Abstract
Background
The consensus definition of acute kidney injury (AKI) has evolved since developing the original multiple organ dysfunction syndrome (MODS) definitions. Whether or not risk for adverse short- and long-term outcomes can be identified using the refined AKI criteria in the setting of MODS has not been studied. We hypothesize that incorporation of Kidney Disease: Improving Global Outcome (KDIGO) AKI criteria into existing MODS definitions will have a higher association with major adverse kidney events at 30 days (MAKE30) and will increase the number of patients with MODS.
Methods
Post hoc analysis of 410 children admitted to a tertiary care pediatric intensive care unit (PICU) was conducted. MODS was defined using two existing criteria (Goldstein and Proulx) during the first 7 days following ICU admission and then modified by replacement of the kidney injury criteria using the KDIGO AKI definitions (G′ and P′).
Results
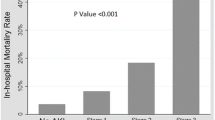
MAKE30 occurred in 65 of 410 (16%) children. After substituting KDIGO kidney injury criteria, identification of MAKE30 increased from 46 children (71%) to 53 (82%) and 29 children (45%) to 43 (66%) for the Goldstein and Proulx criteria, respectively. Additionally, identification of MODS increased from 194 (47%) by Goldstein to 224 (55%) by G′ and 95 children (23%) by Proulx to 132 (32%) by P′.
Conclusions
Substituting KDIGO AKI criteria into existing MODS criteria increases the sensitivity for major adverse kidney events as well as the identification of MODS, improving the detection of children at risk for long-term adverse renal outcomes.


Similar content being viewed by others
References
Farris RWD, Weiss NS, Zimmerman JJ (2013) Functional outcomes in pediatric severe Sepsis. Pediatr Crit Care Med 14:835–842. https://doi.org/10.1097/pcc.0b013e3182a551c8
Lin JC, Spinella PC, Fitzgerald JC, Tucci M, Bush JL, Nadkarni VM, Thomas NJ, Weiss SL, Sepsis Prevalence, Outcomes, and Therapy Study Investigators (2017) New or progressive multiple organ dysfunction syndrome in pediatric severe Sepsis. Pediatr Crit Care Med 18:8–16. https://doi.org/10.1097/pcc.0000000000000978
Typpo KV, Petersen NJ, Hallman DM, Markovitz BP, Mariscalco MM (2009) Day 1 multiple organ dysfunction syndrome is associated with poor functional outcome and mortality in the pediatric intensive care unit. Pediatr Crit Care Med 10:562–570. https://doi.org/10.1097/pcc.0b013e3181a64be1
Leclerc F, Leteurtre S, Duhamel A, Grandbastien B, Proulx F, Martinot A, Gauvin F, Hubert P, Lacroix J (2005) Cumulative influence of organ dysfunctions and septic state on mortality of critically ill children. Am J Resp Crit Care 171:348–353. https://doi.org/10.1164/rccm.200405-630oc
Leteurtre S, Martinot A, Duhamel A, Proulx F, Grandbastien B, Cotting J, Gottesman R, Joffe A, Pfenninger J, Hubert P, Lacroix J, Leclerc F (2003) Validation of the paediatric logistic organ dysfunction (PELOD) score: prospective, observational, multicentre study. Lancet 362:192–197. https://doi.org/10.1016/s0140-6736(03)13908-6
Graciano AL, Balko JA, Rahn DS, Ahmad N, Giroir BP (2005) The pediatric multiple organ dysfunction score (P-MODS): development and validation of an objective scale to measure the severity of multiple organ dysfunction in critically ill children. Crit Care Med 33:1484–1491. https://doi.org/10.1097/01.ccm.0000170943.23633.47
