Abstract
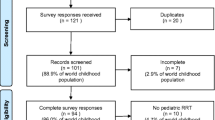
With migration rising, the pediatric nephrology community is faced with challenges concerning the management of end-stage kidney disease (ESKD) in the pediatric refugee population. Data on the care of the pediatric refugee cohort on renal replacement therapy (RRT) is not available. A survey conducted by us in 2018 showed that the group of refugee children arriving to Germany during the years 2015–2017 accounts for approximately 20% of the total pediatric dialysis population in Germany. Provision of (medical) care for these children and their families is often hampered by psychosocial problems, cultural differences, language barriers, and administrative issues. Treating centers need to provide additional human as well as financial and logistic resources. In this educational review, we raise awareness and discuss possible challenges occurring in the treatment of refugee children with ESKD.
Similar content being viewed by others
References
(2018) Migration and migration populations statistic. Eurostat.
UNICEF (2016) Zur Situation der Flüchtlingskinder in Deutschland. In: Bücker K (ed).
BAMF, Bundesamt für Migration und Flüchtlinge (2018) Das Bundesamt in Zahlen 2017. Nürnberg.
Van Biesen W, Vanholder R, Vanderhaegen B, Lameire N, Wanner C, Wiecek A, Sever MS, Feehally J, Kazancioglu R, Rondeau E, Levin A, Harris D (2016) Renal replacement therapy for refugees with end-stage kidney disease: an international survey of the nephrological community. Kidney Int Suppl 6:35–41
Mockenhaupt FP, Barbre KA, Jensenius M, Larsen CS, Barnett ED, Stauffer W, Rothe C, Asgeirsson H, Hamer DH, Esposito DH, Gautret P, Schlagenhauf P (2016) Profile of illness in Syrian refugees: a GeoSentinel analysis, 2013 to 2015. Euro Surveill 21:30160
Spallek J, Tempes J, Ricksgers H, Marquardt L, Prufer-Kramer L, Kramer A (2016) The health situation and health care needs of unaccompanied minor refugees - an approximation based on qualitative and quantitative studies from Bielefeld, Germany. Bundesgesundheitsblatt Gesundheitsforschung Gesundheitsschutz 59:636–641
KfH, Kuratorium für Dialyse und Nierentransplantation (2018) Jahresbericht 2017. Neu-Isenburg, pp 25-26
John-Baptiste A, Naglie G, Tomlinson G, Alibhai SM, Etchells E, Cheung A, Kapral M, Gold WL, Abrams H, Bacchus M, Krahn M (2004) The effect of English language proficiency on length of stay and in-hospital mortality. J Gen Intern Med 19:221–228
Lee ED, Rosenberg CR, Sixsmith DM, Pang D, Abularrage J (1998) Does a physician-patient language difference increase the probability of hospital admission? Acad Emerg Med 5:86–89
LeSon S, Gershwin ME (1995) Risk factors for asthmatic patients requiring intubation. I. Observations in children. J Asthma 32:285–294
Flores G (2005) The impact of medical interpreter services on the quality of health care: a systematic review. Med Care Res Rev 62:255–299
Karliner LS, Jacobs EA, Chen AH, Mutha S (2007) Do professional interpreters improve clinical care for patients with limited English proficiency? A systematic review of the literature. Health Serv Res 42:727–754
Brandl EJ, Schreiter S, Schouler-Ocak M (2019) Are trained medical interpreters worth the cost? A review of the current literature on cost and cost-effectiveness. J Immigr Minor Health. https://doi.org/10.1007/s10903-019-00915-4
Jha V, Chugh KS (2003) The practice of dialysis in the developing countries. Hemodial Int 7:239–249
Sever M, Sever L, Vanholder R (2019) Disasters, children and the kidneys. Pediatr Nephrol. https://doi.org/10.1007/s00467-019-04310-x
