Abstract
Objective
To determine how hypotension in the first 48 h of sepsis management impacts acute kidney injury (AKI) development and persistence.
Study design
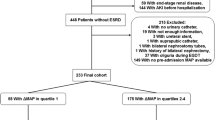
Retrospective study of patients > 1 month to < 20 years old with sepsis in a pediatric ICU between November 2012 and January 2015 (n = 217). All systolic blood pressure (SBP) data documented within 48 h after sepsis recognition were collected and converted to percentiles for age, sex, and height. Time below SBP percentiles and below pediatric advanced life support (PALS) targets was calculated by summing elapsed time under SBP thresholds during the first 48 h. The primary outcome was new or persistent AKI, defined as stage 2 or 3 AKI present between sepsis day 3–7 using Kidney Disease: Improving Global Outcomes creatinine definitions. Secondary outcomes included AKI-free days (days alive and free of AKI) and time to kidney recovery.
Results
Fifty of 217 sepsis patients (23%) had new or persistent AKI. Patients with AKI spent a median of 35 min under the first SBP percentile, versus 4 min in those without AKI. After adjustment for potential confounders, the odds of AKI increased by 9% with each doubling of minutes spent under this threshold (p = 0.03). Time under the first SBP percentile was also associated with fewer AKI-free days (p = 0.02). Time spent under PALS targets was not associated with AKI.
Conclusions
The duration of severe systolic hypotension in the first 48 h of pediatric sepsis management is associated with AKI incidence and duration when defined by age, sex, and height norms, but not by PALS definitions.

Graphical abstract




Similar content being viewed by others
Availability of data and material
The datasets generated and/or analyzed during the current study are not publicly available due to the fact that the authors do not have unrestricted permission from the institution to share these data, but are available from the corresponding author on reasonable request.
Code availability
Statistical analysis is done by custom code with the exception of conversion of systolic blood pressures into z-scores, which is available at https://www.researchgate.net/post/Blood_pressure_percentiles_z-scores_in_STATA.
References
Singer M, Deutschman CS, Seymour CW, Shankar-Hari M, Annane D, Bauer M, Bellomo R, Bernard GR, Chiche JD, Coopersmith CM, Hotchkiss RS, Levy MM, Marshall JC, Martin GS, Opal SM, Rubenfeld GD, van der Poll T, Vincent JL, Angus DC (2016) The third international consensus definitions for sepsis and septic shock (sepsis-3). JAMA 315:801–810. https://doi.org/10.1001/jama.2016.0287
Jaramillo-Bustamante JC, Marin-Agudelo A, Fernandez-Laverde M, Bareno-Silva J (2012) Epidemiology of sepsis in pediatric intensive care units: first Colombian multicenter study. Pediatr Crit Care Med 13:501–508. https://doi.org/10.1097/PCC.0b013e31823c980f
Weiss SL, Fitzgerald JC, Pappachan J, Wheeler D, Jaramillo-Bustamante JC, Salloo A, Singhi SC, Erickson S, Roy JA, Bush JL, Nadkarni VM, Thomas NJ; Sepsis Prevalence, Outcomes, and Therapies (SPROUT) Study Investigators and Pediatric Acute Lung Injury and Sepsis Investigators (PALISI) Network (2015) Global epidemiology of pediatric severe sepsis: the sepsis prevalence, outcomes, and therapies study. Am J Respir Crit Care Med 191:1147–1157. https://doi.org/10.1164/rccm.201412-2323OC
Weiss SL, Parker B, Bullock ME, Swartz S, Price C, Wainwright MS, Goodman DM (2012) Defining pediatric sepsis by different criteria: discrepancies in populations and implications for clinical practice. Pediatr Crit Care Med 13:e219–e226. https://doi.org/10.1097/PCC.0b013e31823c98da
Bagshaw SM, George C, Bellomo R (2008) Early acute kidney injury and sepsis: a multicentre evaluation. Crit Care 12:R47. https://doi.org/10.1186/cc6863
