Abstract
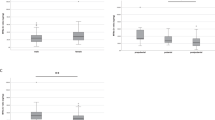
During the past several decades, obesity has been increasing globally. In Japan, obesity is defined by a BMI of 25 kg/m2 or over; 28.6 % of men and 20.6 % of women are obese. Obese people have an increased incidence of developing cardiovascular, renal, and hormonal diseases and sleep disorders. Obese people also have shortened sleep durations. We investigated seasonal differences in melatonin concentrations, heart rates, and heart rate variability during sleep in obese subjects in Japan. Five obese (BMI, 32.0 ± 4.9 kg/m2) and five non-obese (BMI, 23.2 ± 2.9 kg/m2) men participated in this study in the summer and winter. Electrocardiograms were measured continuously overnight in a climatic chamber at 26 °C with a relative humidity of 50 %. Saliva samples for melatonin were collected at 2300 hours, 0200 hours, and 0600 hours. We found that melatonin concentrations during sleep in obese subjects were significantly lower than those in non-obese subjects in the winter. Heart rate during sleep in winter was significantly higher than that in summer in both obese and non-obese subjects. Heart rate variability was not significantly different in the summer and winter in both obese and non-obese subjects. Our results show that decreased nocturnal melatonin concentrations during winter in obese men may be related to higher heart rates, and this may suggest that obese men are at an increased risk of a cardiovascular incident during sleep, especially in the winter.


Similar content being viewed by others
References
Adachi T, Sert-Kuniyoshi FH, Calvin AD, Singh P, Romero-Corral A, van der Walt C, Davison DE, Bukartyk J, Konecny T, Pusalavidyasagar S, Sierra-Johnson J, Somers VK (2011) Effect of weight gain on cardiac autonomic control during wakefulness and sleep. Hypertension 57(4):723–730
Blaicher W, Speck E, Imhof MH, Gruber DM, Schneeberger C, Sator MO, Huber JC (2000) Melatonin in postmenopausal females. Arch Gynecol Obstet 263(3):116–118
Brewerton TD, Krahn DD, Hardin TA, Wehr TA, Rosenthal NE (1994) Findings from the Seasonal Pattern Assessment Questionnaire in patients with eating disorders and control subjects: effects of diagnosis and location. Psychiatry Res 52(1):71–84
Buxton OM, Cain SW, O’Connor SP, Porter JH, Duffy JF, Wang W, Czeisler CA, Shea SA (2012) Adverse metabolic consequences in humans of prolonged sleep restriction combined with circadian disruption. Sci Transl Med 4(129):129–143
Ellis BW, Johns MW, Lancaster R, Raptopoulos P, Angelopoulos N, Priest RG (1981) The St. Mary’s Hospital sleep questionnaire: a study of reliability. Sleep 4(1):93–97
Espino J, Pariente JA, Rodríguez AB (2011) Role of melatonin on diabetes-related metabolic disorders. World J Diabetes 2(6):82–91
Finucane MM, Stevens GA, Cowan MJ, Danaei G, Lin JK, Paciorek CJ, Singh GM, Gutierrez HR, Lu Y, Bahalim AN, Farzadfar F, Riley LM, Ezzati M (2011) Global Burden of Metabolic Risk Factors of Chronic Diseases Collaborating Group (Body Mass Index). National, regional, and global trends in body-mass index since 1980: systematic analysis of health examination surveys and epidemiological studies with 960 country-years and 9.1 million participants. Lancet 377(9765):557–567
Gilbert SS, van den Heuvel CJ, Dawson D (1999) Daytime melatonin and temazepam in young adult humans: equivalent effects on sleep latency and body temperatures. J Physiol 514(Pt 3):905–914
Grassi G, Facchini A, Trevano FQ, Dell’Oro R, Arenare F, Tana F, Bolla G, Monzani A, Robuschi M, Mancia G (2005) Obstructive sleep apnea-dependent and -independent adrenergic activation in obesity. Hypertension 46(2):321–325
Honma K, Honma S, Kohsaka M, Fukuda N (1992) Seasonal variation in the human circadian rhythm: dissociation between sleep and temperature rhythm. Am J Physiol 262(5 Pt 2):R885–R891
Horne JA, Ostberg O (1976) A self-assessment questionnaire to determine morningness-eveningness in human circadian rhythms. Int J Chronobiol 4(2):97–110
Hussein MR, Ahmed OG, Hassan AF, Ahmed MA (2007) Intake of melatonin is associated with amelioration of physiological changes, both metabolic and morphological pathologies associated with obesity: an animal model. Int J Exp Pathol 88(1):19–29
