Abstract
Objective
To evaluate whether grade 4–5 vesicoureteral reflux (VUR) can be predicted from renal ultrasound (RUS) findings and perform voiding cystourethrograms (VCUGs) only on high-risk patients.
Methods
The RUS and VCUG images of infants with prenatally detected hydronephrosis admitted to our institution between 2003 and 2013 were re-evaluated. The UTI episodes were collected retrospectively from patient journals. Patients with complex urinary tract anomalies were excluded.
Results
One hundred eighty, 44 female and 136 male, patients (352 renal units (RU)), 23 (30 RU) of them having grade 4–5 VUR, were included. The median age of the patients at the time of the RUS was 1.3 (0.1–3.0) months and the median follow-up time was 2.0 (0.1–11.2) years.
In multivariate analysis, a visible ureter (OR 12.72; CI 5.33–32.04, p < 0.001) and shorter renal length (OR 2.67; CR 1.50–4.86, p < 0.001) in RUS predicted grade 4–5 VUR while a visible ureter predicted UTIs (OR 5.75; CI 2.59–12.66, p < 0.001).
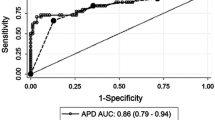
A three-grade risk score for high-grade VUR was developed based on the RUS findings and the patients were categorized into low-, intermediate-, and high-risk groups. The incidence of grade 4–5 VUR was 2.9% in the low-risk, 12.2% in the intermediate-risk, and 52.2% in the high-risk group. The sensitivity and specificity for detecting grade 4–5 VUR were 79 and 82%, respectively.
Conclusions
In patients with antenatally detected hydronephrosis, a visible ureter and reduced renal length in RUS are significant risk factors for high-grade VUR. A RUS-based risk scoring would probably reduce the proportion of unnecessary VCUGs.

Similar content being viewed by others
Change history
15 June 2018
The original publication contained an erroneous version of Table 3 with incorrect data regarding ureteral visibility. The authors apologize for any inconvenience caused by their mistake and are pleased to present the corrected table here.
References
Ek S, Lidefeldt KJ, Varricio L (2007) Fetal hydronephrosis; prevalence, natural history and postnatal consequences in an unselected population. Acta Obstet Gynecol Scand 86:1463–1466
Hamilton BE, Martin JA, Ventura SJ (2013) Births: preliminary data for 2012. Natl Vital Stat Rep 62:1–20
Feldman DM, DeCambre M, Kong E, Borgida A, Jamil M, McKenna P, Egan JF (2001) Evaluation and follow-up of fetal hydronephrosis. J Ultrasound Med 20:1065–1069
Phan V, Traubici J, Hershenfield B, Stephens D, Rosenblum ND, Geary DF (2003) Vesicoureteral reflux in infants with isolated antenatal hydronephrosis. Pediatr Nephrol 18:1224–1228
Brophy MM, Austin PF, Yan Y, Coplen DE (2002) Vesicoureteral reflux and clinical outcomes in infants with prenatally detected hydronephrosis. J Urol 168(4 Pt 2):1716–1719 discussion 1719
Evans K, Asimakadou M, Nwankwo O, Desai D, Cherian A, Mushtaq I, Cuckow P, Duffy P, Smeulders N (2015) What is the risk of urinary tract infection in children with antenatally presenting dilating vesico-ureteric reflux? J Pediatr Urol 11:93.e1–93.93.e6
Nordenström J, Sjöström S, Sillén U, Sixt R, Brandström P (2017) The Swedish infant high-grade reflux trial: UTI and renal damage. J Pediatr Urol 13:146–154
Lee RS, Cendron M, Kinnamon DD, Nguyen HT (2006) Antenatal hydronephrosis as a predictor of postnatal outcome: a meta-analysis. Pediatrics 118:586–593
St Aubin M, Willihnganz-Lawson K, Varda BK, Fine M, Adejoro O, Prosen T, Lewis JM, Shukla AR (2013) Society for fetal urology recommendations for postnatal evaluation of prenatal hydronephrosis—will fewer voiding cystourethrograms lead to more urinary tract infections? J Urol 190:1456–1461
Nguyen HT, Herndon CD, Cooper C, Gatti J, Kirsch A, Kokorowski P, Lee R, Perez-Brayfield M, Metcalfe P, Yerkes E, Cendron M, Campbell JB (2010) The Society for Fetal Urology consensus statement on the evaluation and management of antenatal hydronephrosis. J Pediatr Urol 6:212–231
Nguyen HT, Benson CB, Bromley B, Campbell JB, Chow J, Coleman B, Cooper C, Crino J, Darge K, Herndon CD, Odibo AO, Somers MJ, Stein DR (2014) Multidisciplinary consensus on the classification of prenatal and postnatal urinary tract dilation (UTD classification system). J Pediatr Urol 10:982–998
