Abstract
Background
Acid-base balance is maintained by kidney excretion of titratable acids and bicarbonate reabsorption. Metabolic alkalosis is uncommon in dialysis-treated patients. The aim of this retrospective study was to assess the rate of metabolic alkalosis in pediatric patients treated with peritoneal dialysis.
Methods
Medical records of children treated with peritoneal dialysis in Shaare Zedek Medical Center from January 2000 to June 2021 were reviewed and compared with young adults currently treated with peritoneal dialysis. Demographic, clinical, and peritoneal dialysis characteristics were extracted from the medical records.
Results
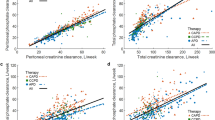
Thirty chronic peritoneal dialysis patients were included in our study, seven under 2 years, 13 between 2 and 18 years, and 10 adults. 90.3% of the measurements in infants showed metabolic alkalosis compared to 32.3% in the 2–18-year group and none in the adult group. Higher size-adjusted daily exchange volume, lack of urine output, and high lactate-containing dialysate were associated with metabolic alkalosis. Alkalosis was not explained by vomiting, diuretic therapy, or carbonate-containing medications. High transport membrane, low dietary protein, and malnutrition, all previously reported explanations for metabolic alkalosis, were not found in our study.
Conclusions
Metabolic alkalosis is common in infants treated with peritoneal dialysis as opposed to older children and adults. High lactate-containing dialysate is a possible explanation. Higher size-adjusted daily dialysate exchange volume, which may reflect higher bicarbonate absorption, is another independent predictor of alkalosis. Acid-base status should be closely followed in infants, and using a dialysis solution with lower bicarbonate or lactate level should be considered.
Graphical abstract
A higher resolution version of the graphical abstract is available as Supplementary Information


Similar content being viewed by others
Availability of data and material
The data that support the findings of this study are available from the corresponding author upon reasonable request.
Code availability
Not applicable.
Abbreviations
- CKD:
-
Chronic kidney disease
- GFR:
-
Glomerular filtration rate
- PD:
-
Peritoneal dialysis
- IRB:
-
Institutional Review Board
- PET:
-
Peritoneal equilibration test
- nPCR:
-
Normalized protein catabolic rate
- WHO:
-
World Health Organization
- CDC:
-
Centers for Disease Control and Prevention
- BMI:
-
Body mass index
- NIH:
-
National Institute of Health
- NKF KDOQI:
-
National Kidney Foundation Kidney Disease Outcomes Quality Initiative
- BSA:
-
Body surface area
- SD:
-
Standard deviation
- IQR:
-
Interquartile range
- CAPD:
-
Continuous ambulatory peritoneal dialysis
- APD:
-
Automated peritoneal dialysis
- HD:
-
Hemodialysis
- DRI:
-
Dietary reference intake
References
Kovesdy CP (2012) Metabolic acidosis and kidney disease: does bicarbonate therapy slow the progression of CKD? Nephrol Dial Transplant 27:3056–3062
Uribarri J, Levin NW, Delmez J, Depner TA, Ornt D, Owen W, Yan G (1999) Association of acidosis and nutritional parameters in hemodialysis patients. Am J Kidney Dis 34:493–499
Tschudy MM, Arcara KM (2012) The Harriet Lane handbook: a manual for pediatric house officers, 19th edn. Elsevier, Philadelphia, p 641
Kaiser BA, Polinsky MS, Stover J, Morgenstern BZ, Baluarte HJ (1994) Growth of children following the initiation of dialysis: a comparison of three dialysis modalities. Pediatr Nephrol 8:733–738
Dobre M, Yang W, Pan Q, Appel L, Bellovich K, Chen J, Feldman H, Fischer MJ, Ham LL, Hostetter T, Jaar BG, Kallem RR, Rosas SE, Scialla JJ, Wolf M, Rahman M, CRIC Study Investigators (2015) Persistent high serum bicarbonate and the risk of heart failure in patients with chronic kidney disease (CKD): a report from the Chronic Renal Insufficiency Cohort (CRIC) study. J Am Heart Assoc 4:e001599
Anderson LE, Henrich WL (1987) Alkalemia-associated morbidity and mortality in medical and surgical patients. South Med J 80:729–733
Galla JH (2000) Metabolic alkalosis. J Am Soc Nephrol 11:369–375
Warady BA, Alexander SR, Hossli S, Vonesh E, Geary D, Watkins S, Salusky IB, Kohaut EC (1996) Peritoneal membrane transport function in children receiving long-term dialysis. J Am Soc Nephrol 7:2385–2391
Tattersall JE, Dick C, Doyle S, Greenwood RN, Farrington K (1995) Alkalosis and hypomagnesaemia: unwanted effects of a low-calcium CAPD solution. Nephrol Dial Transplant 10:258–262
KDOQI Working Group (2009) KDOQI Clinical Practice Guideline for Nutrition in Children with CKD: 2008 update. Executive summary. Am J Kidney Dis 53:S11–S104
KDOQI Working Group (2000) KDOQI Clinical practice guideline for nutrition in CKD. Am J Kidney Dis 3576(3 supp1):S1-S107
Juarez-Congelosi M, Orellana P, Goldstein SL (2007) Normalized protein catabolic rate versus serum albumin as a nutrition status marker in pediatric patients receiving hemodialysis. J Ren Nutr 17:269–274
Kung SC, Morse SA, Bloom E, Raja RM (2001) Acid-base balance and nutrition in peritoneal dialysis. Adv Perit Dial 17:235–237
Kang DH, Yoon KI, Lee HY, Han DS (1998) Impact of peritoneal membrane transport characteristics on acid-base status in CAPD patients. Perit Dial Int 18:294–302
Author information
Authors and Affiliations
Contributions
STB and EBS contributed to the study conception and design. STB, AB, and EBS performed data collection and analysis. The first draft of the manuscript was written by STB, and AB, RBC, CR, JWG, SC, LS, YF, and EBS commented on previous versions of the manuscript. All authors read and approved the final manuscript. As the corresponding author, Shimrit Tzvi-Behr confirms that the manuscript has been read and approved for submission by all the named authors.
Corresponding author
Ethics declarations
Ethics approval
The study was approved by the Institutional Review Board (IRB) at the Shaare Zedek Medical Center (Approval number: 0272-19-SZMC). We declare that this manuscript is original, has not been published before, and is not currently being considered for publication elsewhere.
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Tzvi-Behr, S., Bnaya, A., Becker-Cohen, R. et al. Metabolic alkalosis in infants treated with peritoneal dialysis. Pediatr Nephrol 37, 1889–1895 (2022). https://doi.org/10.1007/s00467-021-05344-w
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00467-021-05344-w