Abstract
Background
Bone impairment appears to be a novel complication of nephropathic cystinosis despite cysteamine therapy. Its exact underlying pathophysiology is nevertheless unclear. The objective of this study was to evaluate bone status among patients included in the French Crystobs study.
Methods
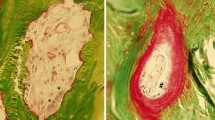
In addition to clinical data, bone status was evaluated using biomarkers (ALP, PTH, 25-D, 1-25D, FGF23), DXA (spine and total body), and high-resolution peripheral quantitative computed tomography (HR-pQCT) at the tibia and radius. Results were compared to age- and gender-matched healthy controls (1:2 basis) from the local reference cohorts.
Results
At a median age of 22.5 (10.2–34.6) years, 10 patients with nephropathic cystinosis were included (2 receiving conservative therapies, 2 undergoing hemodialysis, 6 with a past of renal transplantation); 7 out of 10 patients complained of a bone symptom (past of fracture, bone deformations, and/or bone pain). Biochemicals and spine DXA did not show any significant abnormalities. Using HR-pQCT, significant decreases in cortical parameters (e.g., cortical thickness 850 (520–1100) versus 1225 (480–1680) μm; p < 0.05) and total volumetric bone mineral density (290 (233–360) versus 323 (232–406) mg/cm3; p < 0.05) were observed in cystinotic patients in comparison to controls at the tibia. There were no differences for trabecular parameters. Similar results were observed at the radius.
Conclusions
In this pilot study, bone impairment (rather cortical than trabecular) is a significant clinical problem in nephropathic cystinosis; 70% of patients displayed significant bone symptoms, during teenage or young adulthood. This new complication should be known by physicians because of its potential dramatic impact on quality of life.
Similar content being viewed by others
References
Nesterova G, Gahl WA (2013) Cystinosis: the evolution of a treatable disease. Pediatr Nephrol 28(1):51–59
Bertholet-Thomas A, Bacchetta J, Tasic V, Cochat P (2014) Nephropathic cystinosis: a gap between developing and developed nations. N Engl J Med 370(14):1366–1367
Klusmann M, Van’t Hoff W, Monsell F, Offiah AC (2013) Progressive destructive bone changes in patients with cystinosis. Skelet Radiol 43:387–391
Sirrs S, Munk P, Mallinson PI, Ouellette H, Horvath G, Cooper S, Da Roza G, Rosenbaum D, O'Riley M, Nussbaumer G, Hoang LN, Lee CH (2014) Cystinosis with sclerotic bone lesions. JIMD Rep 13:27–31
Bacchetta J, Greco M, Bertholet-Thomas A, Nobili F, Zustin J, Cochat P, Emma F, Boivin G (2016) Skeletal implications and management of cystinosis: three case reports and literature review. BoneKEy Rep 5:828
Langman CB (2017) Bone complications of cystinosis. J Pediatr 183S:S2–S4
Besouw MTP, Schneider J, Janssen MC, Greco M, Emma F, Cornelissen EA, Desmet K, Skovby F, Nobili F, Lilien MR, De Paepe A, Malfait F, Symoens S, van den Heuvel LP, Levtchenko EN (2013) Copper deficiency in patients with cystinosis with cysteamine toxicity. J Pediatr 163(3):754–760
Besouw MTP, Bowker R, Dutertre J-P, Emma F, Gahl WA, Greco M, Lilien MR, McKiernan J, Nobili F, Schneider JA, Skovby F, van den Heuvel LP, Van’t Hoff WG, Levtchenko EN (2011) Cysteamine toxicity in patients with cystinosis. J Pediatr 159(6):1004–1011
Cherqui S, Sevin C, Hamard G, Kalatzis V, Sich M, Pequignot MO, Gogat K, Abitbol M, Broyer M, Gubler MC, Antignac C (2002) Intralysosomal cystine accumulation in mice lacking cystinosin, the protein defective in cystinosis. Mol Cell Biol 22(21):7622–7632
Claramunt-Taberner D, Flammier S, Gaillard S, Cochat P, Peyruchaud O, Machuca-Gayet I, Bacchetta J (2018) Bone disease in nephropathic cystinosis is related to cystinosin-induced osteoclastic dysfunction. Nephrol Dial Transplant. https://doi.org/10.1093/ndt/gfx362
Dohil R, Rioux P (2013) Pharmacokinetic studies of cysteamine bitartrate delayed-release. Clin Pharmacol Drug Dev 2(2):178–185
Ardeshirpour L, Cole DEC, Carpenter TO (2007) Evaluation of bone and mineral disorders. Pediatr Endocrinol Rev 5(Suppl 1):584–598
