Abstract
Background
There are currently three distinct autosomal recessive inherited types of primary hyperoxaluria (PH: PHI, PHII, and PHIII), all characterized by the endogenous overproduction of oxalate. The PH type is difficult to differentiate by clinical features alone. In addition to universal general characteristics to all hyperoxaluria subtypes, specific urinary metabolites can be detected: glycolate in PHI, L-glyceric acid in PHII, and hydroxy-oxo-glutarate (HOG) in PHIII. PHIII is considered to be the most benign form and is characterized by severe recurrent urolithiasis in early life, followed by clinical remission in many, but not all patients. We examined urinary HOG (UHOG) excretion as a diagnostic marker and its correlation to progression of the clinical course of PHIII.
Methods
UHOG was analyzed by combined ion chromatography/mass spectrometry (IC/MS) in urine samples from 30 PHIII and 68 PHI/II patients and 79 non-PH hyperoxaluria patients.
Results
Mean UHOG excretion was significantly higher in patients with PHIII than in those with PHI/II and in non-PH patients(51.6 vs. 6.61 vs. 8.36 μmol/1.73 m2/24 h, respectively; p<0.01).
Conclusions
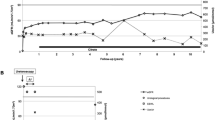
Significantly elevated UHOG excretion was exclusively seen in PHIII patients and showed a 100 % consensus with the results of hydroxy-oxo-glutarate aldolase (HOGA1) mutational analysis in newly diagnosed patients. However, UHOG excretion did not correlate with clinical course on follow-up and could not be used to discriminate between active stone formers and patients with a clinically uneventful follow-up.




Similar content being viewed by others
Change history
10 April 2018
The unit of the HOG-creatinine ratio presented in this article is calculated in μmol/mg creatinine instead of the demonstrated unit of μmol/μmol. This applies to the parameter in the text of the article and the labeling of Figs. 1, 2b and 3c.
References
Hoppe B, Beck BB, Milliner DS (2009) The primary hyperoxalurias. Kidney Int 75:1264–1271
Archer HE, Dormer AE, Scowen EF, Watts RW (1957) Primary hyperoxaluria. Lancet 273:320–322
Hoppe B (2012) An update on primary hyperoxaluria. Nat Rev Nephrol 8:467–475
Milliner DS, Harris PC, Lieske JC (2015) Primary hyperoxaluria type 3. In: Pagon RA, Adam MP, Ardinger HH, Wallace SE, Amemiya A, Bean LJH, Bird TD, Ledbetter N, Mefford HC, Smith RJH, Stephens K (eds) Gene reviews, University of Washington, Seattle
Cochat P, Rumsby G (2013) Primary hyperoxaluria. N Engl J Med 369:649–658
Monico CG, Rossetti S, Belostotsky R, Cogal AG, Herges RM, Seide BM, Olson JB, Bergstrahl EJ, Williams HJ, Haley WE, Frishberg Y, Milliner DS (2011) Primary hyperoxaluria type III gene HOGA1 (formerly DHDPSL) as a possible risk factor for idiopathic calcium oxalate urolithiasis. Clin J Am Soc Nephrol 6:2289–2295
Belostotsky R, Seboun E, Idelson GH, Milliner DS, Becker-Cohen R, Rinat C, Monico CG, Feinstein S, Ben-Shalom E, Magen D, Weissman I, Charon C, Frishberg Y (2010) Mutations in DHDPSL are responsible for primary hyperoxaluria type III. Am J Hum Genet 87:392–399
Beck BB, Baasner A, Buescher A, Habbig S, Reintjes N, Kemper MJ, Sikora P, Mache C, Pohl M, Stahl M, Toenshoff B, Pape L, Fehrenbach H, Jacob DE, Grohe B, Wolf MT, Nürnberg G, Yigit G, Salido EC, Hoppe B (2013) Novel findings in patients with primary hyperoxaluria type III and implications for advanced molecular testing strategies. Eur J Hum Genet 21:162–172
Belostotsky R, Pitt JJ, Frishberg Y (2012) Primary hyperoxaluria type III—a model for studying perturbations in glyoxylate metabolism. J Mol Med (Berl) 90:1497–1504