Saeed B (2011) Development of solid organ transplantation in syria. Int J Organ Transplant Med 2:40–46
Isreb MA, Kaysi S, Rifai AO, Al Kukhun H, Al-Adwan SAS, Kass-Hout TA, Sekkarie MA (2017) The effect of war on syrian refugees with end-stage renal disease. Kidney Int Rep 2:960–963
Saeed MB, Sherif S (2005) Pediatric renal transplantation in syria: a single center experience. Saudi J Kidney Dis Transpl 16:342–347
Harambat J, van Stralen KJ, Kim JJ, Tizard EJ (2012) Epidemiology of chronic kidney disease in children. Pediatr Nephrol 27:363–373
Kari JA (2006) Chronic renal failure in children in the Western area of saudi arabia. Saudi J Kidney Dis Transpl 17:19–24
Akbalik Kara M, Demircioglu Kilic B, Col N, Ozcelik AA, Buyukcelik M, Balat A (2017) Kidney disease profile of Syrian refugee children. Iran J Kidney Dis 11:109–114
Ladapo TA, Esezobor CI, Lesi FE (2014) Pediatric kidney diseases in an African country: prevalence, spectrum and outcome. Saudi J Kidney Dis Transpl 25:1110–1116
Michael IO, Gabriel OE (2003) Pattern of renal diseases in children in midwestern zone of Nigeria. Saudi J Kidney Dis Transpl 14:539–544
Arogundade FA, Hassan MO, Omotoso BA, Oguntola SO, Okunola OO, Sanusi AA, Akinsola A (2016) Spectrum of kidney diseases in Africa: malaria, schistosomiasis, sickle cell disease, and toxins. Clin Nephrol 86:53–60
Hamamy H (2012) Consanguineous marriages: preconception consultation in primary health care settings. J Community Genet 3:185–192
Ozdemir FN, Akçay A, Elsurer R, Sezer S, Arat Z, Haberal M (2005) Interdialytic weight gain is less with the Mediterranean type of diet in hemodialysis patients. J Ren Nutr 15:371–376
D’Alessandro C, Piccoli GB, Cupisti A (2015) The “phosphorus pyramid”: a visual tool for dietary phosphate management in dialysis and CKD patients. BMC Nephrol 16:9
Einollahi B, Shahyad S, Lotfiazar A (2017) Re: Clinical and biochemical parameters of hemodialysis patients before and during the Islamic Ramadan month. Iran J Kidney Dis 11:168
Alshamsi S, Binsaleh F, Hejaili F, Karkar A, Moussa D, Raza H, Parbat P, Al Suwida A, Alobaili S, AlSehli R, Al Sayyari A (2016) Changes in biochemical, hemodynamic, and dialysis adherence parameters in hemodialysis patients during Ramadan. Hemodial Int 20:270–276
Imtiaz S, Nasir K, Dhrolia MF, Hussain M, Abbas HN, Ahmad A (2015) Mortality trend among hemodialysis patients during the islamic month of Ramadan: a 24 years retrospective study. J Coll Physicians Surg Pak 25:189–192
Al Wakeel JS (2014) Kidney function and metabolic profile of chronic kidney disease and hemodialysis patients during Ramadan fasting. Iran J Kidney Dis 8:321–328
Hejaili F, Qurashi S, Binsalih S, Jaradt M, Al Sayyari A (2014) Effect of repeated ramadan fasting in the hottest months of the year on renal graft function. Nephrourol Mon 6:e14362
Einollahi B, Lessan-Pezeshki M, Simforoosh N, Nafar M, Pour-Reza-Gholi F, Firouzan A, Khatami MR, Nourbala MH, Pourfarzini V (2005) Impact of Ramadan fasting on renal allograft function. Transplant Proc 37:3004–3005
Vasavi Chandrika M, Vijaya Krishna M, Jyothirmayi T, Ankamma Naidu V, Manikanta swamy V (2016) Alternatives for gelatin in the preperation of capsules. Adv J Pharm Life Sci Res 4:33-42
Oladzadabbasabadi N, Ebadi S, Mohammadi Nafchi A, Karim AA, Kiahosseini SR (2017) Functional properties of dually modified sago starch/kappa-carrageenan films: an alternative to gelatin in pharmaceutical capsules. Carbohydr Polym 160:43–51
Bundesärztekammer Grundsätze zur Aufnahme von Flüchtlingen und Asylbewerbern in die Warteliste zur Organtransplantation in Deutschland.
