Abstract
Background
Oral cyclophosphamide (CYP) is an important therapeutic agent in treatment of steroid-sensitive nephrotic syndrome having a steroid-dependent (SD) or frequent relapsing (FR) course. This retrospective observational study aimed to determine response to oral CYP and factors associated with positive response in these patients.
Methods
We studied 100 children (male; 75) with FR (19%) and SD (81%) NS treated with CYP in the Pediatric Nephrology clinic. Responders were defined as children in whom steroids were stopped for at least 6 months following CYP and factors affecting response were analysed. Relapse-free survival was estimated by Kaplan–Meier method.
Results
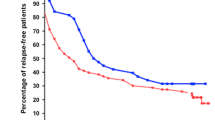
Median age at onset of NS was 3 years (IQR 2–5.2). Median age at CYP was 5.7 years (IQR 3.7–7.9). Fifty percent of patients were in the responder group at 6 months of CYP. Relapse-free survival post CYP therapy was 31% at 1 year, 11% at 2 years. Factors predicting good response were age at onset of NS > 3 years with 61.2% response at 6 months (p = 0.028) and older age at CYP initiation (> 5 years) with 61% response (p = 0.008). Multivariate regression analysis showed age at start of CYP > 5 years was an independent factor for good response (p = 0.044, OR = 2.903, CI −1.03 to 8.18).
Conclusions
Judicious selection of patients, especially with age of onset of NS more than 3 years and initiation of CYP after age of 5 years, can predict better response in this group of patents.
Graphical abstract



Similar content being viewed by others
References
Cammas B, Harambat J, Bertholet-Thomas A, Bouissou F, Morin D, Guigonis V, Bendeddouche S, Afroukh-Hacini N, Cochat P, Llanas B, Decramer S, Ranchin B (2011) Long-term effects of cyclophosphamide therapy in steroid-dependent or frequently relapsing idiopathic nephrotic syndrome. Nephrol Dial Transplant 26:178–184. https://doi.org/10.1093/ndt/gfq405
Nishi S, Ubara Y, Utsunomiya Y, Okada K, Obata Y, Kai H, Kiyomoto H, Goto S, Konta T, Sasatomi Y, Sato Y, Nishino T, Tsuruya K, Furuichi K, Hoshino J, Watanabe Y, Kimura K, Matsuo S (2016) Evidence-based clinical practice guidelines for nephrotic syndrome 2014. Clin Exp Nephrol 20:342–370. https://doi.org/10.1007/s10157-015-1216-x
Martinelli R, Pereira L, Silva O, Okumura A, Rocha H (2004) Cyclophosphamide in the treatment of focal segmental glomerulosclerosis. Braz J Med Biol Res 37:1365–1372. https://doi.org/10.1590/s0100-879x2004000900011
Shohet I, Meyerovitch J, Aladiem M, Boichis H (1988) Cyclophosphamide in treatment of minimal change nephrotic syndrome. Eur J Pediatr 147:239–241. https://doi.org/10.1007/BF00442686
Ponticelli C, Edefonti A, Ghio L, Rizzoni G, Rinaldi S, Gusmano R, Lama G, Zacchello G, Confalonieri R, Altieri P, Bettinelli A, Maschio G, Cinotti GA, Fuiano G, Schena FP, Castellani A, Delia Casa-Alberighi O (1993) Cyclosporin versus cyclophosphamide for patients with steroid-dependent and frequently relapsing idiopathic nephrotic syndrome: a multicentre randomized controlled trial. Nephrol Dial Transplant 8:1326–1332
Sümegi V, Haszon I, Bereczki C, Papp F, Túri S (2008) Long-term follow-up after cyclophosphamide and cyclosporine-A therapy in steroid-dependent and resistant nephrotic syndrome. Pediatr Nephrol 23:1085–1092. https://doi.org/10.1007/s00467-008-0771-8