Bacchetta J, Boutroy S, Vilayphiou N, Ranchin B, Fouque-Aubert A, Basmaison O, Cochat P (2011) Bone assessment in children with chronic kidney disease: data from two new bone imaging techniques in a single-center pilot study. Pediatr Nephrol 26(4):587–595
Szulc P, Boutroy S, Vilayphiou N, Schoppet M, Rauner M, Chapurlat R, Hamann C, Hofbauer LC (2013) Correlates of bone microarchitectural parameters and serum sclerostin levels in men: the STRAMBO study. J Bone Miner Res 28(8):1760–1770
Sornay-Rendu E, Karras-Guillibert C, Munoz F, Claustrat B, Chapurlat RD (2012) Age determines longitudinal changes in body composition better than menopausal and bone status: the OFELY study. J Bone Miner Res 27(3):628–636
Groothoff JW, Offringa M, Van Eck-Smit BLF, Gruppen MP, Van De Kar NJ, Wolff ED, Lilien MR, Davin JC, Heymans HS, Dekker FW (2003) Severe bone disease and low bone mineral density after juvenile renal failure. Kidney Int 63(1):266–275
Denburg MR, Kumar J, Jemielita T, Brooks ER, Skversky A, Portale AA, Salusky IB, Warady BA, Furth SL, Leonard MB (2016) Fracture burden and risk factors in childhood CKD: results from the CKiD cohort study. J Am Soc Nephrol 27(2):543–550
Nikkel LE, Mohan S, Zhang A, McMahon DJ, Boutroy S, Dube G, Tanriover B, Cohen D, Ratner L, Hollenbeak CS, Leonard MB, Shane E, Nickolas TL (2012) Reduced fracture risk with early corticosteroid withdrawal after kidney transplant. Am J Transplant 12(3):649–659
Zimakas PJA, Sharma AK, Rodd CJ (2003) Osteopenia and fractures in cystinotic children post renal transplantation. Pediatr Nephrol 18(4):384–390
Trauner D (2017) Neurocognitive complications of cystinosis. J Pediatr 183S:S15–S18
Emma F, Nesterova G, Langman C, Labbé A, Cherqui S, Goodyer P, Janssen MC, Greco M, Topaloglu R, Elenberg E, Dohil R, Trauner D, Antignac C, Cochat P, Kaskel F, Servais A, Wühl E, Niaudet P, Van’t Hoff W, Gahl W, Levtchenko E (2014) Nephropathic cystinosis: an international consensus document. Nephrol Dial Transplant 29(Suppl 4):iv87–iv94
Weber LT, Mehls O (2010) Limitations of dual x-ray absorptiometry in children with chronic kidney disease. Pediatr Nephrol 25(1):3–5
Denburg MR, Tsampalieros AK, de Boer IH, Shults J, Kalkwarf HJ, Zemel BS, Foerster D, Stokes D, Leonard MB (2013) Mineral metabolism and cortical volumetric bone mineral density in childhood chronic kidny disease. J Clin Endocrinol Metab 98(5):1930–1938
Acknowledgments
The authors would like to acknowledge Dr. Cécile Acquaviva-Bourdain (Département de Biologie, Hospices Civils de Lyon, France) for biochemical measurements and Mrs. Eurielle Bodenan (clinical research associate, CIC1407, Bron, France) for her help in data collection. They also would like to thank the patients and their families for being involved in clinical studies aiming at improving outcomes in nephropathic cystinosis.
Funding
The study was sponsored by Raptor/Horizon Pharmaceuticals.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
The study was approved by the local institutional review board (Comité de Protection des Personnes Lyon Sud Est II, initial approval of the Crystobs study 9/8/2010, approval of the 5th amendment 9/7/2016). Written informed consent was obtained from all patients (and parents in case of pediatric patients).
Conflict of interest
JB has received a travel grant from Raptor Pharmaceuticals and an educational research grant for this clinical study.
PC is a medical expert for Raptor Pharmaceuticals and co-investigator for the RP 103-3, 103-4, and 103-7 studies.
ABT is a medical expert for Raptor Pharmaceuticals and co-investigator for the RP 103-3, 103-4, and 103-7 studies.
MCS received travel grants from Amgen.
Rights and permissions
About this article
Cite this article
Bertholet-Thomas, A., Claramunt-Taberner, D., Gaillard, S. et al. Teenagers and young adults with nephropathic cystinosis display significant bone disease and cortical impairment. Pediatr Nephrol 33, 1165–1172 (2018). https://doi.org/10.1007/s00467-018-3902-x
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00467-018-3902-x