Abstract
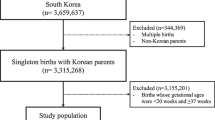
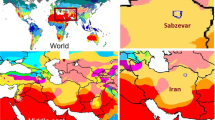
Research on the impact of heat on pregnant women has focused largely on outcomes following extreme temperature events, such as particular heat waves or spells of very cold weather on pregnant women. Consistently, the literature has shown a statistically significant relationship between heat with shortened gestational age with studies concentrated largely in the western states of the USA or other nations. The association between heat and shortened gestational age has not been examined in the Southeastern US where maternal outcomes are some of the most challenging in the nation. Unlike previous studies that focus on the impacts of a single heat wave event, this study seeks to understand the impact of high heat over a 5-year period during the annual warm season (May–September). To achieve this goal, a case-crossover study design is employed to understand the impact of heat on preterm labor across regions in North Carolina (NC). Temperature thresholds for impact and the underlying relationships between preterm labor and heat are investigated using generalized additive models (GAM). Gridded temperature data (PRISM) is used to establish exposure classifications. The results reveal significant impacts to pregnant women exposed to heat with regional variations. The exposure variable with the most stable and significant result was minimum temperature, indicating high overnight temperatures have the most impact on preterm birth. The magnitude of this impact varies across regions from a 1% increase in risk to 6% increase in risk per two-degree increment above established minimum temperature thresholds.



Similar content being viewed by others
References
Alberini A, Gans W, Alhassan M (2011) Individual and public-program adaptation: coping with heat waves in five cities in Canada. Int J Environ Res Public Health 8:4679–4701
Auger N, Gamache P, Adam-Smith J, Harper S (2011) Relative and absolute disparities in preterm birth related to neighborhood education. Ann Epidemiol 21(7):481–488
Auger N, Naimi A, Smargiassi A, Lo E, Kosatsky T (2014) Extreme heat and risk of early delivery among preterm and term pregnancies. Epidemiology. 24(3):344–350
Avalos L, Chen H, De-Kun L, Basu R (2017) The impact of high ambient temperature on spontaneous preterm delivery: a case-crossover study. Environ Health 16(5). https://doi.org/10.1186/s12940-017-0205-5
Balbus JM, Malina C (2009) Identifying vulnerable subpopulations for climate change health effects in the United States. J Occup Environ Med 51:33–37
Bassil K, Cole D (2010) Effectiveness of public health interventions in reducing morbidity and mortality during heat episodes: a structured review. Int J Environ Res Public Health 7:991–1001
Basu R, Malig B, Ostro B (2010) High ambient temperature and the risk of preterm delivery. Am J Epidemiol 172(10):1108–1117. https://doi.org/10.1093/aje/kwq170
Basu R, Pearson D, Broadwin R (2015) A case-crossover study of temperature and infant mortality in California. Pediatr Perinat Epidemiol 29:407–415
Basu R, Chen H, Li D, Avalos L (2017) The impact of maternal factors on the association between temperature and preterm delivery. Environ Res 154:109–114
Beck R, Malig B, Ostrol B (2010) The worldwide incidence of preterm birth: a systematic review of maternal mortality and morbidity. Bull World Health Organ 88:31–38
Benmarhina T, Auger N, Stanislas V, Lo E, Kaufman J (2015) The relationship between apparent temperature and daily number of live births in Montreal. Matern Child Health J 19:2548–2551
Berkowitz GS, Papiernick E (1993) Epidemiology of preterm birth. Epidemiol Rev 15(2):414–443
Carolan-Olah M, Frankowska D (2014) High environmental temperature and preterm birth: a review of the evidence. Midwifery. 30:50–59
Cox B, Vicedo-Cabrera A, Gasparrini A, Roels H, Martens E, Vangronsveld J, Forsberg B, Nawrot T (2016) Ambient temperature as a trigger of preterm delivery in a temperate climate. J Epidemiol Community Health 70:1191–1199
Dadvand P, Basagana X, Sartini C, Figueras F, Vrijheid M, de Nazelle A, Sunyer J, Nieuwenhuijsen M (2011) Climate extremes and the length of gestation. Environ Health Perspect 119(10):1449–1452
Daly C, Halbleib M, Smith JI, Gibson WP, Doggett MK, Taylor GH, Curtis J, Pasteris PP (2008) Physiographically sensitive mapping of climatological temperature and precipitation across the conterminous United States. Int J Climatol 28(15):2031–2064. https://doi.org/10.1002/joc.1688
Ebi K, Teisberg T, Kalkstein L, Robinson L, Weiher R (2004) Heat watch/warning systems save lives. Bull Am Meteorol Soc 85:1067–1073
Ebi K, Kovats S, Menne B (2006) An approach for assessing human health vulnerability and public health interventions to adapt to climate change. Environ Health Perspect 114(12):1930–1934
Fisher, Sheehan, Colton (2016) Home energy affordability gap. Public Finance and General Economics, Belmont, Massachusetts
