Summary
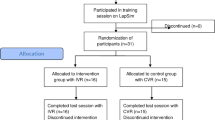
It is well known that learning curves are longer for laparoscopic surgery compared to open surgery. Recently, virtual reality (VR) simulation was developed as alternative to conventional training. Such a new training system makes it possible to offer a wide range of repeatable surgical situations, and thus, enable assessments based on direct observation of performance. During the last four years we did several studies using a VR simulator (LapSim®). After a constructive validity study – discrimination between novices and experienced laparoscopic surgeons, we were able to show that advanced residents benefit most from a three-day practical course for laparoscopic surgery, while – in a further investigation – we found contrary to training at the Pelvitrainer that novices in laparoscopic surgery have the most benefit from VR training. Minimally invasive surgery is significantly more sophisticated for the surgeon than open surgery. While Research on laparoscopic surgery has focused primarily on the development and assessment of technical skills, non technical skills such as visual-spatial perception and stress coping has received much less attention. We showed that spatial perception as well as stress coping positively correlates with virtual laparoscopic skills. A high degree of spatial perception led to faster adaption to a non-stereo environment and correlated with high level of laparoscopic skills. Furthermore, Ineffective stress-coping strategies correlate with poor virtual laparoscopic performance. VR simulation seems to be a promising tool to improve laparoscopic skills in a modern apprenticeship model. According to patient safety, the development of this instrument for surgery should be advanced professionally just as a flight simulators in aviation.
Zusammenfassung
Bei laparoskopischen Operationen bestehen längere Lernkurven als bei konventionellen Operationen. In den letzten Jahren wurden als Alternative zum herkömmlichen Training, virtuelle Operations-Simulatoren entwickelt. Diese gestatten das Üben in einer computergenerierten Umgebung und erlauben das gezielte Training von technischen Fähigkeiten in frei wählbaren Szenarien. In den letzten vier Jahren wurde an der chirurgischen Universitätsklinik Marburg mit Hilfe des Laparoskopiesimulators (LapSim®) eine Reihe von Untersuchungen durchgeführt. Nach initialer Validierung des Simulators "Abbildung laparoskopischer Fertigkeiten von laparoskopisch erfahrenen und weniger erfahrenen Ärzten" konnte der Lernerfolg nach einem praktischen Laparoskopiekurs am Pelvitrainer gemessen und damit die Zielgruppe des Kurses ermittelt werden. In einem weiteren Untersuchungskomplex fanden wir im Gegensatz zu dem Training am Pelvitrainer, dass gerade die Anfänger den höchsten Lernerfolg am Simulator haben. Da die laparoskopischen Operationen besondere Anforderungen an den Chirurgen stellen, gewinnen neben der manuellen Geschicklichkeit auf hohem Niveau auch individuelle Faktoren wie z.B. räumliche Orientierung und Stressverarbeitungsstrategien also sogenannte "non-technical-skills" für die Eignung als laparoskopischer Chirurg zunehmend an Bedeutung. So konnte in weiteren Untersuchungen gezeigt werden, dass das räumliche Denken sowie eine gute Stressverarbeitung positiv mit virtuellen laparoskopischen Fähigkeiten korrelieren. Probanden mit hohem Maß an räumlichem Denkvermögen verfügen über bessere virtuelle laparoskopische Fertigkeit als die Probanden mit geringerem räumlichen Denkvermögen. Des weiteren haben Probanden, die inadäquate Stressbewältigungsstategien besitzen, komplexe Aufgaben am Simulator schlechter durchgeführt als Probanden mit adäquaten Stressbewältigungsstategien. Die virtuelle Laparoskopie ist ein viel versprechendes Werkzeug in der chirurgischen Weiterbildung. Im Interesse des Patienten sollte die Entwicklung dieses Instrumentes in der Chirurgie ebenso professionell vorangetrieben werden wie jene von Flugsimulatoren in der Luftfahrt.
