Abstract
Background
This study aimed to identify main factors associated with child and adolescent access to chronic kidney disease (CKD) treatment in Brazil.
Methods
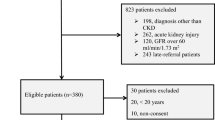
Multi-center cross-sectional study conducted in eight pediatric nephrology centers across all Brazilian geographic regions. Information was collected on characteristics associated with referral and treatment of patients with CKD. The following outcomes were analyzed as follows: (1) age at first consultation, and (2) time elapsed between referral and treatment at the specialized service.
Results
Three hundred thirty-five children were assessed. Variables associated with age at first consultation were as follows: CAKUT (HR=1.7; 95%CI 1.3–2.2, p<0.01); private health plan (HR=1.54; 95%CI 1.06–2.23, p=0.02); modified Medical Outcomes Study Social Support Survey mMOS-SS score (HR=1.02; 95%CI 1.00–1.03, p=0.024); maternal age (HR=0.96; 95%CI 0.95–0.97, p<0.01); and number of siblings in the household (HR=0.86; 95%CI 0.79–0.83, p<0.01). Significant variables associated with time elapsed between referral and treatment at the specialized service were as follows: each additional occupant sharing the household (HR=0.94; 95%CI:0.89–0.99, p=0.02), residing in the Northeast (HR=0.81; 95%CI:0.67–0.98, p=0.03) and having someone to take them to the physician (HR=1.36; 95%CI 1.07–1.74, p=0.01). The median time interval between patient referral and treatment by the service was 11 days (IQR 10–31).
Conclusion
There are potentially modifiable factors hampering access of children with CKD to specialized treatment. The importance of the role of social support for the two outcomes should serve as an alert for health managers and professionals to consider this aspect throughout all steps of the care process of children with CKD.




Similar content being viewed by others
References
Parmar MS (2002) Chronic renal disease. BMJ 325:85–90. https://doi.org/10.1136/bmj.325.7355.85
Kidney disease: improving global outcomes (KDIGO) CKD work group (2013) KDIGO 2012 clinical practice guideline for the evaluation and management of chronic kidney disease. Kidney Int Suppl 3:1–150. https://doi.org/10.1038/kisup.2012.76
Orta-Sibu N, Exeni RA, Garcia C (2009) Latin America. In: Avner ED, Harmon WE, Niaudet P, Yoshikawa N (eds) Pediatric Nephrology. Springer, Verlag, pp 1969–1974
Nogueira PCK, Feltran LS, Camargo MF, Leão ER, BnniNghoveN JRCS, Gonçalves NZ, Pereira LA, Sesso RC (2011) Prevalência estimada da doença renal crônica terminal em crianças no Estado de São Paulo. Rev Assoc Med Bra 57:443–449
Collins GS, Omar O, Shanyinde M, Yu LM (2013) A systematic review finds prediction models for chronic kidney disease were poorly reported and often developed using inappropriate methods. J Clin Epidemiol 66:268–277. https://doi.org/10.1016/j.jclinepi.2012.11.012
Paim JS (2018) Sistema Único de Saúde (SUS) aos 30 anos. Ciênc Saúde Coletiva 23:1723–1728. https://doi.org/10.1590/1413-81232018236.09172018
Konstantyner T, Sesso R, de Camargo MF, de Santis FL, Koch-Nogueira PC (2015) Pediatric chronic dialysis in Brazil: epidemiology and regional inequalities. PLoS One 10:e0135649. https://doi.org/10.1371/journal.pone.0135649
Cleto-Yamane TL, Gomes CLR, Suassuna JHR, Nogueira PCK (2019) Epidemiologia da lesão renal aguda em pediatria. J Bras Nefrol 41:275–283. https://doi.org/10.1590/2175-8239-jbn-2018-0127
Crews DC, Bello AK, Saadi G (2019) Burden, access, and disparities in kidney disease. Exp Clin Transplant 17:131–137. https://doi.org/10.1590/1414-431x20198338
Sesso R, Belasco AG (1996) Late diagnosis of chronic renal failure and mortality on maintenance dialysis. Nephrol Dial Transplant 11:2417–2420. https://doi.org/10.1093/ndt/11.12.2417