Frich P, Alexander LV, Della-Marta P, Gleason B, Haylock M, Klein Tank AMG, Peterson T (2002) Observed coherent changes in climatic extremes during the second half of the twentieth century. Climate Research. 19(3):193–212
Ha S, Liu D, Zhu Y, Kim S, Sherman S, Mendola P (2017) Ambient temperature and early delivery of singleton pregnancies. Environ Health Perspect 125(3):453–459
He, J., Liu, Y., Xia, X., Ma., W., Lin, H., Kan, H., Lu, J., Feng, Q., Mo, W., Wang, P., Xia, H., Qiu, X., Muglia, L. (2016). Ambient temperature and the risk of preterm birth in Guangzhou, China (2001-2011). Environ Health Perspect 124(7), 1100–1106
Janes H, Sheppard L, Lumley T (2005) Case-crossover analysis of air pollution exposure data: referent selection strategies and their implications for bias. Epidemiology. 16(6):717–726
Klebanoff MA, Keim SA (2011) Epidemiology: the changing face of preterm birth. Clin Perinatol 38:339–350
Kovach M, Konrad C, Fuhrmann C (2015) Area-level risk factors for heat-related illness in rural and urban locations across North Carolina, USA. Appl Geogr 60:175–183
Lajinian S, Hudson S, Applewhite L, Feldman J, Minkoff H (1997) An association between the heat-humidity index and preterm labor and delivery: a preliminary analysis. Am J Public Health 87(7):1205–1207
Li C, West-Strum D (2010) Patient panel of underserved populations and adoption of electronic medical record systems by office–based physicians. Health Services Research. 4:963–84
Lippman S, Fuhrmann C, Waller A, Richardson D (2013) Ambient temperature and emergency department visits for heat-related illness in North Carolina, 2007-2008. Environ Res 124:35–42
Lumley J (2003) Defining the problem: the epidemiology of preterm birth. BJOG: Int J Obstet Gynecol 110:3–7
Maclure M (2017) The case-crossover design: a method for studying transient effects on the risk of acute events. Am J Epidemiol 185(11):1174–1183
Matthew S, Mathur D, Chang A, McDonald E, Singh G, Nur D, Gerristen R (2017) Examining the effects of ambient temperature on pre-term birth in Central Australia. Environ Res Public Health 14(147)
Moss TJM (2006) Respiratory consequences of preterm birth. Clin Exp Pharmacol Physiol 33:280–284
Platt RW, Joseph KS, Ananth CV, Grondines J, Abrahamowicz M, Kramer MS (2004) A proportional hazards model with time-dependent covariates and time-varying effects for analysis of fetal and infant death. Am J Epidemiol 160(3):199–206
PRISM Climate Group, Oregon State University, http://prism.oregonstate.edu, created 11 Jul 2012
Sayres WG Jr (2010) Preterm labor. Am Fam Physician 81:477–484
Schifano P, Lallo A, Asta F, De Sario M, Davoli M, Michelozzi P (2013) Effect of ambient temperature and air pollutants on the risk of perterm birth, Rome 2001-2010. Environ Int 61:77–87
Schoen, C., Tabbah, S., Iams, J., Caughey, A., Berghella, V. (2015). Why the United States preterm birth rate is declining. American Journal of Obstetrics and Gynecology. 185-180
Social Explorer; U.S. Census Bureau; (2016) ACS 1-year and 2012–2016 ACS 5-year Data Releases: Technical Documentation
Strand LB, Barnett AG, Tong S (2012) Maternal exposure to ambient temperature and the risks of preterm birth and stillbirth in Brisbane, Australia. Am J Epidemiol 175:99–107
United States Department of Health and Human Services (US DHHS), Centers for Disease Control and Prevention (CDC), National Center for Health Statistics (NCHS),2018 Division of Vital Statistics, Natality public-use data on CDC WONDER Online Database, for years 2007–2016 available February 2018
Wang J, Williams G, Guo Y, Pan X, Tong S (2013) Maternal exposure to heatwave and preterm birth in Brisbane, Australia. BJOG 120:1631–1641
Weinick RM, Byron SC, Bierman AS, (2005) Who can’t pay for health care? Journal of General Internal Medicine. 20(6):504–509
Wood SN, Pya N, Säfken B (2016) Smoothing parameter and model selection for general smooth models. J Am Stat Assoc 111(516):1548–1563
Woods SN (2011) Fast stable restricted maximum likelihood and marginal likelihood estimation of semiparametric generalized linear models. J R Stat Soc Ser B (Statistical Methodology) 73(1):3–36
xmACIS: Applied Climate Information System (2018). NOAA Regional Climate Centers. http://xmacis.rcc-acis.org. Retrieved 2018
Acknowledgments
The authors would like to acknowledge Jess Rinsky, PhD, MPH, Epidemiologist, Division of Public Health, Occupational and Environmental Epidemiology Branch, NC Department of Health and Human Services for her consultation and guidance on this project.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
CISA is a pilot program of the NOAA National Integrated Heat Health Information System (NIHHIS).
Rights and permissions
About this article
Cite this article
Ward, A., Clark, J., McLeod, J. et al. The impact of heat exposure on reduced gestational age in pregnant women in North Carolina, 2011–2015. Int J Biometeorol 63, 1611–1620 (2019). https://doi.org/10.1007/s00484-019-01773-3
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00484-019-01773-3