Smans K, Vaño E, Sanchez R, Schultz FW, Zoetelief J, Kiljunen T, Maccia C, Järvinen H, Bly R, Kosunen A, Faulkner K, Bosmans H (2008) Results of a European survey on patient doses in paediatric radiology. Radiat Prot Dosim 129:204–210
Schneider K, Krüger-Stollfuss I, Ernst G, Kohn MM (2001) Paediatric fluoroscopy—a survey of children’s hospitals in Europe I Staffing, frequency of fluoroscopic procedures and investigation technique. Pediatr Radiol 31:238–246
Visuri S, Jahnukainen T, Taskinen S (2017) Incidence of urinary tract infections in infants with antenatally diagnosed hydronephrosis—a retrospective single center study. J Pediatr Surg 52:1503–1506
Rachmiel M, Aladjem M, Starinsky R (2005) Symptomatic urinary tract infections following voiding cystourethrography. Pediatr Nephrol 20:1449–1452
Lebowitz RL, Olbing H, Parkkulainen KV, Smellie JM, Tamminen-Möbius TE (1985) International system of radiographic grading of vesicoureteric reflux. International Reflux Study in Children. Pediatr Radiol 15:105–109
Fernbach SK, Maizels M, Conway JJ (1993) Ultrasound grading of hydronephrosis: introduction to the system used by the Society for Fetal Urology. Pediatr Radiol 23:478–480
Honkinen O, Jahnukainen T, Mertsola J, Eskola J, Ruuskanen O (2000) Bacteremic urinary tract infection in children. Pediatr Infect Dis J 19:630–634
Han K, Song K, Choi BW (2016) How to develop, validate, and compare clinical prediction models involving radiological parameters: study design and statistical methods. Korean J Radiol 17:339–350
Moriya K, Mitsui T, Kitta T (2015) Early discontinuation of antibiotic prophylaxis in patients with persistent primary vesicoureteral reflux initially detected during infancy: outcome analysis and risk factors for febrile urinary tract infection. J Urol 193:637–642
Park S, Song SH, Lee C, Kim JW, Kim KS (2013) Bacterial pathogens in first febrile urinary tract infection affect breakthrough infections in infants with vesicoureteral reflux treated with prophylactic antibiotics. Urology 81:1342–1345
Zerin JM, Ritchey ML, Chang AC (1993) Incidental vesicoureteral reflux in neonates with antenatally detected hydronephrosis and other renal abnormalities. Radiology 187:157–160
Gloor JM, Ramsey PS, Ogburn Jr PL, Danilenko-Dixon DR, DiMarco CS, Ramin KD (2002) The association of isolated mild fetal hydronephrosis with postnatal vesicoureteral reflux. J Matern Fetal Neonatal Med 12:196–200
Ismaili K, Avni FE, Hall M (2002) Results of systematic voiding cystourethrography in infants with antenatally diagnosed renal pelvis dilation. J Pediatr 141:21–24
Lidefelt K-J, Ek S, Mihocsa L (2006) Is screening for vesicoureteral reflux mandatory in infants with antenatal renal pelvis dilatation. Acta Paediatr 95:1653–1656
Gordon ZN, McLeod DJ, Ching CB, Herz DB, Bates DG, Becknell B, Alpert SA (2016) Uroepithelial thickening improves detection of vesicoureteral reflux in infants with prenatal hydronephrosis. J Pediatr Urol 12:257e1–257e7
Muensterer OJ (2002) Comprehensive ultrasound versus voiding cysturethrography in the diagnosis of vesicoureteral reflux. Eur J Pediatr 161:435–437
Sencan A, Darvas F, Hekimoglu IC, Caf N, Sencan A, Chow J, Nguyen HT (2014) Urinary tract infection and vesicoureteral reflux in children with mild antenatal hydronephrosis. J Ped Urol 10:1008–1013
Acknowledgments
We would like to thank Mitja Lääperi, M.Sc., for the biostatistical expertise in our study.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
The study protocol was approved by the ethics committee at Helsinki University Hospital.
Conflict of interest
The authors declare that they have no conflict of interest.
Rights and permissions
About this article
Cite this article
Visuri, S., Kivisaari, R., Jahnukainen, T. et al. Postnatal imaging of prenatally detected hydronephrosis—when is voiding cystourethrogram necessary?. Pediatr Nephrol 33, 1751–1757 (2018). https://doi.org/10.1007/s00467-018-3938-y
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00467-018-3938-y