Similar content being viewed by others
Literatur
Ahlberg G, Heikkinen T, Iselius L, et al (2002) Does training in a virtual reality simulator improve surgical performance? Surg Endosc 16: 126–129
Ali MR, Mowery Y, Kaplan B, et al (2002) Training the novice in laparoscopy: more challenge is better. Surg Endosc 16: 1732–1736
Ayodeji ID, Schijven MP, Jakimowicz JJ (2006) Determination of face validity for the Simbionix LAP mentor virtual reality training module. Stud Health Technol Inform 119: 28–30
Bogner M (Hrsg) (1994) Human error in medicine. LEA, Hillsdale
Bogner M (Hrsg) (2004) Misadventures in health care. LEA, Mahwah
Brunner WC, Korndorffer JR Jr, Sierra R, Massarweh NN, Dunne JB, Yau CL, Scott DJ (2004) Laparoscopic virtual reality training: are 30 repetitions enough? J Surg Res 122 (2): 150–156
Clerici T, Lange J, Zerz A, Beller S, Szinicz G, Losert UO, Siegl H, Függer R (1995) Educational opportunities in minimally invasive surgery. Wien Klin Wochenschr 107 (2): 43–48
Duffy AJ, Hogle NJ, McCarthy H, Lew JI, Egan A, Christos P, Fowler DL (2005) Construct validity for the LAPSIM laparoscopic surgical simulator. Surg Endosc 19 (3): 401–405
Freeman ML, Nelson DB, Sherman S, Haber GB, Herman ME, Dorsher PJ (1996) Complications of endoscopic biliary sphincterotomy. N Engl J Med 26: 909–918
Gallagher AG, Satava RM (2002) Virtual reality as a metric for the assessment of laparoscopic psychomotor skills. Learning curves and reliability measures. Surg Endosc 16 (12): 1746–1752
Gallagher AG, Lederman AB, McGlade K, Satava RM, Smith CD (2004) Discriminative validity of the Minimally Invasive Surgical Trainer in Virtual Reality (MIST-VR) using criteria levels based on expert performance. Surg Endosc 18 (4): 660–665
Gerdes B, Hassan I, Maschuw K, Schlosser K, Bartholomaus J, Neubert T, Schwedhelm B, Petrikowski-Schneider I, Wissner W, Schonert M, Rothmund M (2006) Instituting a surgical skills lab at a training hospital. Chirurg 77 (11): 1033–1039
Goeters KM (Hrsg) (2004) Aviation psychology: practice and research. Ashgate, Aldershot
Grantcharov TP, Carstensen L, Schulze S (2005) Objective assessment of gastrointestinal endoscopy skills using a virtual reality simulator. JSLS 9 (2): 130–133
Grantcharov TP, Kristiansen VB, Bendix J, et al (2004) Randomized clinical trial of virtual reality simulation for laparoscopic skills training. Br J Surg 91: 146–150
Grantcharov TP, Bardram L, Funch-Jensen P, Rosenberg J (2003) Learning curves and impact of previous operative experience on performance on a virtual reality simulator to test laparoscopic surgical skills. Am J Surg 185 (2): 146–149
Hassan I, Gerdes B, Koller M, Langer P, Rothmund M, Zielke A (2006) Clinical background is required for optimum performance with a VR laparoscopy simulator. Computer Aided Surg 11 (2): 103–106
Hassan I, Koller M, Dick B, Rothmund M, Zielke A. Spatial perception predicts laparoscopic skills on a virtual reality laparoscopy simulator. Child Nervous System (in Druck)
Hassan I, Koller M, Zielke A, Lehmann K, Rothmund M, Gerdes B (2006) Improvement of surgical skills after a three-day practical course for laparoscopic surgery. Swiss Med Wkly 136 (39–40): 631–636
Hassan I, Maschuw K, Rothmund M, Gerdes B (2006) Novices in surgery are the target group of a virtual reality training laboratory. Eur Surg Res 38 (2): 109–113
Hassan I, Sitter H, Schlosser K, Zielke A, Rothmund M, Gerdes B (2005) A virtual reality simulator for objective assessment of surgeons' laparoscopic skills. Chirurg 76 (2): 151–156
Hassan I, Weyers P, Dick B, Gerdes B, Rothmund M, Zielke A (2006) Negative stress coping strategies among novices predict poor virtual laparoscopic performance. Br J Surg 93 (12): 1554–1559
Hyltander A, Liljegren E, Rhodin PH, et al (2002) The transfer of basic skills learned in a laparoscopic simulator to the operating room. Surg Endosc 16: 1324–1328