Watson RS, Crow SS, Hartman ME, Lacroix J, Odetola FO (2017) Epidemiology and outcomes of pediatric multiple organ dysfunction syndrome. Pediatr Crit Care Med 18:S4–S16. https://doi.org/10.1097/pcc.0000000000001047
Proulx F, Fayon M, Farrell CA, Lacroix J, Gauthier M (1996) Epidemiology of sepsis and multiple organ dysfunction syndrome in children. Chest 109:1033–1037. https://doi.org/10.1378/chest.109.4.1033
Goldstein B, Giroir B, Randolph A, International Consensus Conference on Pediatric Sepsis (2005) International pediatric sepsis consensus conference: definitions for sepsis and organ dysfunction in pediatrics. Pediatr Crit Care Med 6:2–8. https://doi.org/10.1097/01.pcc.0000149131.72248.e6
Kidney Disease: Improving Global Outcomes (KDIGO) Acute Kidney Injury Work Group (2012) KDIGO clinical practice guideline for acute kidney injury. Kidney Int Suppl 2:1–138. https://doi.org/10.1038/kisup.2012.2
Kaddourah A, Basu RK, Bagshaw SM, Goldstein SL (2017) Epidemiology of acute kidney injury in critically ill children and young adults. N Engl J Med 376:11–20. https://doi.org/10.1056/nejmoa1611391
Kaddourah A, Basu RK, Goldstein SL, Sutherland SM, Assessment of Worldwide Acute Kidney Injury, Renal Angina and, Epidemiology (AWARE) Investigators (2019) Oliguria and acute kidney injury in critically ill children: implications for diagnosis and outcomes. Pediatr Crit Care Med 20:332–339. https://doi.org/10.1097/pcc.0000000000001866
Weiss SL, Balamuth F, Thurm CW, Downes KJ, Fitzgerald JC, Laskin BL (2019) Major adverse kidney events in pediatric Sepsis. Clin J Am Soc Nephrol 14:664–672. https://doi.org/10.2215/cjn.12201018
Billings FT, Shaw AD (2014) Clinical trial endpoints in acute kidney injury. Nephron Clin Pract 127:89–93. https://doi.org/10.1159/000363725
Carlton EF, Close J, Paice K, Dews A, Gorga SM, Sturza J, Barbaro RP, Cornell TT, Prescott HC (2020) Clinician accuracy in identifying and predicting organ dysfunction in critically ill children. Crit Care Med 48:e1012–e1019. https://doi.org/10.1097/ccm.0000000000004555
Alkandari O, Eddington KA, Hyder A, Gauvin F, Ducruet T, Gottesman R, Phan V, Zappitelli M (2011) Acute kidney injury is an independent risk factor for pediatric intensive care unit mortality, longer length of stay and prolonged mechanical ventilation in critically ill children: a two-center retrospective cohort study. Crit Care 15:R146. https://doi.org/10.1186/cc10269
Selewski DT, Cornell TT, Heung M, Troost JP, Ehrmann BJ, Lombel RM, Blatt NB, Luckritz K, Hieber S, Gajarski R, Kershaw DB, Shanley TP, Gipson DS (2014) Validation of the KDIGO acute kidney injury criteria in a pediatric critical care population. Intensive Care Med 40:1481–1488. https://doi.org/10.1007/s00134-014-3391-8
Hessey E, Ali R, Dorais M, Morissette G, Pizzi M, Rink N, Jouvet P, Lacroix J, Phan V, Zappitelli M (2017) Evaluation of height-dependent and height-independent methods of estimating baseline serum creatinine in critically ill children. Pediatr Nephrol 32:1953–1962. https://doi.org/10.1007/s00467-017-3670-z
Gaies MG, Gurney JG, Yen AH, Napoli ML, Gajarski RJ, Ohye RG, Charpie JR, Hirsch JC (2010) Vasoactive–inotropic score as a predictor of morbidity and mortality in infants after cardiopulmonary bypass. Pediatr Crit Care Med 11:234–238. https://doi.org/10.1097/pcc.0b013e3181b806fc