Sanchez-Pinto LN, Goldstein SL, Schneider JB, Khemani RG (2015) Association between progression and improvement of acute kidney injury and mortality in critically ill children. Pediatr Crit Care Med 16:703–710. https://doi.org/10.1097/PCC.0000000000000461
Fitzgerald JC, Basu RK, Akcan-Arikan A, Izquierdo LM, Pineres Olave BE, Hassinger AB, Szczepanska M, Deep A, Williams D, Sapru A, Roy JA, Nadkarni VM, Thomas NJ, Weiss SL, Furth S; Sepsis PRevalence, OUtcomes, and Therapies Study Investigators and Pediatric Acute Lung Injury and Sepsis Investigators Network (2016) Acute kidney injury in pediatric severe sepsis: an independent risk factor for death and new disability. Crit Care Med 44:2241–2250. https://doi.org/10.1097/CCM.0000000000002007
Fitzgerald JC, Ross ME, Thomas NJ, Weiss SL, Balamuth F, Anderson AH (2018) Risk factors and inpatient outcomes associated with acute kidney injury at pediatric severe sepsis presentation. Pediatr Nephrol 33:1781–1790. https://doi.org/10.1007/s00467-018-3981-8
(2012) Kidney Disease: Improving Global Outcomes (KDIGO) Acute Kidney Injury Work Group. KDIGO clinical practice guideline for acute kidney injury. Section 2: AKI Definition. Kidney Int Suppl (2011) 2:19-36. https://doi.org/10.1038/kisup.2011.32
Kaddourah A, Basu RK, Bagshaw SM, Goldstein SL; AWARE Investigators (2017) Epidemiology of acute kidney injury in critically ill children and young adults. N Engl J Med 376:11–20. https://doi.org/10.1056/NEJMoa1611391
de Oliveira CF, de Oliveira DS, Gottschald AF, Moura JD, Costa GA, Ventura AC, Fernandes JC, Vaz FA, Carcillo JA, Rivers EP, Troster EJ (2008) ACCM/PALS haemodynamic support guidelines for paediatric septic shock: an outcomes comparison with and without monitoring central venous oxygen saturation. Intensive Care Med 34:1065–1075. https://doi.org/10.1007/s00134-008-1085-9
Rivers E, Nguyen B, Havstad S, Ressler J, Muzzin A, Knoblich B, Peterson E, Tomlanovich M (2001) Early goal-directed therapy in the treatment of severe sepsis and septic shock. N Engl J Med 345:1368–1377. https://doi.org/10.1056/NEJMoa010307
Davis AL, Carcillo JA, Aneja RK, Deymann AJ, Lin JC, Nguyen TC, Okhuysen-Cawley RS, Relvas MS, Rozenfeld RA, Skippen PW, Stojadinovic BJ, Williams EA, Yeh TS, Balamuth F, Brierley J, de Caen AR, Cheifetz IM, Choong K, Conway E Jr, Cornell T, Doctor A, Dugas MA, Feldman JD, Fitzgerald JC, Flori HR, Fortenberry JD, Graciano AL, Greenwald BM, Hall MW, Han YY, Hernan LJ, Irazuzta JE, Iselin E, van der Jagt EW, Jeffries HE, Kache S, Katyal C, Kissoon NT, Kon AA, Kutko MC, MacLaren G, Maul T, Mehta R, Odetola F, Parbuoni K, Paul R, Peters MJ, Ranjit S, Reuter-Rice KE, Schnitzler EJ, Scott HF, Torres A Jr, Weingarten-Abrams J, Weiss SL, Zimmerman JJ, Zuckerberg AL (2017) American College of Critical Care Medicine Clinical Practice Parameters for Hemodynamic Support of Pediatric and Neonatal Septic Shock. Crit Care Med 45:1061–1093. https://doi.org/10.1097/CCM.0000000000002425
Kleinman ME, Chameides L, Schexnayder SM, Samson RA, Hazinski MF, Atkins DL, Berg MD, de Caen AR, Fink EL, Freid EB, Hickey RW, Marino BS, Nadkarni VM, Proctor LT, Qureshi FA, Sartorelli K, Topjian A, van der Jagt EW, Zaritsky AL (2010) Part 14: pediatric advanced life support: 2010 American Heart Association guidelines for cardiopulmonary resuscitation and emergency cardiovascular care. Circulation 122:S876–S908. https://doi.org/10.1161/CIRCULATIONAHA.110.971101
Marlais M, Lyttle MD, Inwald D (2017) Ten concerns about blood pressure measurement and targets in paediatric sepsis. Intensive Care Med 43:433–435. https://doi.org/10.1007/s00134-016-4642-7
Abdelrazeq S, Ray S, Rogers L, Noren DP, Peters MJ, Inwald DP (2018) Age-associated blood pressure distributions in paediatric intensive care units differ from healthy children. Intensive Care Med 44:384–386. https://doi.org/10.1007/s00134-017-5017-4