Siegel N, Gaudio K, Krassner L, McDonald B, Anderson F, Kashgarian M (1981) Steroid-dependent nephrotic syndrome in children: histopathology and relapses after cyclophosphamide treatment. Kidney Int 19:454–459
Moncrieff MW, White RH, Oggs CS, Cameron JS (1969) Cyclophosphamide therapy in the nephrotic syndrome in childhood. Br Med J 1:666–671. https://doi.org/10.1136/bmj.1.5645.666
Tejani A, Phadke K, Nicastri A, Adamson O, Chen CK, Trachtman H, Tejani C (1985) Efficacy of cyclophosphamide in steroid-sensitive childhood nephrotic syndrome with different morphological lesions. Nephron 41:170–173. https://doi.org/10.1159/000183575
Ponticelli C, Escoli R, Moroni G (2018) Does cyclophosphamide still play a role in glomerular diseases? Autoimmun Rev 17:1022–1027. https://doi.org/10.1016/j.autrev.2018.04.007
Al Salloum AA, Muthanna A, Bassrawi R, Al Shehab AA, Al Ibrahim A, Islam MZ, Al Hasan K (2012) Long-term outcome of the difficult nephrotic syndrome in children. Saudi J Kidney Dis Transpl 23:965–972. https://doi.org/10.4103/1319-2442.100877
Indian Pediatric Nephrology Group, Indian Academy of Pediatrics, Bagga A, Ali U, Banerjee S, Kanitkar M, Phadke KD, Senguttuvan P, Sethi S, Shah M (2008) Management of steroid sensitive nephrotic syndrome: revised guidelines. Indian Pediatr 45:203–214
Azib S, Macher MA, Kwon T, Dechartres A, Alberti C, Loirat C, Deschênes G, Baudouin V (2011) Cyclophosphamide in steroid-dependent nephrotic syndrome. Pediatr Nephrol 26:927–932. https://doi.org/10.1007/s00467-011-1830-0
Watson AR, Rance CP, Bain J (1985) Long term effects of cyclophosphamide on testicular function. Br Med J (Clin Res Ed) 291:1457–1460. https://doi.org/10.1136/bmj.291.6507.1457
Yule SM, Boddy AV, Cole M, Price L, Wyllie R, Tasso MJ, Pearson AD, Idle JR (1996) Cyclophosphamide pharmacokinetics in children. Br J Clin Pharmacol 41:13–19. https://doi.org/10.1111/j.1365-2125.1996.tb00153.x
Van Husen M, Kemper MJ (2011) New therapies in steroid-sensitive and steroid-resistant idiopathic nephrotic syndrome. Pediatr Nephrol 26:881–892. https://doi.org/10.1007/s00467-010-1717-5
Vester U, Kranz B, Zimmermann S, Hoyer P (2003) Cyclophosphamide in steroid-sensitive nephrotic syndrome: outcome and outlook. Pediatr Nephrol 18:661–664. https://doi.org/10.1007/s00467-003-1170-9
Ueda N, Kuno K, Ito S (1990) Eight and 12 week courses of cyclophosphamide in nephrotic syndrome. Arch Dis Child 65:1147–1150. https://doi.org/10.1136/adc.65.10.1147
Vester U, Kranz B, Zimmermann S, Büscher R, Hoyer PF (2005) The response to cyclophosphamide in steroid-sensitive nephrotic syndrome is influenced by polymorphic expression of glutathion-S-transferases-M1 and -P1. Pediatr Nephrol 20:478–481. https://doi.org/10.1007/s00467-004-1759-7
Bhimma R, Adhikari M, Asharam K (2006) Steroid-resistant nephrotic syndrome: the influence of race on cyclophosphamide sensitivity. Pediatr Nephrol 21:1847–1853. https://doi.org/10.1007/s00467-006-0276-2
Zagury A, de Oliveira AL, de Moraes CA, de Araujo Montalvão JA, Novaes RH, de Sá VM, Monteiro de Carvalho Dde B, Matuck T (2011) Long-term follow-up after cyclophosphamide therapy in steroid-dependent nephrotic syndrome. Pediatr Nephrol 26:915–920. https://doi.org/10.1007/s00467-011-1825-x
Durkan A, Hodson E, Willis N, Craig J (2001) Immunosuppressive agents in childhood nephrotic syndrome: a meta-analysis of randomized controlled trials. Kidney Int 59:1919–1927. https://doi.org/10.1046/j.1523-1755.2001.0590051919.x