Semler MW, Self WH, Wanderer JP, Ehrenfeld JM, Wang L, Byrne DW, Stollings JL, Kumar AB, Hughes CG, Hernandez A, Guillamondegui OD, May AK, Weavind L, Casey JD, Siew ED, Shaw AD, Bernard GR, Rice TW, SMART Investigators and the Pragmatic Critical Care Research Group (2018) Balanced crystalloids versus saline in critically ill adults. N Engl J Med 378:829–839. https://doi.org/10.1056/nejmoa1711584
Le CT (2006) A solution for the most basic optimization problem associated with an ROC curve. Stat Methods Med Res 15:571–584. https://doi.org/10.1177/0962280206070637
Hessey E, Ali R, Dorais M, Pizzi M, Rink N, Jouvet P, Lacroix J, Phan V, Zappitelli M (2017) Renal function follow-up and renal recovery after acute kidney injury in critically ill children. Pediatr Crit Care Med 18:733–740. https://doi.org/10.1097/pcc.0000000000001166
Chawla LS, Amdur RL, Shaw AD, Faselis C, Palant CE, Kimmel PL (2014) Association between AKI and long-term renal and cardiovascular outcomes in United States veterans. Clin J Am Soc Nephrol 9:448–456. https://doi.org/10.2215/cjn.02440213
Greenberg JH, Zappitelli M, Devarajan P, Thiessen-Philbrook HR, Krawczeski C, Li S, Garg AX, Coca S, Parikh CR, TRIBE-AKI Consortium (2016) Kidney outcomes 5 years after pediatric cardiac surgery: the TRIBE-AKI study. JAMA Pediatr 170:1071–1078. https://doi.org/10.1001/jamapediatrics.2016.1532
Mammen C, Abbas AA, Skippen P, Nadel H, Levine D, Collet JP, Matsell DG (2012) Long-term risk of CKD in children surviving episodes of acute kidney injury in the intensive care unit: a prospective cohort study. Am J Kidney Dis 59:523–530. https://doi.org/10.1053/j.ajkd.2011.10.048
Askenazi DJ, Feig DI, Graham NM, Hui-Stickle S, Goldstein SL (2006) 3–5 year longitudinal follow-up of pediatric patients after acute renal failure. Kidney Int 69:184–189. https://doi.org/10.1038/sj.ki.5000032
Chawla LS, Amdur RL, Faselis C, Li P, Kimmel PL, Palant CE (2017) Impact of acute kidney injury in patients hospitalized with pneumonia. Crit Care Med 45:600–606. https://doi.org/10.1097/ccm.0000000000002245
Fiorentino M, Tohme FA, Wang S, Murugan R, Angus DC, Kellum JA (2018) Long-term survival in patients with septic acute kidney injury is strongly influenced by renal recovery. PLoS One 13:e0198269. https://doi.org/10.1371/journal.pone.0198269
Izawa J, Uchino S, Takinami M (2016) A detailed evaluation of the new acute kidney injury criteria by KDIGO in critically ill patients. J Anesth 30:215–222. https://doi.org/10.1007/s00540-015-2109-6
Villeneuve A, Joyal J-S, Proulx F, Ducruet T, Poitras N, Lacroix J (2016) Multiple organ dysfunction syndrome in critically ill children: clinical value of two lists of diagnostic criteria. Ann Intensive Care 6:40. https://doi.org/10.1186/s13613-016-0144-6
Chawla LS, Bellomo R, Bihorac A, Goldstein SL, Siew ED, Bagshaw SM, Bittleman D, Cruz D, Endre Z, Fitzgerald RL, Forni L, Kane-Gill SL, Hoste E, Koyner J, Liu KD, Macedo E, Mehta R, Murray P, Nadim M, Ostermann M, Palevsky PM, Pannu N, Rosner M, Wald R, Zarbock A, Ronco C, Kellum JA, Acute Disease Quality Initiative Workgroup 16 (2017) Acute kidney disease and renal recovery: consensus report of the Acute Disease Quality Initiative (ADQI) 16 Workgroup. Nat Rev Nephrol 13:241–257. https://doi.org/10.1038/nrneph.2017.2
