancet Oncol. 2012;13(1):100–10.
Malagón T, Drolet M, Boily MC, et al. Cross-protective efficacy of two human papillomavirus vaccines: a systematic review and meta-analysis. Lancet Infect Dis. 2012;12(10):781–9.
Canfell K, Chesson H, Kulasingam SL, Berkhof J, Diaz M, Kim JJ. Modeling preventative strategies against human papillomavirus-related disease in developed countries. Vaccine. 2012;30 Suppl 5:F157–67.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Rössler, L., Reich, O., Horvat, R. et al. Human papillomavirus in high-grade cervical lesions: Austrian data of a European multicentre study. Wien Klin Wochenschr 125, 591–599 (2013). https://doi.org/10.1007/s00508-013-0403-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00508-013-0403-6