Larkins NG, Liu ID, Willis NS, Craig JC, Hodson EM (2020) Non-corticosteroid immunosuppressive medications for steroid-sensitive nephrotic syndrome in children. Cochrane Database Syst Rev 4:CD002290. https://doi.org/10.1002/14651858.CD002290.pub5
Kemper MJ, Altrogge H, Ludwig K, Timmermann K, Müller-Wiefel DE (2000) Unfavorable response to cyclophosphamide in steroid-dependent nephrotic syndrome. Pediatr Nephrol 14:772–775. https://doi.org/10.1007/pl00013435
Report of Arbeitsgemeinschaft für Pädiatrische Nephrologie (1987) Cyclophosphamide treatment of steroid dependent nephrotic syndrome: comparison of eight week with 12 week course. Arch Dis Child 62:1102–1106. https://doi.org/10.1136/adc.62.11.1102
Kari JA, Alhasan KA, Albanna AS, Safdar OY, Shalaby MA, Böckenhauer D, El-Desoky SM (2020) Rituximab versus cyclophosphamide as first steroid-sparing agent in childhood frequently relapsing and steroid-dependent nephrotic syndrome. Pediatr Nephrol 35:1445–1453. https://doi.org/10.1007/s00467-020-04570-y
Webb H, Jaureguiberry G, Dufek S, Tullus K, Bockenhauer D (2016) Cyclophosphamide and rituximab in frequently relapsing/steroid-dependent nephrotic syndrome. Pediatr Nephrol 31:589–594. https://doi.org/10.1007/s00467-015-3245-9
Hoyer PF (2015) New lessons from randomized trials in steroid-sensitive nephrotic syndrome: clear evidence against long steroid therapy. Kidney Int 87:17–19. https://doi.org/10.1038/ki.2014.354
Hoyer PF, Brodeh J (2006) Initial treatment of idiopathic nephrotic syndrome in children: prednisone versus prednisone plus cyclosporine A: a prospective, randomized trial. J Am Soc Nephrol 17:1151–1157. https://doi.org/10.1681/ASN.2005090922
Latta K, von Schnakenburg C, Ehrich J (2001) A meta-analysis of cytotoxic treatment for frequently relapsing nephrotic syndrome in children. Pediatr Nephrol 16:271–282. https://doi.org/10.1007/s004670000523
Berns JS, Gaudio KM, Krassner LS, Anderson FP, Durante D, McDonald BM, Siegel NJ (1987) Steroid-responsive nephrotic syndrome of childhood: a long-term study of clinical course, histopathology, efficacy of cyclophosphamide therapy, and effects on growth. Am J Kidney Dis 9:108–114. https://doi.org/10.1016/s0272-6386(87)80087-2
Moorani KN, Zubair AM, Veerwani NR, Hotchandani HJ (2020) Efficacy of levamisole in children with frequent relapsing and steroid dependent nephrotic syndrome at tertiary care center-Karachi. Pak J Med Sci 36:1193–1198. https://doi.org/10.12669/pjms.36.6.2337
Acknowledgements
The authors acknowledge all of the parents round the world who are constantly involved in the care of children with nephrotic syndrome.
Author information
Authors and Affiliations
Contributions
JS, DB: recruited the subjects, collected the data, carried out the literature review and prepared the initial draft of the manuscript; PAP, SB, SK: contributed to manuscript writing; GSD: conceived and designed the study, analysed the data and finalized the manuscript. All authors have approved the manuscript submitted.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethical clearance
Institutional ethics committee.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Sandhu, J., Bhat, D., Dhooria, G.S. et al. Oral cyclophosphamide therapy in 100 children with steroid-sensitive nephrotic syndrome: experience from a developing country. Pediatr Nephrol 36, 2759–2767 (2021). https://doi.org/10.1007/s00467-021-05052-5
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00467-021-05052-5