Akcan-Arikan A, Zappitelli M, Loftis LL, Washburn KK, Jefferson LS, Goldstein SL (2007) Modified RIFLE criteria in critically ill children with acute kidney injury. Kidney Int 71:1028–1035. https://doi.org/10.1038/sj.ki.5002231
Sutherland SM, Ji J, Sheikhi FH, Widen E, Tian L, Alexander SR, Ling XB (2013) AKI in hospitalized children: epidemiology and clinical associations in a national cohort. Clin J Am Soc Nephrol 8:1661–1669. https://doi.org/10.2215/cjn.00270113
Sutherland SM, Byrnes JJ, Kothari M, Longhurst CA, Dutta S, Garcia P, Goldstein SL (2015) AKI in hospitalized children: comparing the pRIFLE, AKIN, and KDIGO definitions. Clin J Am Soc Nephrol 10:554–561. https://doi.org/10.2215/cjn.01900214
Fleming GM, Sahay R, Zappitelli M, King E, Askenazi DJ, Bridges BC, Paden ML, Selewski DT, Cooper DS (2016) The incidence of acute kidney injury and its effect on neonatal and pediatric extracorporeal membrane oxygenation outcomes. Pediatr Crit Care Med 17:1157–1169. https://doi.org/10.1097/pcc.0000000000000970
Jetton JG, Boohaker LJ, Sethi SK, Wazir S, Rohatgi S, Soranno DE, Chishti AS, Woroniecki R, Mammen C, Swanson JR, Shanty Sridhar S, Wong CS, Kupferman JC, Griffin RL, Askenazi DJ, Neonatal Kidney Collaborative (NKC) (2017) Incidence and outcomes of neonatal acute kidney injury (AWAKEN): a multicentre, multinational, observational cohort study. Lancet Child Adolesc Heal 1:184–194. https://doi.org/10.1016/s2352-4642(17)30069-x
Fitzgerald JC, Basu RK, Akcan-Arikan A, Izquierdo LM, Piñeres Olave BE, Hassinger AB, Szczepanska M, Deep A, Williams D, Sapru A, Roy JA, Nadkarni VM, Thomas NJ, Weiss SL, Furth S, Sepsis PRevalence, OUtcomes, and Therapies Study Investigators and Pediatric Acute Lung Injury and Sepsis Investigators Network (2016) Acute kidney injury in pediatric severe Sepsis. Crit Care Med 44:2241–2250. https://doi.org/10.1097/ccm.0000000000002007
Fitzgerald JC, Ross ME, Thomas NJ, Weiss SL, Balamuth F, Anderson AH (2018) Risk factors and inpatient outcomes associated with acute kidney injury at pediatric severe sepsis presentation. Pediatr Nephrol 33:1781–1790. https://doi.org/10.1007/s00467-018-3981-8
Hessey E, Morissette G, Lacroix J, Perreault S, Samuel S, Dorais M, Jouvet P, Lafrance JP, LeLorier J, Phan V, Palijan A, Pizzi M, Roy L, Zappitelli M (2018) Long-term mortality after acute kidney injury in the pediatric ICU. Hosp Pediatr 8:260–268. https://doi.org/10.1542/hpeds.2017-0215
Weiss SL, Asaro LA, Flori HR, Allen GL, Wypij D, Curley MA, Randomized Evaluation of Sedation Titration for Respiratory Failure (RESTORE) Study Investigators (2017) Multiple organ dysfunction in children mechanically ventilated for acute respiratory failure. Pediatr Crit Care Med 18:319–329. https://doi.org/10.1097/pcc.0000000000001091
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
None.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Gorga, S.M., Carlton, E.F., Kohne, J.G. et al. Consensus acute kidney injury criteria integration identifies children at risk for long-term kidney dysfunction after multiple organ dysfunction syndrome. Pediatr Nephrol 36, 1637–1646 (2021). https://doi.org/10.1007/s00467-020-04865-0
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00467-020-04865-0