Weiss SL, Peters MJ, Alhazzani W, Agus MSD, Flori HR, Inwald DP, Nadel S, Schlapbach LJ, Tasker RC, Argent AC, Brierley J, Carcillo J, Carrol ED, Carroll CL, Cheifetz IM, Choong K, Cies JJ, Cruz AT, De Luca D, Deep A, Faust SN, De Oliveira CF, Hall MW, Ishimine P, Javouhey E, Joosten KFM, Joshi P, Karam O, Kneyber MCJ, Lemson J, MacLaren G, Mehta NM, Moller MH, Newth CJL, Nguyen TC, Nishisaki A, Nunnally ME, Parker MM, Paul RM, Randolph AG, Ranjit S, Romer LH, Scott HF, Tume LN, Verger JT, Williams EA, Wolf J, Wong HR, Zimmerman JJ, Kissoon N, Tissieres P (2020) Surviving Sepsis Campaign International guidelines for the management of septic shock and sepsis-associated organ dysfunction in children. Pediatr Crit Care Med 21:e52–e106. https://doi.org/10.1097/PCC.0000000000002198
Lamontagne F, Richards-Belle A, Thomas K, Harrison DA, Sadique MZ, Grieve RD, Camsooksai J, Darnell R, Gordon AC, Henry D, Hudson N, Mason AJ, Saull M, Whitman C, Young JD, Rowan KM, Mouncey PR; 65 trial investigators (2020) Effect of reduced exposure to vasopressors on 90-day mortality in older critically ill patients with vasodilatory hypotension: a randomized clinical trial. JAMA. https://doi.org/10.1001/jama.2020.0930
Poukkanen M, Wilkman E, Vaara ST, Pettila V, Kaukonen KM, Korhonen AM, Uusaro A, Hovilehto S, Inkinen O, Laru-Sompa R, Hautamaki R, Kuitunen A, Karlsson S (2013) Hemodynamic variables and progression of acute kidney injury in critically ill patients with severe sepsis: data from the prospective observational FINNAKI study. Crit Care 17:R295. https://doi.org/10.1186/cc13161
Deep A, Sagar H, Goonasekera C, Karthikeyan P, Brierley J, Douiri A (2018) Evolution of acute kidney injury and its association with systemic hemodynamics in children with fluid-refractory septic shock. Crit Care Med 46:e677–e683. https://doi.org/10.1097/CCM.0000000000003156
Goldstein B, Giroir B, Randolph A (2005) International pediatric sepsis consensus conference: definitions for sepsis and organ dysfunction in pediatrics. Pediatr Crit Care Med 6:2–8. https://doi.org/10.1097/01.PCC.0000149131.72248.E6
Feudtner C, Hays RM, Haynes G, Geyer JR, Neff JM, Koepsell TD (2001) Deaths attributed to pediatric complex chronic conditions: national trends and implications for supportive care services. Pediatrics 107:E99. https://doi.org/10.1542/peds.107.6.e99
Balamuth F, Weiss SL, Fitzgerald JC, Hayes K, Centkowski S, Chilutti M, Grundmeier RW, Lavelle J, Alpern ER (2016) Protocolized treatment is associated with decreased organ dysfunction in pediatric severe sepsis. Pediatr Crit Care Med 17:817–822. https://doi.org/10.1097/PCC.0000000000000858
Han M, Fitzgerald JC, Balamuth F, Keele L, Alpern ER, Lavelle J, Chilutti M, Grundmeier RW, Nadkarni VM, Thomas NJ, Weiss SL (2017) Association of delayed antimicrobial therapy with one-year mortality in pediatric sepsis. Shock 48:29–35. https://doi.org/10.1097/SHK.0000000000000833
Weiss SL, Fitzgerald JC, Balamuth F, Alpern ER, Lavelle J, Chilutti M, Grundmeier R, Nadkarni VM, Thomas NJ (2014) Delayed antimicrobial therapy increases mortality and organ dysfunction duration in pediatric sepsis. Crit Care Med 42:2409–2417. https://doi.org/10.1097/CCM.0000000000000509
Slater A, Shann F, Pearson G (2003) PIM2: a revised version of the paediatric index of mortality. Intensive Care Med 29:278–285. https://doi.org/10.1007/s00134-002-1601-2
Topjian AA, French B, Sutton RM, Conlon T, Nadkarni VM, Moler FW, Dean JM, Berg RA (2014) Early postresuscitation hypotension is associated with increased mortality following pediatric cardiac arrest. Crit Care Med 42:1518–1523. https://doi.org/10.1097/CCM.0000000000000216
Rosner B (2018) Pediatric Blood Pressure. https://sites.google.com/a/channing.harvard.edu/bernardrosner/pediatric-blood-press. Accessed Oct 3 2018
Bruun S (2018) Blood pressure percentiles (z-scores) in STATA. https://www.researchgate.net/post/Blood_pressure_percentiles_z-scores_in_STATA. Accessed Oct 3 2018
