Abstract
Background
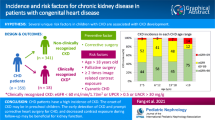
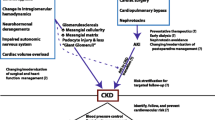
Cyanotic nephropathy (CN), seen in 30–50% of patients with congenital cyanotic heart disease (CCHD), affects both tubular and glomerular function, resulting in proteinuria and azotemia. Microalbuminuria is an early marker for glomerular damage and an independent predictor of progressive renal disease.
Methods
A cross-sectional study was conducted. A total of 116 patients aged 1 month to 15 years with CCHD at Chiang Mai University Hospital between 2015 and 2016 were assessed and 94 patients were enrolled. To determine the prevalence and associated factors of significant albuminuria in CCHD patients, baseline characteristics, oxygen saturation, surgery, hemoglobin (Hb), hematocrit (Hct), spot urine albumin, urine protein, and creatinine were obtained. Binary logistic-regression modeling was used to identify associated factors.
Results
Prevalence of CN in children with CCHD was 58.51% and 92.55% according to albuminuria and proteinuria staging respectively. Prevalence of significant proteinuria, significant albuminuria, and decreased GFR was 88.30%, 41.49% and 31.91% respectively. Participants with significant albuminuria had fewer previous surgeries (p = 0.05), a longer waiting time for surgery (p = 0.02), enalapril usage (p = 0.04), pulmonary hypertension (p = 0.03), higher Hct z-score (p = 0.03) and lower platelet count (p = 0.001) compared with those without significant albuminuria. Using multivariate logistic regression analysis, waiting duration for surgery (p = 0.04), Hct >40% (p = 0.02), and platelet count <290,000/mm3 (p = 0.04) were predictive of microalbuminuria.
Conclusions
Cyanotic nephropathy can be detected in the first decade of life with the presentation of microalbuminuria. High Hct level and low platelet count were identified as a predictor of microalbuminuria, whereas early cardiac surgery decreased the risk of developing significant albuminuria.

Similar content being viewed by others
References
Meessen H, Litton MA (1953) Morphology of the kidney in morbus caeruleus. AMA Arch Pathol 56:480–487
Dittrich S, Kurschat K, Lange PE (2001) Abnormal rheology in cyanotic congenital heart disease—a factor in non-immune nephropathy. Scand J Urol Nephrol 35:411–415
Agras PI, Derbent M, Ozcay F, Baskin E, Turkoglu S, Aldemir D, Tokel K, Saatci U (2005) Effect of congenital heart disease on renal function in childhood. Nephron Physiol 99:10–15
Zheng J, Yao Y, Han L, Xiao Y (2013) Renal function and injury in infants and young children with congenital heart disease. Pediatr Nephrol 28:99–104
Akita H, Matsuoka S, Kuroda Y (1993) Nephropathy in patients with cyanotic congenital heart disease. Tokushima J Exp Med 40:47–53
Inatomi J, Matsuoka K, Fujimaru R, Nakagawa A, Iijima K (2006) Mechanisms of development and progression of cyanotic nephropathy. Pediatr Nephrol 21:1440–1445
Dinneen SF, Gerstein HC (1997) The association of microalbuminuria and mortality in non-insulin-dependent diabetes mellitus. A systematic overview of the literature. Arch Intern Med 157:1413–1418
Wachtell K, Ibsen H, Olsen MH, Borch-Johnsen K, Lindholm LH, Mogensen CE, Dahlof B, Devereux RB, Beevers G, de Faire U, Fyhrquist F, Julius S, Kjeldsen SE, Kristianson K, Lederballe-Pedersen O, Nieminen MS, Okin PM, Omvik P, Oparil S, Wedel H, Snapinn SM, Aurup P (2003) Albuminuria and cardiovascular risk in hypertensive patients with left ventricular hypertrophy: the LIFE study. Ann Intern Med 139:901–906
Singh A, Satchell SC (2011) Microalbuminuria: causes and implications. Pediatr Nephrol 26:1957–1965