Koziróg M, Poliwczak AR, Duchnowicz P, Koter-Michalak M, Sikora J, Broncel M (2011) Melatonin treatment improves blood pressure, lipid profile, and parameters of oxidative stress in patients with metabolic syndrome. J Pineal Res 50(3):261–266
Kräuchi K, Cajochen C, Wirz-Justice A (1997) A relationship between heat loss and sleepiness: effects of postural change and melatonin administration. J Appl Physiol 83(1):134–139
Müller HL, Handwerker G, Wollny B, Faldum A, Sörensen N (2002) Melatonin secretion and increased daytime sleepiness in childhood craniopharyngioma patients. J Clin Endocrinol Metab 87(8):3993–3996
Mutoh T, Shibata S, Korf HW, Okamura H (2003) Melatonin modulates the light-induced sympathoexcitation and vagal suppression with participation of the suprachiasmatic nucleus in mice. J Physiol 547(Pt 1):317–332
Park SJ, Tokura H (1999) Bright light exposure during the daytime affects circadian rhythms of urinary melatonin and salivary immunoglobulin A. Chronobiol Int 16(3):359–371
Paulis L, Simko F (2007) Blood pressure modulation and cardiovascular protection by melatonin: potential mechanisms behind. Physiol Res 56(6):671–684
Piestrzeniewicz K, Łuczak K, Lelonek M, Wranicz JK, Goch JH (2008) Obesity and heart rate variability in men with myocardial infarction. Cardiol J 15(1):43–49
Rodríguez-Colón SM, Bixler EO, Li X, Vgontzas AN, Liao D (2011) Obesity is associated with impaired cardiac autonomic modulation in children. Int J Pediatr Obes 6(2):128–134
Rosen LN, Targum SD, Terman M, Bryant MJ, Hoffman H, Kasper SF, Hamovit JR, Docherty JP, Welch B, Rosenthal NE (1990) Prevalence of seasonal affective disorder at four latitudes. Psychiatry Res 31(2):131–144
Rosenthal NE, Bradt GJ, Wehr TA (1984) Seasonal Pattern Assessment Questionnaire in Assessment. National Institute of Mental Health, Bethesda
Scheen AJ, Van Cauter E (1998) The roles of time of day and sleep quality in modulating glucose regulation: clinical implications. Horm Res 49(3–4):191–201
Takasu NN, Hashimoto S, Yamanaka Y, Tanahashi Y, Yamazaki A, Honma S, Honma K (2006) Repeated exposures to daytime bright light increase nocturnal melatonin rise and maintain circadian phase in young subjects under fixed sleep schedule. Am J Physiol Regul Integr Comp Physiol 291(6):R1799–R1807
Task Force of the European Society of Cardiology and the North American Society of Pacing and Electrophysiology (1996) Heart rate variability. Standards of measurement, physiological interpretation, and clinical use. Eur Heart J 17(3):354–81
The Examination Committee of Criteria for ‘Obesity Disease’ in Japan, Japan Society for the Study of Obesity (2002) New Criteria for ‘Obesity Disease’ in Japan. Circ J 66:987–992
Touitou Y, Smolensky MH, Portaluppi F (2006) Ethics, standards, and procedures of animal and human chronobiology research. Chronobiol Int 23(6):1083–1096
Wehr TA, Moul DE, Barbato G, Giesen HA, Seidel JA, Barker C, Bender C (1993) Conservation of photoperiod-responsive mechanisms in humans. Am J Physiol 265(4 Pt 2):R846–R857
Yatsuya H, Yamagishi K, Iso H (2011) Adiposity and risk of cardiovascular diseases in Japan: secular trend, individual level associations and causal pathway—implications for the prevention of cardiovascular diseases in societies with rapid economic development. EPMA J 2:65–73
Zimberg IZ, Dâmaso A, Re MD, Carneiro AM, de Sá Souza H, de Lira FS, Tufik S, de Mello MT (2012) Short sleep duration and obesity: mechanisms and future perspectives. Cell Biochem Funct 30(6):524–529
Acknowledgments
The study was supported by a Grant from the Aikeikai Foundation, Japan in 2010 to M.S., and by a Grant from the Hori Information Science Promotion Foundation, Japan in 2010 to D.K.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Sato, M., Kanikowska, D., Iwase, S. et al. Seasonal differences in melatonin concentrations and heart rates during sleep in obese subjects in Japan. Int J Biometeorol 57, 743–748 (2013). https://doi.org/10.1007/s00484-012-0601-3
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00484-012-0601-3