McIntosh AM, Tong S, Deakyne SJ, Davidson JA, Scott HF (2017) Validation of the vasoactive-inotropic score in pediatric sepsis. Pediatr Crit Care Med 18:750–757. https://doi.org/10.1097/PCC.0000000000001191
Schwartz GJ, Munoz A, Schneider MF, Mak RH, Kaskel F, Warady BA, Furth SL (2009) New equations to estimate GFR in children with CKD. J Am Soc Nephrol 20:629–637. https://doi.org/10.1681/ASN.2008030287
Zappitelli M, Parikh CR, Akcan-Arikan A, Washburn KK, Moffett BS, Goldstein SL (2008) Ascertainment and epidemiology of acute kidney injury varies with definition interpretation. Clin J Am Soc Nephrol 3:948–954. https://doi.org/10.2215/CJN.05431207
Hessey E, Ali R, Dorais M, Morissette G, Pizzi M, Rink N, Jouvet P, Lacroix J, Phan V, Zappitelli M (2017) Renal function follow-up and renal recovery after acute kidney injury in critically ill children. Pediatr Crit Care Med 18:733–740. https://doi.org/10.1097/PCC.0000000000001166
Schetz M, Gunst J, De Vlieger G, Van den Berghe G (2015) Recovery from AKI in the critically ill: potential confounders in the evaluation. Intensive Care Med 41:1648–1657. https://doi.org/10.1007/s00134-015-3946-3
Fine JP, Gray RJ (1999) A proportional hazards model for the subdistribution of a competing risk. J Am Stat Assoc 94:496–509. https://doi.org/10.1080/01621459.1999.10474144
Funding
This study was supported by the Division of Critical Care Medicine Russell Raphaely, endowed chair of Critical Care Medicine at the Children’s Hospital of Philadelphia. Dr. Fitzgerald was supported by the National Institutes of Health [grant number R43-HD096961]. Dr. Weiss was supported by the National Institutes of Health [grant number K23-GM110496]. Dr. Balamuth was supported by the National Institutes of Health [grant number K23-HD082368]. Dr. Anderson is supported by the National Institutes of Health [grant numbers R01-DK104730 and R01-DK107566] and has received travel and consulting fees from Kyowa Hakko Kirin.
Author information
Authors and Affiliations
Contributions
All authors contributed to the study conception and design. Material preparation, data collection, and data validation were performed by Julie Fitzgerald, Scott Weiss, Fran Balamuth, Marianne Chilutti, and Robert Grundmeier. Analysis was performed by Julie Fitzgerald under the supervision of Michelle Ross. Supervision of the project was performed by Michelle Ross, Neal Thomas, and Amanda Anderson. The first draft of the manuscript was written by Julie Fitzgerald, and all authors commented on the previous version of the manuscript. All authors read and approved the final manuscript. All authors agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Corresponding author
Ethics declarations
Conflict of interest/competing interests
For the remaining authors, no conflicts of interest were declared.
Ethics approval
The study was approved by the Children’s Hospital of Philadelphia Institutional Review Board with a waiver of informed consent given the retrospective, observational nature of this epidemiologic study. The study was performed in accordance with ethical standards as laid down in the 1964 Declaration of Helsinki and its later amendments.
Consent to participate
A waiver of informed consent was granted given the retrospective, observational nature of this epidemiologic study.
Consent for publication
As a waiver of informed consent was granted, the consent for publication was not sought. No individually identifying information is included in this manuscript.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Fitzgerald, J.C., Ross, M.E., Thomas, N.J. et al. Association of early hypotension in pediatric sepsis with development of new or persistent acute kidney injury. Pediatr Nephrol 36, 451–461 (2021). https://doi.org/10.1007/s00467-020-04704-2
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00467-020-04704-2