Nogueira PCK, Konstantyner T, Carvalho MFC, Pinto CCX, Paz IP, Belangero VMS, Tavare MS, Garcia CD, Ferra Net OA, Zuntini KLCR, Lordelo MR, Oi SSP, Damasceno RT, Sesso R (2019) Development of a risk score for earlier diagnosis of chronic kidney disease in children. PLoS One 14:e0215100. https://doi.org/10.1371/journal.pone.0215100
Schwartz GJ, Muñoz A, Schneider MF, Mak RH, Kaskel F, Waradyand BA, Furth SL (2009) New equations to estimate GFR in children with CKD. J Am Soc Nephrol 20:629–637. https://doi.org/10.1681/ASN.2008030287
ABEP (2015) Critério Brasil 2015 e atualização da distribuição de classes para 2016. http://www.abep.org. Accessed 10 Jan 2020
Zanini DS, Peixoto EM, Nakano TC (2018) Escala de apoio social (MOS-SSS): proposta de normatização com referência nos itens. Temas Psicol 26:387–399. https://doi.org/10.9788/TP2018.1-15Pt
Griep RH, Chor D, Faerstein E, Wernwck GC, Lopes CS (2005) Validade de constructo de escala de apoio social do Medical Outcomes Study adaptada para o português no Estudo Pró-Saúde Construct. Cad Saúde Pública 21:703–714. https://doi.org/10.9788/TP2018.1-15En
Moser A, Stuck AE, Silliman RA, Ganz P, Clough-Gorr KM (2012) The eight- item modified Medical Outcomes Study Social Support Survey: psychometric evaluation showed excellent performance. J Clin Epidemiol 65:1107–1116. https://doi.org/10.1016/j.jclinepi.2012.04.00
SiIva ACS, Oliveira EA (2015) Update on the approach of urinary tract infection in childhood. J Pediatr 91:S2–S10. https://doi.org/10.1016/j.jped.2015.05.003
Lorenzo AJ (2010) Medical versus surgical management for vesicoureteric reflux: the case for medical management. CUAJ 4:276–279. https://doi.org/10.5489/cuaj.1082
NAPRTCS (2014) Collaborative studies NAPRTCS annual transplant report. http://www.naprtcs.org. Accessed 10 Jan 2020
Harambat J, van Stralen KJ, Kim JJ, Tizard EJ (2012) Epidemiology of chronic kidney disease in children. Pediatr Nephrol 27:363–373. https://doi.org/10.1007/s00467-011-1939-1
Rodriguez MM (2014) Congenital anomalies of the kidney and the urinary tract (CAKUT). Fetal Pediatr Pathol 33:293–320. https://doi.org/10.3109/15513815.2014.959678
Alcalde PR, Kirsztajn GM (2018) Expenses of the Brazilian Public Healthcare System with chronic kidney disease. J Bras Nefrol 40:122–129. https://doi.org/10.1590/2175-8239-jbn-3918
Malta DC, Stopa SR, Pereira CA, Szwarcwald CL, Oliveira M, dos Reis AC (2017) Cobertura de planos de saúde na população brasileira, segundo a Pesquisa Nacional de Saúde. Ciênc Saúde Coletiva 22:179–190. https://doi.org/10.1590/1413-81232017221.16782015
Carlos L, Cecilio DO (1997) Modelos tecno-assistenciais em saúde - da pirâmide ao círculo. Cad Saúde Públ 13:469–478. https://doi.org/10.1590/S0102-311X1997000300022
IBGE (2019) Instituto Braileiro de geografia e Estatística. https://www.ibge.gov.br. Accessed 10 Jan 2020
Acknowledgements
The authors would like to thank the referral centers and professionals for their contributions to the study: Santa Casa do Pará, Belém; Hospital Albert Sabin, Ceará; HUUFMS, Mato Grosso do Sul; Santa Casa de Belo Horizonte, Minas Gerais; HUUFMA, Maranhão; Hospital Roberto Santos, Bahia; Hospital de Clínicas UNICAMP, São Paulo; and Irmandade da Santa Casa de Porto Alegre, Rio Grande do Sul.
Funding
This study was funded by the Brazilian Health Ministry, Support Program for the Institutional Development of the National Health System—Proadi-SUS, under grant no. 25000.180613/2011-11.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflicts of interest.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
ESM 1
(DOCX 42 kb)
Rights and permissions
About this article
Cite this article
de Pádua Paz, I., Konstantyner, T., de Castro Cintra Sesso, R. et al. Access to treatment for chronic kidney disease by children and adolescents in Brazil. Pediatr Nephrol 36, 2827–2835 (2021). https://doi.org/10.1007/s00467-021-05009-8
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00467-021-05009-8