Flanagan MF, Hourihan M, Keane JF (1991) Incidence of renal dysfunction in adults with cyanotic congenital heart disease. Am J Cardiol 68:403–406
Fogo A, Hawkins EP, Berry PL, Glick AD, Chiang ML, MacDonell RC Jr, Ichikawa I (1990) Glomerular hypertrophy in minimal change disease predicts subsequent progression to focal glomerular sclerosis. Kidney Int 38:115–123
Spear GS (1960) Glomerular alterations in cyanotic congenital heart disease. Bull Johns Hopkins Hosp 106:347–367
Spear GS, Kihara I (1964) The glomerulus in cyanotic congenital heart disease: an immunofluorescent study. Bull Johns Hopkins Hosp 115:481–493
Kidney Disease: Improving Global Outcomes (KDIGO) CKD Work Group (2013) KDIGO 2012 clinical practice guideline for the evaluation and management of chronic kidney disease. Kidney Int Suppl 3:1–150
Schwartz GJ, Munoz A, Schneider MF, Mak RH, Kaskel F, Warady BA, Furth SL (2009) New equations to estimate GFR in children with CKD. J Am Soc Nephrol 20:629–637
Flegal KM, Cole TJ (2013) Construction of LMS parameters for the Centers for Disease Control and Prevention 2000 growth charts. Natl Health Stat Report (63):1–3
National High Blood Pressure Education Program Working Group on High Blood Pressure in Children and Adolescents (2004) The fourth report on the diagnosis, evaluation, and treatment of high blood pressure in children and adolescents. Pediatrics 114(2 Suppl 4th Report):555–576
Dallman P (1977) Blood and blood-forming tissue. In: Rudolph A (ed) Pediatrics. Appleton-Century-Crofts, Norwalk, CT
Galie N, Humbert M, Vachiery JL, Gibbs S, Lang I, Torbicki A, Simonneau G, Peacock A, Vonk Noordegraaf A, Beghetti M, Ghofrani A, Gomez Sanchez MA, Hansmann G, Klepetko W, Lancellotti P, Matucci M, McDonagh T, Pierard LA, Trindade PT, Zompatori M, Hoeper M, Aboyans V, Vaz Carneiro A, Achenbach S, Agewall S, Allanore Y, Asteggiano R, Paolo Badano L, Albert Barbera J, Bouvaist H, Bueno H, Byrne RA, Carerj S, Castro G, Erol C, Falk V, Funck-Brentano C, Gorenflo M, Granton J, Iung B, Kiely DG, Kirchhof P, Kjellstrom B, Landmesser U, Lekakis J, Lionis C, Lip GY, Orfanos SE, Park MH, Piepoli MF, Ponikowski P, Revel MP, Rigau D, Rosenkranz S, Voller H, Luis Zamorano J (2016) 2015 ESC/ERS Guidelines for the diagnosis and treatment of pulmonary hypertension: The Joint Task Force for the Diagnosis and Treatment of Pulmonary Hypertension of the European Society of Cardiology (ESC) and the European Respiratory Society (ERS): endorsed by: Association for European Paediatric and Congenital Cardiology (AEPC), International Society for Heart and Lung Transplantation (ISHLT). Eur Heart J 37:67–119
Krull F, Ehrich JH, Wurster U, Toel U, Rothganger S, Luhmer I (1991) Renal involvement in patients with congenital cyanotic heart disease. Acta Paediatr Scand 80:1214–1219
Birn H, Christensen EI (2006) Renal albumin absorption in physiology and pathology. Kidney Int 69:440–449
Dimopoulos K, Diller GP, Koltsida E, Pijuan-Domenech A, Papadopoulou SA, Babu-Narayan SV, Salukhe TV, Piepoli MF, Poole-Wilson PA, Best N, Francis DP, Gatzoulis MA (2008) Prevalence, predictors, and prognostic value of renal dysfunction in adults with congenital heart disease. Circulation 117:2320–2328
Eckardt KU, Hartmann W, Vetter U, Pohlandt F, Burghardt R, Kurtz A (1990) Serum immunoreactive erythropoietin of children in health and disease. Eur J Pediatr 149:459–464
Scott HW Jr, Elliott SR 2nd (1950) Renal hemodynamics in congenital cyanotic heart disease. Bull Johns Hopkins Hosp 86:58–71
Malizia E (1956) Renal function and hemodynamics in primary and secondary polycythemia. Acta Med Scand 154:399–406
Becker EL, Schilling JA, Harvey RB (1957) Renal function in man acclimatized to high altitude. J Appl Physiol 10:79–80