Janke W, Erdmann G, Kallus KW (2002) Stressverarbeitungsfragebogen SVF mit SVF 120 und SVF 78. Hogrefe, Göttingen
Lehmann KS, Ritz JP, Maass H, et al (2005) A prospective randomized study to test the transfer of basic psychomotor skills from virtual reality to physical reality in a comparable training setting. Ann Surg 241: 442–449
McClusky DA 3rd, Ritter EM, Lederman AB, Gallagher AG, Smith CD (2005) Correlation between perceptual, visuo-spatial, and psychomotor aptitude to duration of training required to reach performance goals on the MIST-VR surgical simulator. Am Surg 71 (1): 13–21
Moran MR (1997) The learning curve for laparoscopic colorectel surgery. Arch Surg 132 (8): 931–932
Paisley AM, Baldwin PJ, Paterson-Brown S (2001) Validity of surgical simulation for the assessment of operative skill. Br J Surg 88: 1525–1532
Pressmar SB, Haase W (2001) Effects on depth perception and pattern recognition in random dot stereograms by changing the matrix dot density. Ophthalmologe 98 (10): 955–959
Ro CY, Toumpoulis IK, Ashton RC Jr, Jebara T, Schulman C, Todd GJ, Derose JJ Jr, McGinty JJ (2005) The LapSim: a learning environment for both experts and novices. Stud Health Technol Inform 111: 414–417
Schijven M, Jakimowicz J (2003) Construct validity: experts and novices performing on the Xitact LS500 laparoscopy simulator. Surg Endosc 17 (5): 803–810
Schlachta CM, Mamazza J, Seshadri PA (2001) Defining a learning curve for laparoscopic colorectal resections. Dis Colon Rectum 44: 217–222
Schlosser K, Alkhawaga M, Gerdes B, Hassan I. Training of laparoscopic skills with virtual reality simulator: a critical reappraisal of the learning curve. Eur Surg (in Druck)
Scott J, Soot NE, Mehrdad F (1996) Transition from open to laparoscopic fundoplication – the learning curve. Arch Surg 134: 278–281
Seymour NE, Gallagher AG, Roman SA, et al (2002) Virtual reality training improves operating room performance results of a randomized, double-blinded study. Ann Surg 236: 458–464
Shah J, Buckley D, Frisby J, Darzi A (2003) Depth cue reliance in surgeons and medical students. Surg Endosc 17 (9): 1472–1474
Simons AJ (1995) Laparoscopic-assisted colectomy, learning curve. Dis Colon Rectum 38 (6): 600–603
Torkington J, Smith SG, Rees B, Darzi A (2001) The role of the basic surgical skills course in the acquisition and retention of laparoscopic skill. Surg Endosc 15 (10): 1071–1075
Stumpf H, Fay E (1983) Schlauchfiguren – Ein Test zur Beurteilung des räumlichen Vorstellungsvermögens. Verlag für Psychologie, Hogrefe, Göttingen Toronto Zürich
Torkington J, Smith SG, Rees B, Darzi A (2001) The role of the basic surgical skills course in the acquisition and retention of laparoscopic skill. Surg Endosc 15 (10): 1071–1075
Verdaasdonk EG, Stassen LP, Monteny LJ, Dankelman J (2006) Validation of a new basic virtual reality simulator for training of basic endoscopic skills: the SIMENDO. Surg Endosc 20 (3): 511–518
Voitk AJ, Tsao SG, Ignatius S (2001) The tail of the learning curve for laparoscopic cholecystectomy. Am J Surg 182: 250–253
Watson DI, Baigrie RJ, Jamieson GG (1996) A learning curve for laparoscopic fundoplication. Definable, avoidable, or a waste of time? Ann Surg 224: 198–203
Woodrum DT, Andreatta PB, Yellamanchilli RK, Feryus L, Gauger PG, Minter RM (2006) Construct validity of the LapSim laparoscopic surgical simulator. Am J Surg 191 (1): 28–32
Youngblood PL, Srivastava S, Curet M (2005) Comparison of training on two laparoscopic simulators and assessment of skills transfer to surgical performance. J Am Coll Surg 200: 564–551
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Hassan, I., Osei-Agymang, T., Radu, D. et al. Simulation endoskopischer Operationen – Vier Jahre Erfahrung an der Chirurgischen Universitätsklinik Marburg. Wien Klin Wochenschr 120, 70–76 (2008). https://doi.org/10.1007/s00508-008-0930-8
Received:
Accepted:
Issue Date:
DOI: https://doi.org/10.1007/s00508-008-0930-8