Takemoto SK, Terasaki PI, Gjertson DW, Cecka JM (2000) Twelve years’ experience with national sharing of HLA-matched cadaveric kidneys for transplantation. N Engl J Med 343:1078–1084
Bryan CF, Harrell KM, Mitchell SI, Warady BA, Aeder MI, Luger AM, Murillo D, Muruve NA, Nelson PW, Shield CF (2003) HLA points assigned in cadaveric kidney allocation should be revisited: an analysis of HLA class II molecularly typed patients and donors. Am J Transplant 3:459–464
Cantrelle C, Laurens C, Luciolli E, Loty B, Tuppin P (2006) Access to kidney transplantation in France of non-French patients and French patients living in overseas territories. Transplantation 81:1147–1152
Jakobsen M, Demott MA, Heir T (2014) Prevalence of psychiatric disorders among unaccompanied asylum-seeking adolescents in norway. Clin Pract Epidemiol Ment Health 10:53–58
Ruf M, Schauer M, Elbert T (2010) Prävalenz von traumatischen Stresserfahrungen und seelischen Erkrankungen bei in Deutschland lebenden Kindern von Asylbewerbern. Z Klin Psychol Psychother 39:151–160
Eurostat (2018) Asylum applicants considered to be unaccompanied minors by citizenship, age and sex Annual data. European Union.
Norredam M, Nellums L, Nielsen RS, Byberg S, Petersen JH (2018) Incidence of psychiatric disorders among accompanied and unaccompanied asylum-seeking children in Denmark: a nation-wide register-based cohort study. Eur Child Adolesc Psychiatry 27:439–446
Flüchtlinge BfMu (2018) Das Bundesamt in Zahlen 2017. Nürnberg.
Acknowledgments
Members of the German Society of Pediatric Nephrology (GPN) are the following: Heiko Billing, Rainer Büscher, Martin Feldkötter, Dieter Haffner, Matthias Hansen, Martin Holder, Bernd Hoppe, Ulrike John, Günter Klaus, Carmen Montoya, Martin Pohl, Bettina Ruckenbrod, Franz Schaefer, Monika Schimmel, Hagen Staude, Christina Taylan, Lutz Weber, Simone Wygoda
Author information
Authors and Affiliations
Consortia
Corresponding author
Ethics declarations
Conflict of interests
The authors declare that they have no conflict of interest
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Multiple choice questions (answers follow reference list)
Multiple choice questions (answers follow reference list)
-
1.
How large was the proportion of refugee children in the group of dialyzed children in Germany in the year 2017?
-
a)
5%
-
b)
22%
-
c)
37%
-
d)
12%
-
a)
-
2.
What are the most common countries of origin among refugee children on RRT in Germany?
-
a)
Iraq, Eritrea, Afghanistan
-
b)
Afghanistan, Syria, Somalia
-
c)
Syria, Libya, Afghanistan
-
d)
Syria, Iraq, Afghanistan
-
a)
-
3.
How large is the proportion of patients on PD in the group of ESKD patients in Syria?
-
a)
4%
-
b)
27%
-
c)
35%
-
d)
16%
-
a)
-
4.
According to some studies, what is the most common cause of CKD in Cameroon and Nigeria?
-
a)
CAKUT
-
b)
Tubulopathies
-
c)
Glomerular disease
-
d)
Cystic kidney disease
-
a)
-
5.
What percentage of the world’s population is practicing consanguinity?
-
a)
20%
-
b)
14%
-
c)
47%
-
d)
24%
-
a)
1. b) 22%; 2. d) Syria, Iraq, Afghanistan; 3. a) 4%; 4. c) Glomerular disease; 5. a) 20%
Rights and permissions
About this article
Cite this article
Lemke, J., Schild, R., Konrad, M. et al. Distribution and management of the pediatric refugee population with renal replacement: A German pediatric cohort. Pediatr Nephrol 36, 271–277 (2021). https://doi.org/10.1007/s00467-019-04374-9
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00467-019-04374-9