Dent GA, Herman JH, Siegel JE (2007) Laboratory hematology. In: Kahn MJ, Gregory SA (eds) American Society of Hematology self-assessment program. The American Society of Hematology, Washington, DC, pp 444–465
Takahashi S, Ooya K, Wada N, Inagaki T, Takana Y, Saito A, Nagata M, Harada K (2003) Partial exchange transfusion improved renal function and proteinuria in a patient with cyanotic heart disease nephropathy. Clin Nephrol 60:222–223
Omonuwa KO, Talwar A, Dedopoulos S, Mailloux LU (2009) Repeated phlebotomies improve and stabilise renal function in cyanotic nephropathy. BMJ Case Rep. https://doi.org/10.1136/bcr.10.2008.1084
Linderkamp O, Klose HJ, Betke K, Brodherr-Heberlein S, Buhlmeyer K, Kelson S, Sengespeik C (1979) Increased blood viscosity in patients with cyanotic congenital heart disease and iron deficiency. J Pediatr 95:567–569
Broberg CS, Bax BE, Okonko DO, Rampling MW, Bayne S, Harries C, Davidson SJ, Uebing A, Khan AA, Thein S, Gibbs JS, Burman J, Gatzoulis MA (2006) Blood viscosity and its relationship to iron deficiency, symptoms, and exercise capacity in adults with cyanotic congenital heart disease. J Am Coll Cardiol 48:356–365
Lill MC, Perloff JK, Child JS (2006) Pathogenesis of thrombocytopenia in cyanotic congenital heart disease. Am J Cardiol 98:254–258
Awad H, el-Safty I, Abdel-Gawad M, el-Said S (2003) Glomerular and tubular dysfunction in children with congenital cyanotic heart disease: effect of palliative surgery. Am J Med Sci 325:110–114
Passwell J, Orda S, Modan M, Shem-Tov A, Aladjem A, Boichis H (1976) Abnormal renal functions in cyanotic congenital heart disease. Arch Dis Child 51:803–805
Fine LG, Orphanides C, Norman JT (1998) Progressive renal disease: the chronic hypoxia hypothesis. Kidney Int Suppl 65:S74–S78
Ghafari S, Malaki M (2011) Truncus arteriosus: a major cause of proteinuria in children. J Cardiovasc Dis Res 2:237–240
Spear GS (1964) The glomerulus in cyanotic congenital heart disease and primary pulmonary hypertension. A review. Nephron 1:238–248
Hida K, Wada J, Yamasaki H, Nagake Y, Zhang H, Sugiyama H, Shikata K, Makino H (2002) Cyanotic congenital heart disease associated with glomerulomegaly and focal segmental glomerulosclerosis: remission of nephrotic syndrome with angiotensin converting enzyme inhibitor. Nephrol Dial Transplant 17:144–147
Fujimoto Y, Matsushima M, Tsuzuki K, Okada M, Shibata M, Yanase Y, Usui K, Nagashima M (2002) Nephropathy of cyanotic congenital heart disease: clinical characteristics and effectiveness of an angiotensin-converting enzyme inhibitor. Clin Nephrol 58:95–102
Filler G, Lipshultz SE (2012) Why multidisciplinary clinics should be the standard for treating chronic kidney disease. Pediatr Nephrol 27:1831–1834
Acknowledgements
This study was funded by the Faculty of Medicine, Chiang Mai University. The authors would like to thank the pediatric cardiology nurses for assistance with urine collection, and the children and parents who volunteered to participate in this study.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Informed consent
Written informed consent was obtained from all parents. The study has been approved by the Medical Ethics Committee of Chiang Mai University.
Conflicts of interest
The authors declare that there are no conflicts of interest regarding the publication of this paper.
Rights and permissions
About this article
Cite this article
Hongsawong, N., Khamdee, P., Silvilairat, S. et al. Prevalence and associated factors of renal dysfunction and proteinuria in cyanotic congenital heart disease. Pediatr Nephrol 33, 493–501 (2018). https://doi.org/10.1007/s00467-017-3804-3
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00467-017-3804-3