Hopp K, Cogal AG, Bergstralh EJ, Seide BM, Olson JB, Meek AM, Lieske JC, Milliner DS, Harris PC (2015) Rare kidney stone consortium phenotype-genotype correlations and estimated carrier frequencies of primary hyperoxaluria. J Am Soc Nephrol 26:2559–2570
Kemper MJ, Conrad S, Muller-Wiefel DE (1997) Primary hyperoxaluria type 2. Eur J Pediatr 156:509–512
Danpure CJ, Jennings PR, Watts RW (1987) Enzymological diagnosis of primary hyperoxaluria type 1 by measurement of hepatic alanine: glyoxylate aminotransferase activity. Lancet 1:289–291
Milliner DS, Wilson DM, Smith LH (2001) Phenotypic expression of primary hyperoxaluria: comparative features of types I and II. Kidney Int 59:31–36
Jacob DE, Grohe B, Geßner M, Beck BB, Hoppe B (2013) Kidney stones in primary hyperoxaluria: new lessons learnt. PLoS One 8:e70617
Pitt JJ, Willis F, Tzanakos N, Belostotsky R, Frishberg Y (2015) 4-hydroxyglutamate is a biomarker for primary hyperoxaluria type 3. JIMD Rep 15:1–6
Riedel TJ, Knight J, Murray MS, Milliner DS, Holmes RP, Lowther WT (2012) 4-Hydroxy-2-oxoglutarate aldolase inactivity in primary hyperoxaluria type 3 and glyoxylate reductase inhibition. Biochim Biophys Acta 1822:1544–1552
Toussaint C (1998) Pyridoxine-responsive PH1: treatment. J Nephrol 11[Suppl 1]:49–50
Milliner DS, Eickholt JT, Bergstralh EJ, Wilson DM, Smith LH (1994) Results of long-term treatment with orthophosphate and pyridoxine in patients with primary hyperoxaluria. N Engl J Med 331:1553–1558
Leumann E, Hoppe B, Neuhaus T (1993) Management of primary hyperoxaluria: efficacy of oral citrate administration. Pediatr Nephrol 7:207–211
Hamm LL (1990) Renal handling of citrate. Kidney Int 38:728–735
Allard L, Cochat P, Leclerc AL, Cachat F, Fichtner C, De Souza VC, Garcia CD, Camoin-Schweitzer MC, Macher MA, Acquaviva-Bourdain C, Bacchetta J (2015) Renal function can be impaired in children with primary hyperoxaluria type 3. Pediatr Nephrol 30:1807–1813
Zhao F, Bergstralh EJ, Mehta RA, Vaughan LE, Olson JB, Seide BM, Meek AM, Cogal AG, Lieske JC, Milliner DS (2016) Predictors of incident ESRD among patients with primary hyperoxaluria presenting prior to kidney failure. Clin J Am Soc Nephrol 11(1):119–126
Knight J, Jiang J, Assimos DG, Holmes RP (2006) Hydroxyproline ingestion and urinary oxalate and glycolate excretion. Kidney Int 70(11):1929–1934
Acknowledgments
We thank Przemyslaw Sikora (Lublin, Poland), Katarzyna Jobs (Warzaw, Poland), Marcin Zaniew, Lars Pape (Hannover, Germany), Burkhard Tönshoff (Heidelberg, Germany), Martin Bald (Stuttgart, Germany), Martin Pohl (Freiburg, Germany), Bärbel Lange-Sperandio (Munich, Germany), and Markus J. Kemper (Hamburg, Germany) for providing us with patient information and urine samples. We also thank B. Bär and D. Armborst (Germany) and F. Blanco (Spain) for extensive laboratory support. The work was partially supported by a grant from the German-Israeli Foundation (GIF) to (Bodo B. Beck & Bernd Hoppe)
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
This study was approved by the local ethics committee and all material was obtained after written informed consent.
Conflict of interest
The authors declare no conflict of interest.
Rights and permissions
About this article
Cite this article
Ventzke, A., Feldkötter, M., Wei, A. et al. Systematic assessment of urinary hydroxy-oxo-glutarate for diagnosis and follow-up of primary hyperoxaluria type III. Pediatr Nephrol 32, 2263–2271 (2017). https://doi.org/10.1007/s00467-017-3731-3
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00467-017-3731-3